The healthcare landscape is undergoing a profound transformation, moving from reactive treatments to proactive, predictive, and personalized care. At the heart of this revolution is Artificial Intelligence (AI). Once a concept confined to science fiction, AI is now an indispensable tool that is enhancing nearly every facet of the medical field. From diagnosing diseases with unprecedented accuracy to streamlining complex administrative tasks, the applications are both vast and impactful. In Canada and across the globe, healthcare organisations are leveraging AI to solve long-standing challenges, improve patient outcomes, and create more efficient, sustainable systems.
This shift extends even to consumer technology, where personal devices now play a crucial role in preventative health. The integration of AI-powered features into everyday gadgets highlights this trend, offering new ways to monitor well-being. For medical professionals seeking to understand these developments, resources like a cardiologist’s guide to smartwatch ECGs provide essential perspectives on how consumer-grade devices intersect with clinical practice. This convergence underscores the broad impact of intelligent systems.
This article will delve into the seven most significant benefits of AI in healthcare industry, exploring the specific technologies, real-world examples, and actionable insights that demonstrate how intelligent systems are not just augmenting human capabilities but fundamentally redefining the future of medicine. We will examine how these advancements are powered by innovative software solutions that drive progress in healthcare applications, making intelligent medicine a present-day reality. Get ready to explore how AI is making healthcare smarter, faster, and more effective for everyone.
1. Enhanced Medical Imaging and Diagnostics
One of the most transformative benefits of AI in the healthcare industry is its profound impact on medical imaging and diagnostics. AI-powered tools can analyse complex medical images, such as X-rays, CT scans, and MRIs, with a level of precision and speed that complements, and in some cases surpasses, human capabilities. These systems leverage sophisticated machine learning algorithms, particularly deep learning, to identify subtle patterns, anomalies, and early-stage disease indicators that might be imperceptible to the human eye.
This technology represents a paradigm shift from traditional diagnostic methods. Instead of relying solely on a radiologist’s experience, AI introduces a data-driven layer of analysis, trained on millions of annotated images. This allows for the rapid detection of conditions like cancerous tumours, diabetic retinopathy, cardiovascular abnormalities, and neurological disorders, often at their earliest and most treatable stages.
How it Works in Practice
The implementation of AI in diagnostics involves several key stages. First, a vast and diverse dataset of medical images is curated and meticulously labelled by clinical experts. An AI model, typically a convolutional neural network (CNN), is then trained on this data to recognise specific features associated with various diseases. Once validated, this model can be integrated into a hospital’s Picture Archiving and Communication System (PACS) or a radiologist’s workflow, providing real-time analysis and flagging suspicious areas for human review.
Leading organisations have demonstrated remarkable success with this approach. For example, Google’s DeepMind AI can detect over 50 sight-threatening eye diseases from optical coherence tomography (OCT) scans with an accuracy rivalling top specialists. Similarly, platforms like PathAI are enhancing the accuracy of cancer pathology by helping pathologists identify malignant cells in tissue samples with greater consistency, directly impacting treatment decisions.
Actionable Implementation Strategy
For healthcare organisations looking to adopt this technology, a strategic approach is essential:
- Start with High-Volume Areas: Begin implementation with standardized, high-volume imaging procedures like chest X-rays or mammograms to maximise initial impact and streamline workflow integration.
- Prioritise Diverse Datasets: Ensure the AI models are trained on diverse patient data, including various ethnicities, ages, and genders, to prevent algorithmic bias and ensure equitable diagnostic accuracy.
- Maintain a Human-in-the-Loop System: Implement AI as an assistive tool, not a replacement. A radiologist’s final review and oversight remain crucial for quality assurance, ethical considerations, and handling complex, atypical cases.
The following chart illustrates the quantitative improvements AI brings to the diagnostic process, showcasing significant gains in accuracy, error reduction, and speed.
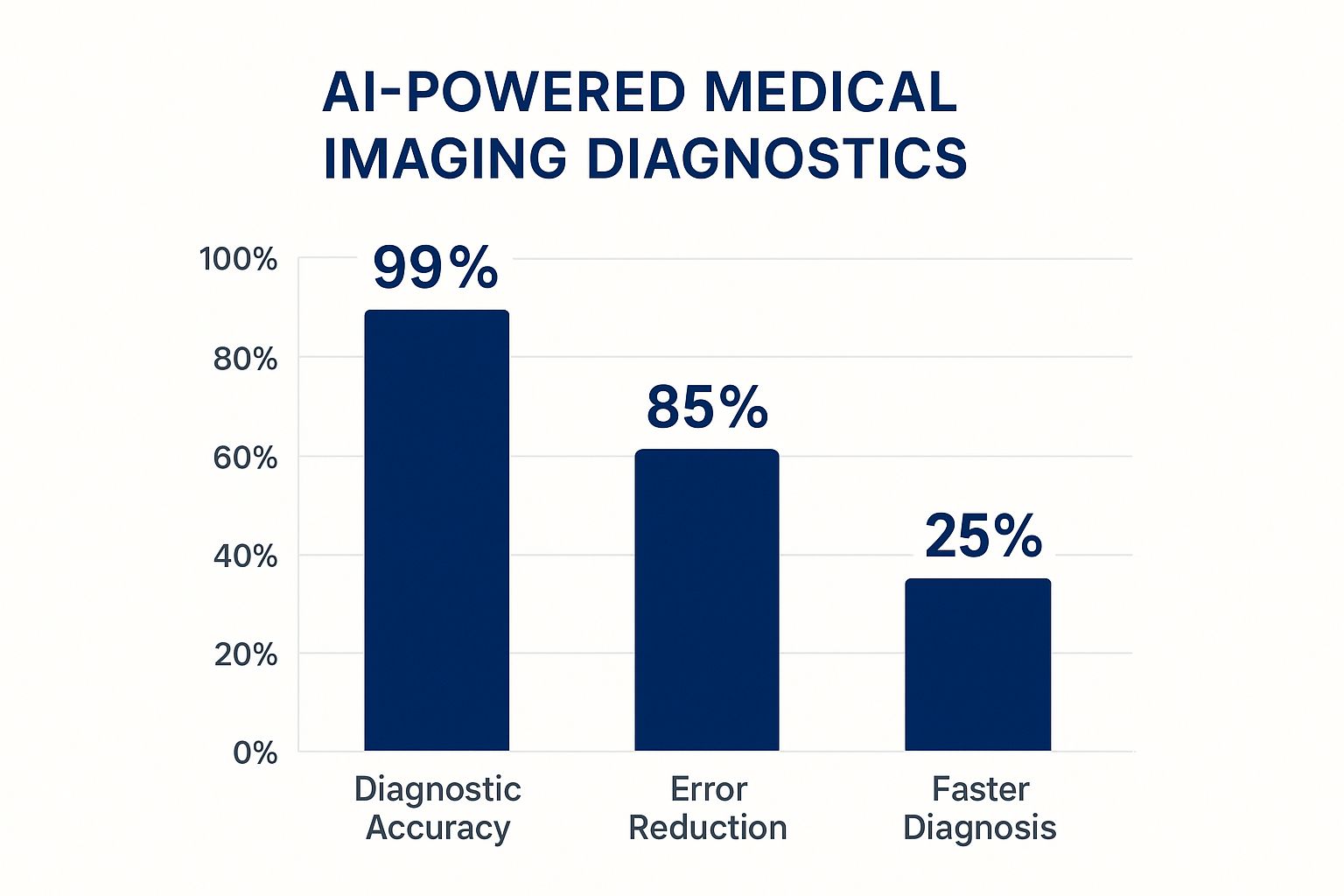
As the data clearly shows, AI integration can lead to near-perfect diagnostic accuracy while substantially reducing errors and accelerating the time to diagnosis. This efficiency allows clinicians to focus on patient care and treatment planning, fundamentally improving healthcare outcomes.
2. Precision Medicine and Personalized Treatment
Another significant benefit of AI in the healthcare industry is its central role in advancing precision medicine and creating personalized treatment plans. AI algorithms can sift through massive, complex datasets, including a patient’s genetic makeup, lifestyle factors, medical history, and environmental influences. This analysis allows for a shift away from the traditional one-size-fits-all medical model towards highly targeted therapies tailored to the individual. The result is more effective treatments with fewer adverse side effects, optimising patient outcomes.
This data-driven approach allows clinicians to predict which treatment and prevention strategies will be most effective for specific groups of people. By understanding a patient’s unique molecular profile, healthcare providers can select therapies that are most likely to succeed, avoid those that will be ineffective, and anticipate potential complications before they arise. It represents a more proactive, predictive, and participatory model of patient care.

How it Works in Practice
The practical application of AI in precision medicine begins with data aggregation. AI platforms consolidate information from diverse sources, such as genomic sequencing, electronic health records (EHRs), and real-time monitoring devices. Sophisticated machine learning models then analyze this data to identify correlations between a patient’s specific biological markers and their potential response to various therapies.
Prominent organizations are already demonstrating the power of this approach. For example, Tempus uses AI to analyse clinical and molecular data to help oncologists make personalized treatment decisions for cancer patients. Similarly, IBM Watson for Oncology cross-references patient data against a vast database of medical literature and clinical trials to provide evidence-based treatment recommendations. These tools empower clinicians with deeper insights, enabling them to devise treatment strategies with a much higher probability of success.
Actionable Implementation Strategy
For healthcare providers and organizations aiming to leverage AI for personalized treatment, a structured implementation plan is key:
- Build Comprehensive Patient Data Repositories: Start by creating a secure and integrated data infrastructure that can consolidate genomic, clinical, and lifestyle data into a unified patient profile.
- Partner with Genomic Testing Laboratories: Collaborate with specialised labs like Foundation Medicine to gain access to comprehensive genomic profiling, providing the foundational data needed for AI analysis. To understand more about this integration, learn more about AI helping the healthcare industry on cleffex.com.
- Invest in Genetic Counselling Capabilities: As genetic data becomes a standard part of patient care, it is crucial to have trained professionals who can interpret results and communicate complex information effectively to patients.
- Ensure Robust Consent and Data Privacy: Implement clear protocols for patient consent and adhere to stringent data privacy and security standards to build trust and ensure regulatory compliance.
3. Drug Discovery and Development Acceleration
Another of the core benefits of AI in the healthcare industry is its ability to radically accelerate the traditionally slow and costly process of drug discovery and development. AI models can analyze vast biological datasets to predict how molecules will behave, identify promising drug compounds, and even forecast potential side effects, condensing a process that often takes over a decade and billions of dollars into a much shorter and more cost-effective timeline.
This technology represents a monumental leap forward from conventional trial-and-error laboratory methods. By leveraging machine learning to simulate complex biological interactions, researchers can de-risk the development pipeline, focusing resources only on the most viable candidates. This data-driven approach allows for the rapid identification of novel therapies for diseases ranging from cancer to rare genetic disorders, significantly shortening the path from laboratory to patient.
How it Works in Practice
The practical application of AI in pharmacology is multifaceted. It begins with generative AI models creating novel molecular structures with desired properties or screening immense virtual libraries of existing compounds to find matches for a specific disease target. For instance, AI can predict a protein’s 3D structure from its amino acid sequence, a critical step in designing drugs that bind to it effectively. These predictions are then used to guide laboratory experiments, optimising clinical trial design by selecting patient populations most likely to respond to a new therapy.
Pioneering organisations are already showcasing the transformative potential of this technology. DeepMind’s AlphaFold has revolutionised structural biology by predicting protein structures with unprecedented accuracy. Similarly, companies like Insilico Medicine and Recursion Pharmaceuticals use end-to-end AI platforms to identify novel disease targets and design new drug candidates for conditions like idiopathic pulmonary fibrosis and various cancers, moving compounds from discovery to clinical trials in record time.
Actionable Implementation Strategy
For pharmaceutical and biotech firms aiming to integrate AI into their research and development, a focused strategy is key:
- Focus on Well-Characterised Disease Areas Initially: Start with diseases that have abundant, high-quality biological and clinical data to train and validate AI models effectively before tackling more complex or data-scarce conditions.
- Invest in High-Quality Data Curation: The success of any AI model is contingent on the data it’s trained on. Establish robust processes for cleaning, standardising, and annotating diverse datasets (genomic, proteomic, clinical) to ensure model accuracy and reliability.
- Collaborate with Academic and Research Institutions: Partner with universities and research centres to gain access to cutting-edge algorithms, specialised expertise, and novel datasets, fostering an ecosystem of innovation.
- Maintain Partnerships with Regulatory Bodies: Engage with regulatory agencies like Health Canada or the FDA early and often to ensure AI-driven discovery and trial design methodologies align with approval standards, smoothing the path to market.
4. Predictive Analytics and Early Warning Systems
Another of the core benefits of AI in the healthcare industry is the power of predictive analytics to create sophisticated early warning systems. These AI-driven tools continuously analyse vast streams of patient data, including real-time vital signs, lab results, and information from electronic health records (EHRs). By identifying subtle patterns and correlations invisible to human observers, these systems can predict the likelihood of adverse events hours or even days before they happen.
This technology marks a crucial shift from reactive to proactive care. Instead of responding to a crisis after a patient has already deteriorated, clinicians receive advance notice, allowing them to intervene preventively. This capability is instrumental in identifying patients at high risk for sepsis, cardiac arrest, acute kidney injury, or hospital readmissions, enabling timely and life-saving interventions.
How it Works in Practice
The implementation of predictive analytics involves creating and training machine learning models on extensive historical patient datasets. These models learn the complex combination of factors that often precede a specific adverse event. Once deployed, the AI runs in the background, continuously monitoring incoming data from connected devices and EHRs for at-risk patients. When the system’s algorithm detects a pattern indicating a high probability of a future event, it generates an alert for the clinical care team.
Renowned institutions have pioneered this approach with significant success. For instance, Johns Hopkins developed the Targeted Real-time Early Warning System (TREWS), which uses AI to screen patients for sepsis and has been shown to reduce mortality rates. Similarly, Epic Systems Corporation’s Deterioration Index is integrated into its EHR to provide a predictive score for patient decline, while Philips’ IntelliVue Guardian Solution offers a similar early warning capability for general hospital wards.
Actionable Implementation Strategy
For healthcare providers aiming to leverage this technology, a phased and strategic implementation is key:
- Start with High-Impact Conditions: Focus initial efforts on well-defined, high-risk conditions like sepsis or hospital-acquired infections where early intervention has a proven, significant impact on patient outcomes.
- Establish Clear Alert Protocols: Implement robust alert management protocols to prevent “alert fatigue.” This includes defining who receives alerts, what the immediate next steps are, and how to escalate responses effectively.
- Invest in Staff Training: Ensure clinical staff are thoroughly trained on how to interpret the system’s predictions and respond appropriately. This builds trust in the technology and ensures it is used to its full potential.
By forecasting patient deterioration, these systems empower clinical teams to act decisively, significantly improving patient safety and reducing the costs associated with emergency interventions and prolonged hospital stays. You can learn more about how AI models are being trained for these tasks and their impact by exploring detailed resources on artificial intelligence in healthcare.
5. Robotic Surgery and Surgical Assistance
Another of the most impactful benefits of AI in the healthcare industry is its integration into robotic surgery, creating systems that provide surgeons with unparalleled precision and control. AI-enhanced robotics augment a surgeon’s abilities by eliminating natural hand tremors, improving dexterity, and offering magnified 3D visualization of the surgical site. This fusion of human expertise and machine accuracy enables complex, minimally invasive procedures to be performed with greater safety and efficacy than ever before.

This technology revolutionizes the operating theatre. Rather than relying on traditional open surgery or standard laparoscopy, AI-powered systems allow surgeons to operate through tiny incisions with enhanced agility and range of motion. The AI component can also provide real-time data analysis and haptic feedback, guiding the surgeon’s movements and helping to identify critical anatomical structures. This leads to reduced blood loss, less post-operative pain, shorter hospital stays, and significantly faster recovery times for patients.
How it Works in Practice
During a robotic-assisted procedure, the surgeon operates from a console, typically located in the same room, which provides a high-definition, 3D view of the surgical area. The surgeon’s hand and wrist movements are translated by the AI-driven system into precise, real-time movements of miniaturized instruments attached to the robotic arms. The system’s algorithms filter out tremors and scale movements, allowing for delicate manoeuvres that would be impossible for the human hand alone.
Pioneered by systems like Intuitive Surgical’s da Vinci platform, this field has expanded to include advanced technologies like Medtronic’s Hugo and CMR Surgical’s Versius system. These platforms are used across various specialities, including urology, gynaecology, and general surgery, for procedures ranging from prostatectomies to complex cardiac valve repairs. Dr. Mani Menon, a pioneer in the field, demonstrated how this technology could dramatically improve patient outcomes, popularizing its adoption worldwide.
Actionable Implementation Strategy
For healthcare facilities aiming to integrate robotic surgery, a structured implementation is key to success:
- Invest in Comprehensive Surgeon Training: Develop robust, hands-on training and credentialing programs. Ensure surgical teams are proficient not just with the technology, but also with team communication in a robotic surgery environment.
- Start with High-Volume, Standardized Procedures: Begin with common, well-established procedures like cholecystectomies or hysterectomies. This allows the surgical team to build experience and refine workflows before tackling more complex cases.
- Develop Backup Protocols for System Failures: Establish clear, rehearsed protocols for potential technical malfunctions or power outages. This includes knowing how to quickly convert to a traditional laparoscopic or open procedure to ensure patient safety is never compromised.
- Monitor Outcomes Data Continuously: Track key performance indicators such as operative time, complication rates, and patient recovery metrics. Use this data to continuously improve techniques, optimize system use, and demonstrate the value of the investment.
6. Clinical Decision Support and Treatment Recommendations
Another of the core benefits of AI in the healthcare industry is its ability to power advanced Clinical Decision Support (CDS) systems. These sophisticated tools act as intelligent co-pilots for clinicians, analysing vast datasets in real-time to provide evidence-based recommendations, diagnostic suggestions, and crucial safety alerts. By synthesising patient data with the latest medical literature and clinical guidelines, AI-driven CDS helps standardise care, reduce medical errors, and guide practitioners toward the most effective treatment pathways.
This technology enhances a clinician’s expertise rather than replacing it. It processes complex variables, such as a patient’s electronic health record, genomic data, and lab results, and cross-references them against established protocols. The system can flag potential drug-to-drug interactions, predict the risk of sepsis, or suggest personalised treatment plans, empowering healthcare providers to make more informed decisions at the point of care.
How it Works in Practice
AI-powered CDS systems are integrated directly into a hospital’s electronic health record (EHR) workflow. Using machine learning models, these systems continuously learn from new data, refining their predictive accuracy and recommendations over time. The synergy between knowledge management and artificial intelligence is pivotal here, allowing healthcare professionals to quickly access and apply vast amounts of information for accurate clinical support. When a physician enters patient information, the AI engine analyses it in the background and presents relevant, context-aware alerts and suggestions without disrupting the clinical workflow.
Prominent examples demonstrate the impact of this technology. Epic Systems’ sepsis and deterioration prediction models are widely used to provide early warnings, enabling timely intervention. Similarly, IBM Watson for Oncology assists oncologists by analysing patient data against a massive database of research and clinical trials to recommend personalised cancer treatment options. These tools translate complex data into actionable clinical intelligence.
Actionable Implementation Strategy
For healthcare organisations aiming to integrate AI-driven CDS, a phased and strategic approach is vital:
- Customise Alerts to Reduce Fatigue: Work with clinical teams to configure system alerts and notifications. Over-alerting can lead to “notification fatigue,” so it’s crucial to prioritise high-risk scenarios and make suggestions contextually relevant.
- Train Staff on Proper Utilisation: Provide comprehensive training to ensure clinicians understand how the system works, trust its recommendations, and know how to use its insights to complement their own clinical judgment.
- Regularly Update Knowledge Bases: The AI’s effectiveness depends on the quality and currency of its data. Establish a clear process for continuously updating the system with the latest evidence-based guidelines, medical research, and pharmaceutical information.
7. Administrative Workflow Automation
One of the most immediate and impactful benefits of AI in the healthcare industry is its ability to automate and streamline burdensome administrative workflows. AI-powered systems can handle a vast array of repetitive, rules-based tasks, from appointment scheduling and insurance verification to medical coding and billing, freeing up invaluable time for healthcare professionals to focus on direct patient care. This technology uses a combination of natural language processing (NLP), machine learning (ML), and robotic process automation (RPA) to bring new levels of efficiency to the operational backbone of healthcare.
This represents a crucial shift away from manual processes that are often slow, prone to error, and costly. Instead of staff spending hours on data entry or sifting through paperwork, AI introduces an intelligent layer of automation that operates with speed and precision. This not only reduces operational overhead but also minimizes the risk of costly billing errors, improves revenue cycle management, and ultimately enhances the patient experience by reducing wait times and administrative hurdles.
How it Works in Practice
The implementation of AI in administrative workflows involves deploying intelligent systems to manage specific tasks. For example, NLP algorithms can transcribe and structure clinical notes dictated by physicians, automatically extracting relevant information for electronic health records (EHRs) and billing. Beyond clinical applications, AI streamlines various back-office tasks. For instance, understanding why healthcare facilities are transitioning to digital check-in systems reveals how automation is transforming the patient journey from the moment they arrive.
Leading technology providers have made significant strides in this area. Nuance’s Dragon Medical One uses speech recognition to help clinicians capture patient stories accurately and efficiently within the EHR. Platforms like Olive AI and UiPath deploy “digital workers” or bots that automate tasks like prior authorisation, claim processing, and patient intake, integrating seamlessly with existing hospital information systems. Similarly, Amazon Transcribe Medical offers highly accurate, real-time transcription services tailored for clinical documentation. These examples highlight how the right custom medical software development can integrate AI to solve specific administrative challenges.
Actionable Implementation Strategy
For healthcare organisations aiming to leverage administrative automation, a phased and strategic approach is vital:
- Target High-Volume, Repetitive Processes: Begin by identifying and automating tasks that are rules-based, high-volume, and time-consuming, such as appointment reminders, data entry, or initial insurance eligibility checks. This ensures a quick and measurable return on investment.
- Prioritise Staff Training and Change Management: Proactively communicate the benefits of automation to staff, framing it as a tool to reduce mundane work, not replace jobs. Provide comprehensive training to ensure a smooth transition and encourage adoption.
- Implement a Gradual Rollout with Monitoring: Start with a pilot program in a single department to test the technology and measure its impact. Monitor key performance indicators like processing times, error rates, and staff satisfaction before scaling the solution across the organisation.
- Maintain Human Oversight for Quality Control: While AI excels at routine tasks, human oversight remains essential for handling exceptions, resolving complex issues, and ensuring quality assurance, particularly in critical areas like medical billing and coding.
Benefits Comparison of 7 AI Healthcare Applications
| Item | Implementation Complexity | Resource Requirements | Expected Outcomes | Ideal Use Cases | Key Advantages |
|---|---|---|---|---|---|
| Enhanced Medical Imaging and Diagnostics | High – requires large datasets and regulatory approval | Extensive labeled imaging data, integration with PACS | 99%+ accuracy, 85% error reduction, faster diagnosis | Radiology, urgent diagnostic imaging | Superhuman accuracy, 24/7 availability, early detection |
| Precision Medicine and Personalized Treatment | Moderate to High – data integration and genomic analysis | Comprehensive patient data, genetic testing facilities | Up to 40% improved treatment efficacy, fewer side effects | Oncology, tailored therapies | Personalized treatments, reduced adverse reactions |
| Drug Discovery and Development Acceleration | High-complex modeling and simulations | High computational power, curated molecular databases | Up to 70% cost reduction, 5-10 years faster development | Pharmaceutical R&D | Accelerated drug discovery, cost savings |
| Predictive Analytics and Early Warning Systems | Moderate – continuous data monitoring and model updates | Real-time patient data streams, EHR integration | 18% mortality reduction, 25-30% fewer readmissions | ICU, patient monitoring | Proactive interventions, improved patient safety |
| Robotic Surgery and Surgical Assistance | Very High – expensive hardware and surgeon training | High-cost robotic systems, trained personnel | 40-50% fewer complications, faster recovery | Complex surgeries, minimally invasive | Enhanced precision, reduced surgeon fatigue |
| Clinical Decision Support and Treatment Recommendations | Moderate – integration with EHR and knowledge bases | Updated clinical data and guidelines databases | 15-25% reduction in errors, improved guideline adherence | Routine clinical decision making | Error reduction, standardized care, support clinicians |
| Administrative Workflow Automation | Moderate – process redesign and system integration | NLP tools, RPA software, staff training | 30-50% cost reduction, saves 2-3 hours daily | Scheduling, billing, and documentation | Increased efficiency, reduced manual tasks |
Embracing the Future: Integrating AI into Healthcare’s Core
The journey through the myriad applications of artificial intelligence in medicine paints a clear and compelling picture. The benefits of AI in the healthcare industry are not distant promises but tangible realities actively reshaping patient care, operational efficiency, and medical innovation. We have explored how AI-powered algorithms are sharpening the accuracy of medical imaging, leading to earlier and more precise diagnoses than ever before. This leap forward is saving lives by catching diseases like cancer in their nascent stages, providing a crucial advantage in treatment.
Furthermore, the shift towards precision medicine, fuelled by AI’s ability to analyse complex genomic and lifestyle data, is moving us away from one-size-fits-all treatments. This personalised approach ensures that therapies are tailored to an individual’s unique biological makeup, maximising efficacy while minimising adverse effects. We have also seen how AI drastically accelerates the timeline for drug discovery and development, a process that once took decades and billions of dollars. By simulating molecular interactions and identifying promising compounds, AI is bringing new hope and novel treatments to patients faster.
From Reactive to Proactive Healthcare
One of the most profound shifts driven by AI is the move from a reactive to a proactive healthcare model. Predictive analytics and early warning systems, powered by machine learning, are now capable of identifying patients at high risk for conditions like sepsis or cardiac arrest, allowing for timely intervention. This foresight is mirrored in the operating theatre, where robotic surgery systems, guided by AI, offer surgeons unparalleled precision and control, leading to less invasive procedures, reduced complications, and faster recovery times.
This technological evolution extends beyond direct clinical care into the very fabric of healthcare operations. Key takeaways from our exploration include:
- Human-AI Collaboration is Key: The most effective applications of AI do not replace clinicians but augment their skills. AI serves as a powerful co-pilot, handling data-intensive tasks and offering insights that empower healthcare professionals to make more informed decisions.
- Operational Efficiency Unlocks Better Care: Automating administrative workflows, from scheduling to medical billing and coding, frees up valuable time and resources. This allows organisations to redirect focus from paperwork to patient-centred activities, improving both the staff and patient experience.
- Data is the Bedrock of Progress: The success of any AI initiative hinges on access to high-quality, secure, and diverse data. Establishing robust data governance and prioritising patient privacy are non-negotiable prerequisites for ethical and effective implementation.
Charting the Course for AI Adoption
For Canadian healthcare organisations, small businesses, and startups, the path forward involves a strategic and measured approach to integration. The initial step is not a massive technological overhaul but a careful assessment of specific pain points. Whether it’s reducing diagnostic wait times, optimising bed management, or personalising patient communication, a targeted strategy ensures a tangible return on investment.
The value of mastering these AI-driven approaches is immense. It translates to improved patient outcomes, reduced operational costs, and a competitive edge in a rapidly evolving sector. By embracing these innovations, we are not merely adopting new tools; we are building a more resilient, intelligent, and compassionate healthcare ecosystem. This convergence of human expertise and artificial intelligence is the cornerstone of a future where healthcare is more accessible, effective, and personalised for everyone.
Ready to explore how custom AI solutions can transform your healthcare organisation? The team at Cleffex Digital Ltd specialises in developing secure, compliant, and cutting-edge AI-driven software tailored to the unique challenges of the medical industry. Visit Cleffex Digital Ltd to learn how we can help you harness the power of AI to improve patient outcomes and streamline your operations.







