What if we could forecast a health crisis with the same precision we predict the weather? This isn't science fiction; it's the monumental shift happening in medicine today. We're moving from a model of treating sickness as it arises to proactively preventing it from ever taking hold. The engine driving this change is predictive healthcare with AI, a field where data and algorithms work together to spot health risks before they become emergencies.
The Shift From Reactive to Predictive Medicine
For generations, healthcare has been fundamentally reactive. You feel sick, you see a doctor, you get a diagnosis, and then you start treatment. It’s a system that works, but it often means we’re intervening only after a disease has already established itself. Predictive healthcare completely flips that script. Think of it as a sophisticated early-warning system for the human body.

Instead of waiting for the fire alarm to blare, this approach listens for the faintest whispers of smoke. By crunching massive datasets, from electronic health records and genetic markers to real-time data from a smartwatch, AI algorithms can detect subtle patterns invisible to the human eye. This gives clinicians the power to identify patients at high risk for conditions like heart disease, diabetes, or even specific cancers, sometimes years before symptoms would ever appear.
Empowering Clinicians With Foresight
This isn't about replacing doctors. It's about augmenting their expertise with incredibly powerful tools. Imagine an AI as a brilliant medical assistant that never sleeps, constantly sifting through patient data to flag potential concerns for a doctor’s review. This frees up healthcare professionals to evolve from reactive problem-solvers into proactive health strategists.
A few of the biggest benefits of this shift are:
Personalised Prevention: We can finally move beyond generic, one-size-fits-all advice. Instead, we can create health plans tailored to a person's unique genetic and lifestyle risk factors.
Optimised Hospital Operations: Hospitals can better manage their resources by predicting patient admission surges or identifying individuals most likely to be readmitted after discharge.
Earlier Intervention: Pinpointing potential issues in their infancy means treatments are often far more effective and much less invasive.
Ultimately, the move toward predictive medicine empowers people to get ahead of future health challenges. It allows them to take meaningful, proactive steps, which often start with something as simple as comprehensive at-home health testing as an action plan for longevity.
This data-driven approach is already producing real-world results, improving patient outcomes and making the entire healthcare system more efficient. The integration of AI is making these advanced analytical tools more accessible, paving the way for a future where medicine is more personal, precise, and preventive. For a deeper dive into these advantages, check out our post on the benefits of AI in the healthcare industry: 7 Key Ways AI Improves Care
How Core AI Technologies Power Predictive Insights
To really get what’s happening inside predictive healthcare with AI, we need to peek under the bonnet and look at the technologies doing the heavy lifting. These aren't just abstract ideas; they are the digital engines crunching vast amounts of complex medical data to see what’s coming next for a patient's health. Each piece of technology has a distinct and crucial job to do.
Machine Learning: The Digital Diagnostician
Think of Machine Learning (ML) as the foundation of most predictive analytics. It's all about algorithms that learn from data without needing to be programmed for every single possibility.
Instead of following a rigid set of "if-then" rules, ML models get smarter and more accurate over time as they are fed more information. This adaptability is exactly what makes them so valuable for tasks like flagging patients who are likely to be readmitted to the hospital or even forecasting disease outbreaks across a community.
In healthcare, we primarily see two flavours of machine learning:
Supervised Learning: This is like teaching the AI with flashcards. The model is given data where the answer is already known (e.g., patient records clearly labelled "diabetic" or "non-diabetic"). It studies these examples to figure out the patterns, so it can make accurate predictions on new, unknown patient data.
Unsupervised Learning: Here, the AI is let loose on a pile of unlabelled data and told to find interesting patterns or groups on its own. It might discover clusters of patients with similar, previously unrecognized characteristics, potentially uncovering new risk factors that clinicians hadn't considered before.
This infographic shows just how much better these AI approaches are compared to traditional methods.
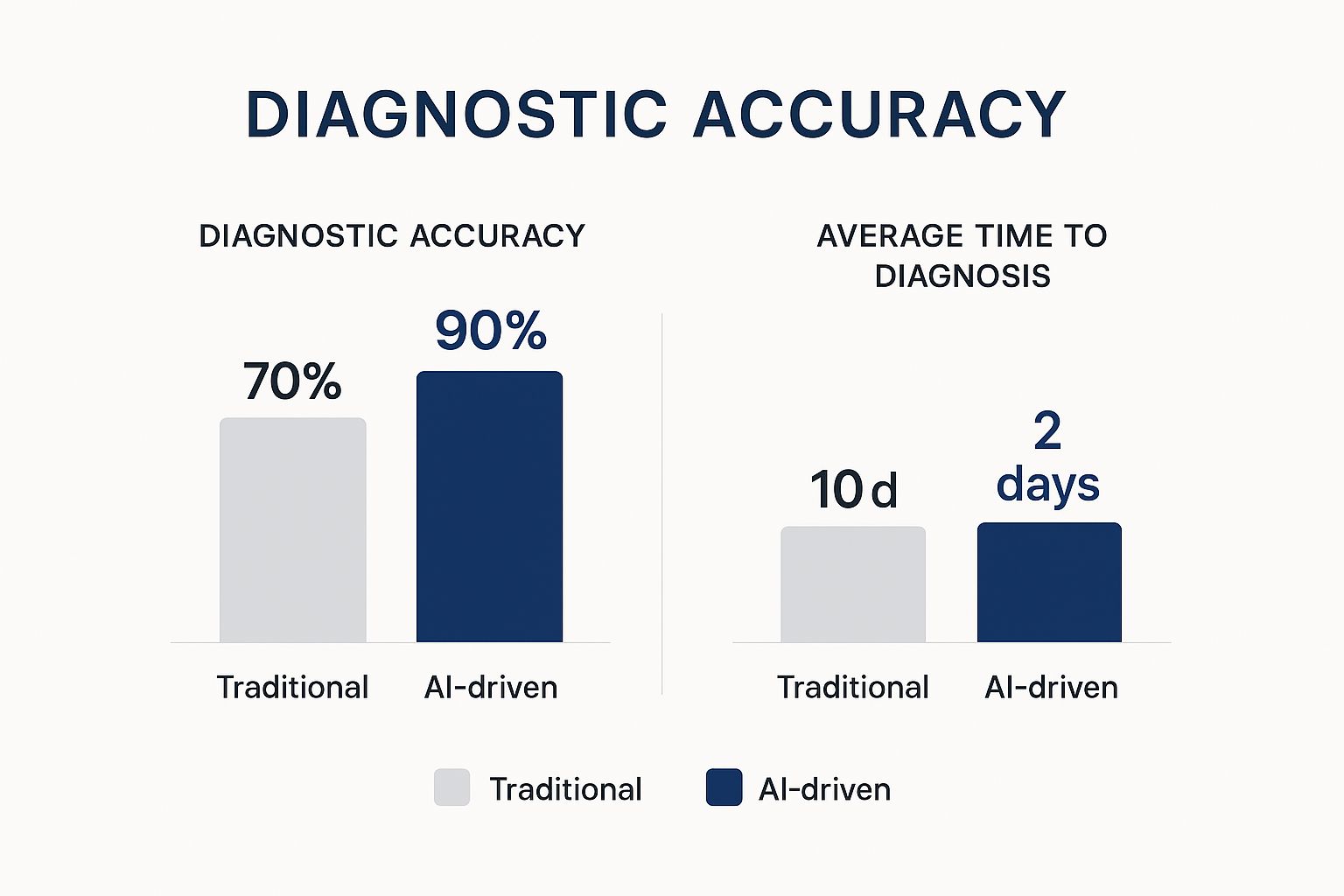
The numbers speak for themselves: a huge 20% jump in diagnostic accuracy and an 80% faster time-to-diagnosis. That's a direct, measurable improvement in both clinical workflow and patient outcomes.
Natural Language Processing: Decoding Clinical Notes
Next up is Natural Language Processing (NLP). Consider it the universal translator for medical information. So much vital patient data is stuck in unstructured text, such as doctors' notes, specialist reports, and patient feedback. NLP gives computers the power to read, understand, and make sense of all this human language.
NLP is the key that unlocks insights buried in text. It can scan millions of clinical notes to spot trends in patient-reported symptoms or track adverse drug reactions on a scale that would be impossible for any human team.
This technology is what turns messy, conversational text into clean, structured data points that machine learning models can actually use. For any hospital or clinic looking to tap into this goldmine of data, working with expert AI development Services is the best way to build a system that works.
Deep Learning: Seeing the Invisible
Finally, there's Deep Learning, which is a more advanced and powerful subset of machine learning. It functions like the highly trained eye of a seasoned specialist, using complex, multi-layered neural networks to analyze incredibly detailed data, like medical images.
A deep learning model can be trained to spot cancerous cells on a pathology slide or find tiny anomalies in an MRI scan that might otherwise be missed. Its knack for recognizing incredibly complex patterns in visual data has made it a game-changer in modern diagnostics, particularly in radiology and pathology.
Let's break down how these technologies fit together.
Key AI Technologies in Predictive Healthcare
AI Technology | Primary Function | Example Application |
|---|---|---|
Machine Learning (ML) | Learns from historical data to identify patterns and make predictions without being explicitly programmed. | Predicting patient readmission risk based on their electronic health record (EHR) data. |
Natural Language Processing (NLP) | Understands and extracts meaningful information from unstructured human language (text and speech). | Analyzing physicians’ notes to identify patients with undocumented symptoms or conditions. |
Deep Learning | A subset of ML that uses complex neural networks to analyze intricate data, especially images. | Detecting early signs of diabetic retinopathy from retinal scans, often with greater accuracy than the human eye. |
Each of these technologies brings a unique strength to the table. When combined, they provide a powerful toolkit for creating smarter Healthcare Tech Solutions that help push medicine from being reactive to truly proactive.
Real-World Clinical Applications of AI in Action
Technology is only as good as its real-world impact. When we talk about predictive healthcare with AI, we're not just discussing theories; we're seeing these tools make a difference in hospitals and clinics every day. This is where algorithms move from the lab to the patient’s bedside, becoming a crucial part of a clinician's toolkit.

One of the most profound applications is in catching life-threatening conditions early. Take sepsis, a notoriously fast-moving and deadly infection. AI models can now keep a constant watch on a patient's vitals and lab results, picking up on subtle patterns that signal the start of sepsis, often hours before a human might suspect a thing. That early warning gives medical teams a critical head start on treatment.
It’s a similar story with hospital readmissions. By analysing a patient’s health record, existing conditions, and even socioeconomic factors, AI can flag individuals who are at high risk of ending up back in the hospital after being discharged. This allows care teams to be proactive with follow-up calls or home health visits, helping to ensure a smoother, more permanent recovery.
From Diagnosis to Workflow Optimisation
Beyond just identifying high-risk patients, AI is fundamentally changing how we approach diagnostics. In fields like radiology and pathology, deep learning algorithms are now trained to review medical images with incredible precision. Think of it as a second set of expert eyes, highlighting suspicious areas on an MRI or pinpointing cancerous cells on a slide, helping specialists catch diseases earlier and with greater accuracy.
This isn't just happening in research labs. In California, where the global AI healthcare market is expected to reach $21.66 billion this year, these tools are already in busy clinical settings. In places like Santa Clarita, an estimated 90% of hospitals have brought AI on board, from LLM assistants that cut down on paperwork to predictive systems that speed up critical care. This practical integration is saving an average of 39 minutes in stroke treatment, a clear example of how AI delivers measurable improvements. You can find more details on this regional AI adoption on Nucamp.co.
Getting this kind of optimisation right is a core benefit of working with experienced AI Development Services that truly understand the unique pressures of the healthcare sector.
Personalising Treatment on a Mass Scale
Predictive AI is also unlocking the door to truly personalised medicine. By analysing a patient's genetic data right alongside their clinical history, AI models can help forecast how they'll respond to certain treatments. This is especially powerful in oncology, where AI can help doctors select the most effective chemotherapy based on a tumour's unique genetic signature.
Predictive analytics allows clinicians to move from a one-size-fits-all approach to a highly individualised treatment strategy, significantly improving the chances of a positive outcome for the patient.
This level of customisation was once impossible to do at scale. Now, these intelligent systems are making precision care a reality for more people than ever. For those curious about the first steps of implementing this technology, a clear strategy is essential, as we explored in our predictive healthcare with ai adoption guide.
Ultimately, these real-world examples show that AI is much more than a futuristic idea. It’s a practical, powerful tool that is already empowering clinicians, improving patient outcomes, and making our entire healthcare system more efficient. These are the kinds of forward-thinking Healthcare Tech Solutions that are shaping the future of medicine. To learn more about the team behind these innovations, feel free to explore our about us page.
Navigating the Hurdles of AI Implementation
For all its incredible promise, bringing predictive healthcare with AI into the real world is far from a simple plug-and-play operation. The journey from a promising algorithm to a trusted clinical tool is loaded with challenges. Getting it right means thinking far beyond the technology itself and tackling the messy, human side of the equation.

Right out of the gate, most healthcare organizations run into the data integration and quality problem. An AI model is a bit like a student; it can only ever be as smart as the material it studies. The trouble is, hospital data is often a tangled mess, locked away in different, aging IT systems. We're talking electronic health records, lab reports, and imaging archives that don't speak the same language. Pulling all that information together into a single, clean dataset is a massive, often underestimated, foundational step.
And of course, there are the massive ethical questions. Patient data privacy isn't just a goal; it's a fundamental requirement, demanding rock-solid cybersecurity and strict compliance with all regulations.
Overcoming Algorithmic Bias and Building Trust
One of the most serious ethical minefields is the risk of algorithmic bias. If an AI is trained on data that mostly comes from one demographic, it might make dangerously inaccurate predictions for everyone else. This isn't a hypothetical problem; it's a real threat that could make existing health disparities even worse. Fixing this means being incredibly deliberate about sourcing diverse data and constantly checking the model for fairness.
This ties directly into the "black box" dilemma. Many of the most powerful AI models can make startlingly accurate predictions, but how they get there is a mystery. For a doctor to confidently use an AI's recommendation, they need to understand its reasoning. You can't just expect a clinician to trust a recommendation that comes from a black box.
This critical need for clarity has spurred the growth of a whole new field: Explainable AI (XAI). The entire point of XAI is to build models that can justify their conclusions in plain language, building the confidence clinicians need to actually use them in their practice.
Tackling these complex issues is a core part of the discussion around the ethics of AI in healthcare, focusing on creating systems that are not only powerful but also transparent and fair.
The Role of Governance and Regulation
To keep everyone safe while this technology develops, we need clear rules of the road. Thoughtful regulatory frameworks can act as guardrails, guiding innovation without strangling it. This is where governance comes in, ensuring patient safety is always the top priority.
By addressing these hurdles with a clear strategy, healthcare organisations can finally begin to realize the full potential of predictive AI and build a future where technology truly improves patient care for everyone.
What's Next? Medicine’s Future with Next-Generation AI
As we look ahead, AI in healthcare is on the verge of a major shift. It's moving from being a handy tool to becoming a fundamental partner in medicine. The next wave of predictive healthcare with AI isn't just about tweaking current practices; it's about delivering a level of precision and personalisation that once felt like pure science fiction. We're graduating from predicting general risks to creating truly individualised medicine.
Think about treatments designed not just for a disease, but for a single person's unique genetic makeup. By weaving together genomic data, lifestyle details, and real-time health monitoring, AI will soon craft therapeutic plans tailored to one individual. This could mean knowing exactly how someone will react to a specific drug before they even take it, cutting out the guesswork and getting the best results from day one.
Building Fairness into the Code
A huge step forward is the push to create AI models that actively promote health equity. For too long, algorithms have risked amplifying the biases found in old medical data, often leaving vulnerable or minority groups behind. The future is all about building systems that don't just avoid these blind spots but actively seek them out and correct them.
A great example of this is happening at UC Davis Health in California. They developed an AI model called BE-FAIR, which was built from the ground up to reduce bias. It works by identifying at-risk patients from every demographic who could benefit from proactive care to stay out of the hospital. While around 65% of hospitals use predictive models, many of them unintentionally miss people in underserved communities. BE-FAIR’s approach makes sure that help gets to those who need it most, setting a new bar for what fair healthcare can look like. You can read the full research on how UC Davis Health uses AI to leave no patient behind.
This focus on fairness is a core principle for the next generation of AI Development Services, making sure that technology works for everyone, not just a select few.
Speeding Up Drug Discovery and Clinical Trials
Another area where AI is set to make a massive impact is in pharmaceutical research. Finding and testing new drugs is a notoriously slow and costly marathon, often taking more than a decade and costing billions. AI is poised to change that timeline completely.
Sophisticated algorithms can now sift through massive biological datasets to pinpoint promising drug targets at incredible speeds. They can even predict how effective a new compound might be and what side effects it might have long before it gets to a lab, saving an enormous amount of time and money.
It's not just about finding new drug candidates, either. AI is also streamlining the entire clinical trial process. By analysing patient data, it can help researchers design smarter trials and find the best participants, making studies faster and far more likely to produce clear results.
This kind of acceleration is a game-changer. It means life-saving medications could get to the people who need them years sooner than they do today.
AI as a True Clinical Partner
When you boil it all down, the future of medicine is about collaboration. AI won't replace doctors; it will become their indispensable partner. By taking on the heavy lifting of complex data analysis and offering predictive insights, AI will free up clinicians to concentrate on what they do best: delivering compassionate, human-to-human care. This teamwork will lead to smarter, fairer, and more effective Healthcare Tech Solutions for all of us.
Getting there requires a deep appreciation for both technology and medicine. As we build this future, working with experts who truly understand this intersection is key. To see the team committed to this mission, we invite you to get to know us on our about us page. The evolution of healthcare is already underway, powered by intelligent, equitable, and forward-thinking AI.
Building a Healthier Future Through Partnership
Building an intelligent healthcare system isn't a solo mission; it's a team sport. Throughout this guide, we've seen how the incredible potential of predictive healthcare with AI comes to life when technology experts, clinical professionals, and healthcare leaders work together. This is the synergy that transforms a promising algorithm into a tool that can actually save lives.
Successfully putting these systems into practice takes more than just good code. It requires a deep understanding of clinical workflows, a firm commitment to ethical standards, and a shared vision for making healthcare more proactive and personal. The real magic happens when data science insights are paired with the hands-on expertise of doctors and nurses.
Finding the Right Partner for Your AI Journey
For any healthcare organization looking to step into this future, the first move is often finding the right partner. The best partners don't just bring technical skills to the table; they have a genuine respect for the unique challenges of medicine. This is crucial for building solutions that are both powerful and practical.
The goal is to build a system where AI supports human expertise, freeing clinicians to focus on what they do best: care for the patient. This collaborative approach ensures that technology serves medicine, not the other way around.
As we've seen, the benefits are huge, from catching diseases earlier to making hospitals run more smoothly. A strategic partnership helps you navigate the tricky parts, like data integration, model validation, and ethical oversight, ensuring the whole process is successful. This is the foundation of effective predictive healthcare with AI.
This guide has shown that predictive AI isn't some far-off concept; it's here now, creating real value in modern medicine. Expert AI Development Services can help your organisation identify the precise problems these tools are ready to solve. Crafting smarter Healthcare Tech Solutions is a journey built on partnership and shared goals. To learn more about our team and how we approach this mission, we invite you to get to know us on our about us page.
Your Questions About AI in Healthcare, Answered
As AI continues to make its way into medicine, it’s only natural to have questions. Let's tackle some of the most common ones to demystify how these tools are improving patient care.
How Accurate Are AI Predictive Models in Healthcare?
They can be incredibly accurate, often spotting patterns that traditional methods might miss. But that accuracy really depends on a few key things: the quality and quantity of the data it learns from, the specific algorithm used, and how complex the medical issue is.
It’s important to remember that AI isn't a crystal ball. Think of it more like a highly advanced assistant for clinicians. Its job is to provide insights and support a doctor's expertise, not to make final decisions on its own. Every reliable system has strong oversight, meaning models are constantly checked and validated by human experts before they ever influence patient care.
Will AI Replace Doctors and Other Healthcare Professionals?
Not at all. The goal is to empower healthcare professionals, not replace them. AI is fantastic at sifting through massive amounts of data and handling repetitive tasks, work that often bogs clinicians down.
By taking on that heavy lifting, AI frees up doctors and nurses to focus on what they do best: navigating complex medical decisions, connecting with patients, and delivering compassionate, human-centred care. It's about giving them better tools to make more informed decisions, helping them become even more effective at their jobs.
How Is Patient Data Kept Private and Secure?
Protecting patient data is non-negotiable. Security is built in from the ground up, starting with strict compliance with regulations like HIPAA.
Beyond that, techniques like data anonymization are used to strip away personal identifiers before the information is even fed into a model. This protects privacy right from the start. Access to any sensitive data is tightly restricted and regularly audited to ensure everything is secure and trustworthy.
What is the First Step to Implement Predictive AI?
For any hospital or clinic, the best first step is to pick a clear, specific problem you want to solve. Don't try to boil the ocean. A great starting point could be something with a measurable impact, like reducing patient readmission rates or predicting the early onset of sepsis.
Once you have a target, the next move is to look at your data. Is it clean, accessible, and ready to use? You'll also need a solid governance plan. Partnering with specialists who understand both AI and healthcare can make these initial stages much smoother. For more on this topic, you can find a wealth of information and ongoing discussions on platforms offering additional insights and discussions on AI in healthcare.
At Cleffex, we are dedicated to navigating this exciting frontier. Our team combines deep technical expertise with a genuine understanding of clinical needs to build solutions that are not only powerful but also practical and ethical. To learn more about our mission and the team driving these advancements, please visit our about us page.







