Think of AI in medical imaging as a highly-trained partner for radiologists. It uses sophisticated algorithms to comb through medical scans like X-rays, CTs, and MRIs, helping doctors spot signs of disease faster and more accurately than ever before. In many cases, it can catch subtle anomalies that the human eye might overlook.
This technology isn't here to replace clinicians. Instead, it acts as a second set of eyes, highlighting suspicious areas and automating repetitive tasks so that experts can focus on what matters most: the patient.
The New Era of Medical Imaging with AI

For decades, a radiologist's job was a lot like a detective's; carefully poring over images, searching for the smallest, faintest clues of disease. Today, AI has become its high-powered magnifying glass, bringing details into sharp focus that were once nearly impossible to see.
This isn't about handing the work over to a machine. It’s about creating a powerful partnership that enhances a radiologist's natural expertise, leading to quicker, more confident diagnoses. This collaboration is already proving essential in tackling major healthcare hurdles, like the frustratingly long wait times many people endure for critical scan results.
A Roadmap for Understanding AI in Diagnostics
This guide will walk you through exactly how AI is changing the game in medical imaging. We’ll break down everything from the core concepts to real-world examples and what’s on the horizon.
Here’s a look at what we’ll cover:
Core AI Technologies: We'll demystify the engines driving these tools, like machine learning and computer vision, in simple terms.
Real-World Applications: You'll see how AI is already making a difference in fields like oncology, neurology, and cardiology.
Workflow Transformation: We'll examine how these tools are making the entire diagnostic process smoother and more efficient.
Challenges and Ethics: A realistic look at the hurdles we still need to clear, from data privacy and algorithmic bias to regulatory approvals.
Future Innovations: A glimpse into what's next, including predictive analytics and the move toward truly personalized medicine.
The impact of this technology goes far beyond just one department. As we've touched on before in our post about how AI is helping the healthcare industry, these advancements are fundamentally reshaping patient care.
By sifting through massive datasets and recognizing patterns invisible to the human eye, AI can flag potential abnormalities with incredible speed. This allows radiologists to zero in on the areas that need their expert attention the most.
Ultimately, the aim is to build smart systems that support our medical professionals and lead to better health outcomes for everyone.
A Look Under the Hood: The Core AI Technologies in Diagnostics
To really get a feel for how AI is changing medical imaging and diagnostics, we need to pop the hood and look at the engines making it all happen. This isn't some black-box magic; it's a powerful combination of computational methods designed to learn from and interpret visual data, ultimately amplifying a clinician's own expertise.
Let's break down the main players.
Machine Learning: The Foundation
Think of Machine Learning (ML) as the system's foundational training. It’s like teaching a medical student by showing them thousands of labelled images: this is a benign tumour, this one is malignant. Over time, the student (or algorithm) learns to recognise the key patterns and distinguishing features on its own. ML provides the essential groundwork for medical image analysis.
Deep Learning and Neural Networks: The Specialist's Eye
Deep Learning is what happens when that student becomes a world-renowned specialist. It uses highly complex structures called neural networks, which are loosely modelled on the human brain's own layered architecture.
These multi-layered networks can analyse images with incredible depth, picking up on subtle patterns, textures, and anomalies that are often invisible to the human eye. This is the technology that empowers an AI to spot a minuscule, early-stage cancerous lesion on a high-resolution CT scan. The "deep" in deep learning really just refers to the sheer number of layers in the network, with each one adding a new level of analysis to produce a more refined and accurate conclusion. This sophisticated approach is quickly becoming the standard in the AI in Healthcare Industry.
Computer Vision: Giving AI the Power of Sight
If deep learning is the AI’s brain, then Computer Vision is its eyes. This is the field of AI that’s all about training computers to see and make sense of the visual world. In diagnostics, this is what lets an algorithm process a digital X-ray or MRI scan, correctly identify specific anatomical structures, and even segment different types of tissue from one another.
To make these concepts a bit clearer, here's a quick summary of how they work together.
Key AI Technologies in Medical Imaging
AI Technology | Primary Function in Imaging | Simple Analogy |
|---|---|---|
Machine Learning (ML) | Learns from labelled image data to identify patterns. | A medical student learning to recognise conditions by studying textbooks and case files. |
Deep Learning (DL) | Uses multi-layered neural networks for complex, nuanced image analysis. | A seasoned specialist with decades of experience spotting subtle clues others might miss. |
Computer Vision (CV) | Enables the AI to process, segment, and interpret visual information from scans. | The AI’s ‘eyes,’ allowing it to see and understand the content of an image. |
When you put them all together, you get a system where computer vision "sees" the scan, machine learning provides the basic knowledge, and deep learning delivers the expert-level analysis.
This infographic helps visualise how these technologies fit together to create practical applications.
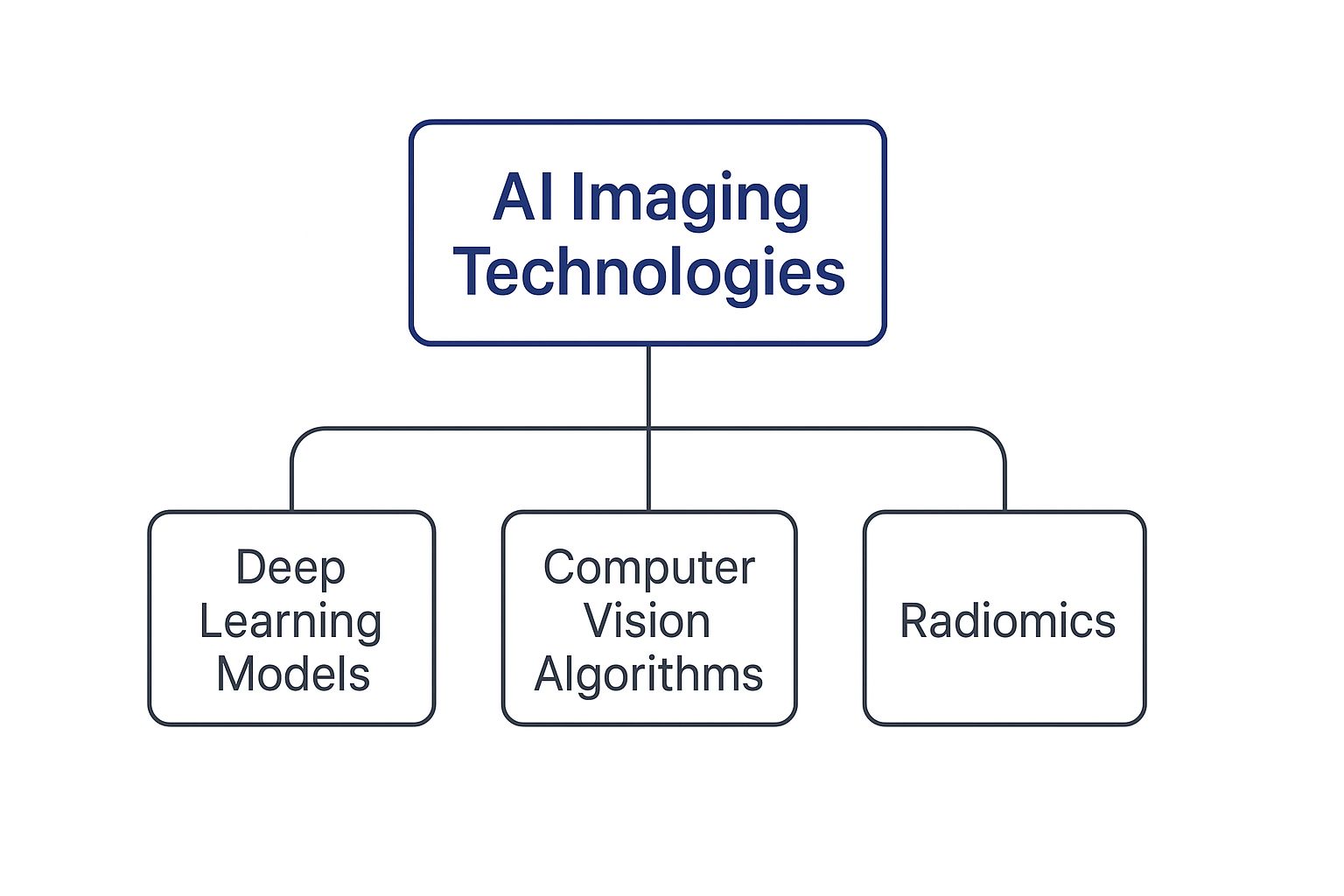
The diagram shows how more specialised techniques, like deep learning and computer vision, are the foundational pillars that support the entire field of AI imaging.
And this is driving real market growth. In Canada, the AI in medical imaging market is set to explode, projected to grow from USD 33.7 million in 2022 to USD 367.2 million by 2030. Deep learning is firmly in the driver's seat, accounting for nearly 57% of the revenue share in 2022 because of its superior accuracy in areas like neurology, cardiology, and breast screening. You can read the full research about these market trends here.
These technologies don’t work to replace clinicians. Instead, they equip them with an unprecedented level of insight. The goal is simple: flag potential issues with greater speed and precision, so medical experts can confirm diagnoses and plan treatments with more confidence than ever before.
Ultimately, knowing how these pieces fit together demystifies how AI tools are built and brought into the clinic. It’s this powerful technological base that allows a top-tier AI-Powered Healthcare Software Development Company to build solutions that genuinely improve patient outcomes. This progress is a huge part of the digital shift happening across medicine, and it relies on sophisticated Healthcare Software Development Services to bridge the gap between complex algorithms and everyday clinical use.
Real-World Applications of AI Across Medical Specialties

The theory behind AI in medical imaging is one thing, but seeing it work in the real world is where its value truly clicks. These intelligent systems are moving out of the research lab and into the clinic, making a direct impact on patient care right now.
We're not talking about far-off concepts anymore. These are practical tools helping doctors make better, more informed decisions every single day. By looking at a few specific examples, you can really start to see how AI is helping solve unique diagnostic challenges across different fields of medicine.
Enhancing Cancer Detection in Oncology
Oncology is easily one of the most impactful areas for AI in medical imaging. We all know the old saying, "early detection saves lives," and AI is becoming an incredibly powerful ally in that mission.
Think about what it takes to read a mammogram. A radiologist has to meticulously scan for minuscule calcifications or subtle changes in tissue that could signal early-stage breast cancer. It's a high-stakes, demanding task where the smallest oversight can have huge consequences. This is where AI comes in. Trained on millions of previous scans, these models can flag suspicious areas with impressive precision, acting as a vigilant second pair of eyes.
This doesn't replace the radiologist. Instead, it allows them to focus their expert attention on the specific areas the AI has highlighted, improving both their speed and accuracy. Some of these tools can even spot cancer cells that are almost invisible to the human eye, potentially catching the disease at its most treatable stage. It’s a collaborative process that ultimately means fewer missed diagnoses and faster answers for anxious patients.
Aiding Neurological Assessments
The human brain is a marvel of complexity, and interpreting neurological scans takes years of specialized training. In neurology, AI is giving clinicians a major assist, helping them identify signs of conditions like stroke, Alzheimer's disease, and multiple sclerosis with much greater confidence.
For instance, when a patient shows up with stroke symptoms, every second counts. An AI algorithm can tear through a CT scan in moments, looking for signs of a blockage or bleed in the brain. This kind of rapid analysis helps the medical team make immediate treatment decisions, which can dramatically improve a patient's recovery and minimise long-term brain damage.
The same goes for Alzheimer's research. AI models can measure subtle changes in brain volume over time or detect the amyloid plaques in PET scans that are tell-tale signs of the disease. Often, these markers appear long before a person shows major cognitive symptoms, opening the door for earlier intervention. You can learn more about how this technology is being applied in our AI in radiology practical guide for clinicians.
By automating the measurement of brain structures and flagging anomalies, AI provides neurologists with quantitative data to support their qualitative assessments. This combination of machine precision and human expertise leads to more robust diagnostic conclusions.
Advancing Cardiac Diagnostics in Cardiology
In cardiology, doctors often rely on imaging like echocardiograms, ultrasounds of the heart to see how well it's functioning. These scans are packed with information, but manually measuring key indicators like ejection fraction (a measure of how much blood the heart pumps with each beat) can be slow and prone to human variability.
AI algorithms can automate these calculations with incredible speed and consistency. The system can analyze the heart's movement frame-by-frame, spitting out a precise measurement in a fraction of the time it would take a person. This frees up cardiologists to see more patients and spend more time on the most complex cases.
These applications show that AI isn't some futuristic dream; it's a present-day reality that is fundamentally changing diagnostics, one specialty at a time. The key is building systems that fit seamlessly into the existing clinical workflow, bridging the gap between a powerful algorithm and a doctor who needs to make a critical decision.
How AI is Reshaping the Diagnostic Workflow
To really grasp the impact of AI in medical imaging, we need to look beyond the technology and see how it’s changing the day-to-day grind for clinicians. This isn't some far-off, futuristic idea. AI is already on the ground, acting as an incredibly smart assistant that refines and speeds up the entire diagnostic process.
What it really does is tackle the most stubborn bottlenecks in modern healthcare. By taking over the repetitive, time-consuming tasks, AI hands back precious hours to medical experts, letting them zero in on complex cases and critical patient decisions.
Boosting Speed and Prioritizing Care
One of the most immediate wins with AI is its knack for triage and prioritization. Picture a busy hospital radiologist facing a mountain of scans. An AI system can sift through that entire queue in moments, instantly flagging images that show signs of an urgent problem, like a possible stroke or a critical fracture.
This simple act pushes the most time-sensitive cases to the front of the line for human review. It’s like having a hyper-efficient assistant that constantly reorganizes your workload based on clinical urgency, making sure patients who need help right away get it. The result is a more responsive workflow that can make a real difference in patient outcomes.
This kind of efficiency is a game-changer, especially in healthcare systems under immense pressure. In Canada, for instance, wait times are a massive issue. The 2025 Philips Future Health Index Canada report found that 45% of Canadian patients face long waits for doctor appointments. For specialists, the average maximum wait is a staggering 131 days. These delays aren't just an inconvenience; one in five Canadians ends up in the hospital while waiting for care. AI tools that can accelerate image analysis and triage are a direct answer to these pressures. You can learn more about these healthcare findings from Philips.
Automating Tedious Tasks for Greater Precision
Beyond triage, AI is a master at automating the monotonous but vital tasks of measurement. Take tumour tracking for an oncology patient. Traditionally, a clinician has to manually measure the lesion on every single scan, a slow process that’s always prone to tiny human variations.
An AI tool does this in seconds, and it does it with perfect consistency every time. It can outline the tumour precisely, calculate its volume, and compare it against previous scans, generating objective, reliable data. This gives clinicians a much clearer, more confident picture of how well a treatment is working.
This kind of automation is popping up everywhere:
Organ Segmentation: Automatically outlining organs or other structures to set up surgical plans or guide radiation therapy.
Lesion Characterization: Analyzing the texture, shape, and features of an anomaly to help predict if it’s likely benign or malignant.
Report Generation: Drafting preliminary reports by documenting findings automatically, which the radiologist can then quickly review, edit, and sign off on.
By taking over these routine jobs, AI doesn’t just save time; it improves the quality and consistency of the diagnostic data itself. This frees up clinicians to focus their brainpower on interpretation, differential diagnosis, and working with other specialists to map out the best treatment plan.
Creating a Collaborative Human-AI Workflow
The end goal here isn’t to replace experts but to create a seamless partnership where human experience and machine precision work together. The idea is to integrate these tools in a way that supports clinicians, not disrupts them.
When AI reshapes the diagnostic workflow like this, the ripple effects are huge: faster reports, fewer potential errors, and patients starting treatment sooner. For a deeper look at how this is fundamentally changing medicine, you can find more insights into AI-driven diagnostics. This collaborative model is about empowering experts, giving them better tools to do what they do best.
Navigating The Hurdles of AI in Diagnostics

Bringing a technology as powerful as AI for medical imaging and diagnostics into clinical practice isn’t a simple plug-and-play affair. While the potential is enormous, the path to getting it right is lined with serious challenges that healthcare professionals, developers, and regulators need to tackle together.
To build real, lasting trust, we have to face these ethical questions and technical hurdles head-on. It's about more than just smart algorithms; it's about creating a system that is fair, transparent, and puts patient well-being first.
The Hurdle of Data Privacy and Security
The engine of any effective AI model is data, and lots of it. In medicine, that data is profoundly personal and sensitive, demanding the highest level of protection. This makes patient data privacy a cornerstone issue that can't be overlooked.
Developers have to be meticulous with anonymization and de-identification techniques. At the same time, healthcare organizations must navigate a maze of privacy laws to ensure that every single piece of data used to train AI models is handled legally and ethically.
Tackling Algorithmic Bias
An AI model is a reflection of the data it learns from. If that training data isn't a balanced representation of the entire patient population, the algorithm can inherit and even amplify human biases, leading to serious health inequities.
Think about it: an AI trained mostly on data from one demographic might be less accurate for others. This could make existing health disparities even worse. The solution involves consciously curating diverse datasets and constantly checking the algorithms to make sure they work fairly for everyone, regardless of their background. We've explored this in more detail in our article on the ethics of AI in healthcare.
“Solving algorithmic bias is not just a technical problem; it is an ethical imperative. To ensure AI promotes health equity rather than undermining it, developers and clinicians must work together to build, test, and deploy these tools with a conscious commitment to fairness and inclusivity.”
The 'Black Box' Problem and Regulatory Oversight
One of the biggest conversations in AI right now is the "black box" problem. This is what happens when a complex model gives an answer, but its reasoning is so tangled that even its creators can't fully explain how it got there. For a doctor who needs to stand by their diagnosis, that lack of transparency is a non-starter.
This has spurred the push toward Explainable AI (XAI), a field focused on making these models more transparent and their decisions easier to understand. In parallel, regulatory bodies like Health Canada are stepping up, creating new frameworks to approve AI-powered medical devices. They’re ensuring these tools are not just effective, but also safe, reliable, and clear in their function before they ever see a patient.
Navigating these challenges is fundamental to successfully integrating AI into the diagnostic workflow. Below is a summary of these key obstacles and the strategies being developed to overcome them.
Key Challenges in AI Medical Imaging Implementation
Challenge | Description | Mitigation Strategy |
|---|---|---|
Data Quality and Availability | AI models require massive, high-quality, and diverse datasets, which are often siloed or inconsistent across different healthcare institutions. | Develop federated learning models that train AI on local data without centralizing it. Create standardized data collection and labelling protocols. |
Algorithmic Bias | Training data that doesn’t represent diverse populations can lead to AI tools that perform poorly for minority groups, worsening health inequities. | Actively curate and balance datasets to include all demographics. Implement ongoing bias audits and fairness checks throughout the AI lifecycle. |
The ‘Black Box’ Problem | Many deep learning models are opaque, making it difficult for clinicians to understand or trust their outputs, which is a major barrier to adoption. | Invest in Explainable AI (XAI) research to create interpretable models. Develop tools that highlight the specific image features the AI used for its analysis. |
Regulatory Approval | The path to getting AI medical devices approved by bodies like Health Canada is complex and still evolving, requiring rigorous validation. | Establish clear, standardized validation frameworks for AI. Foster close collaboration between AI developers, clinicians, and regulatory agencies. |
Workflow Integration | Fitting a new AI tool into the established, high-pressure workflows of radiologists and pathologists without causing disruption is difficult. | Design AI solutions with direct input from end-users. Prioritize user-centric interfaces and seamless integration with existing PACS and EMR systems. |
Ultimately, overcoming these hurdles requires a collaborative effort. By focusing on ethical guidelines, technical transparency, and practical integration, the healthcare community can responsibly bring the benefits of AI to clinics and hospitals everywhere.
Looking Beyond the Horizon: What’s Next for AI in Medical Imaging?
If you think AI in medical imaging is impressive now, just wait. We're on the cusp of a major shift, moving far beyond simply spotting what's already there on a scan. The next chapter is all about prediction, seeing what's coming and heading it off at the pass. This isn't science fiction; it's the beginning of a truly proactive and deeply personalised era in medicine.
Think about it. We’re moving toward AI models that can do more than just flag a tumour. Imagine an algorithm that can look at an initial scan and accurately forecast that tumour's growth pattern, or even predict its response to various chemotherapy agents before a patient receives a single dose. That's the power of predictive analytics taking shape right now.
From Finding Disease to Forecasting It
The real game-changer will be using AI to anticipate disease long before the first clear symptom ever appears. By analyzing incredibly subtle changes in imaging data over time, patterns a human radiologist might not notice for years, AI could flag individuals at high risk for developing conditions like Alzheimer's or heart disease. This opens up a critical window for prevention that never existed before.
This potential is attracting serious attention and investment. The Canadian AI healthcare market, which includes these forward-looking diagnostic tools, hit USD 163.80 million in 2024. But it’s expected to explode to over USD 3.3 billion by 2033. This incredible growth isn't just hype; it's a direct response to real-world pressures like rising healthcare costs and an aging population, showing a massive vote of confidence in AI's ability to help. You can discover more insights about this expanding market and what's driving it.
Weaving Together a Complete Health Picture
The other exciting frontier is combining imaging data with everything else we know about a patient. AI's true potential will be unleashed when it can simultaneously analyze a patient's CT scan, their genetic markers, recent lab work, and their entire electronic health record.
By pulling all these threads together, we create a rich, multi-dimensional view of a person's health. This is what allows us to move away from a one-size-fits-all approach and design treatment plans tailored to a patient's unique biology. It’s the very definition of precision medicine.
The ultimate vision is a seamless partnership between clinician and machine, fundamentally changing how we deliver care. As an experienced AI-Powered Healthcare Software Development Company, we're building toward a future where this collaboration leads to better outcomes through smarter, more predictive tools.
The journey of AI in diagnostics is really just getting started. There are challenges to navigate, of course, but the path forward is clear: AI is becoming an indispensable partner for human experts. It’s already delivering on speed and accuracy, and now, it’s bringing foresight into the clinic. To see how we're committed to building this future, you can learn more about our team and expertise.
Your Questions About AI in Medical Imaging, Answered
As we wrap up this deep dive into AI's role in medical imaging, it's natural to have a few questions. Let's tackle some of the most common ones that come up in conversation.
What’s the Real Advantage of Using AI in Diagnostics?
It really comes down to two things: speed and precision. AI models can sift through thousands of scans far faster than any person could, highlighting areas of concern for a radiologist to review.
This not only speeds up the whole diagnostic process and gets answers to patients sooner, but it also acts as a second set of eyes, often spotting subtle patterns the human eye might overlook.
Is the Goal Here to Replace Radiologists?
Absolutely not. Think of AI as a highly specialized and incredibly efficient assistant, not a replacement. The idea is to build a collaborative partnership.
AI takes care of the high-volume, repetitive analysis, freeing up radiologists to pour their expertise into the most complex cases, consult with other physicians, and focus on patient care. Their critical thinking and experience are simply irreplaceable.
How Do You Handle Patient Privacy with These AI Systems?
Patient data security is non-negotiable. It's the foundation of any trustworthy medical AI tool. This is managed through a multi-layered approach: strict compliance with privacy laws, advanced data anonymization to strip personal identifiers, and the use of heavily encrypted platforms for all data handling.
Any credible player in the AI in Healthcare Industry builds their solutions with security and privacy at the very core of their design.
The smartest way to look at this is to see AI not as an automated doctor, but as a powerful tool that enhances the skills of medical professionals. The result is a healthcare system that's both more efficient and more accurate.
What are the Biggest Hurdles to Getting AI into a Clinic?
The challenges are often more practical than technical. First, there's the big task of integrating new AI software with a hospital's existing, often complex, IT systems. Then there's the significant upfront investment and, just as importantly, the need to properly train the clinical team to use these new tools effectively.
As we explored in our Healthtech adoption guide, navigating these operational roadblocks is crucial for success. Crafting these systems demands specialized Healthcare Software Development Services. For a truly integrated solution, partnering with an AI-Powered Healthcare Software Development Company ensures the technology actually solves real-world clinical problems. If you're interested in our approach, you can learn more about our team.
At Cleffex Digital Ltd, we specialize in building custom AI solutions that fit right into your existing healthcare workflows. We focus on boosting your diagnostic power while keeping security and compliance front and centre. Visit us to learn how we can help you build the future of medical diagnostics.







