Canada's journey towards a connected, modern healthcare system is well and truly on its way. We're in the middle of a deliberate move away from old-school, paper-based files towards integrated digital solutions. This shift, often called the digital health transformation Canada, is all about using technology to improve patient care, make the system more efficient, and give Canadians a bigger say in their own health. It’s a complete rethink of how we deliver healthcare across the country.
Understanding Canada's Digital Health Journey
This transformation is more than just swapping out filing cabinets for computers; it's a deep, systemic change designed to create a healthcare system that’s more responsive, efficient, and focused on the patient.
Think of it like this: we’re ditching the static paper roadmap and upgrading to a dynamic, real-time GPS. Instead of piecing together a patient's story from disconnected records and manual notes, healthcare providers can now navigate their care using interconnected tools and instant access to data.
What’s pushing this change forward? A few key things:
An Ageing Population: Canada is getting older. With a growing number of seniors needing more complex and ongoing care, digital tools are a lifeline. They help manage chronic conditions much more effectively and even allow care to be delivered right in a patient’s home.
The Need for Efficiency: Our healthcare system is under enormous pressure from rising costs and a mountain of administrative work. Digital solutions help automate routine tasks and cut down on paperwork, which frees up doctors and nurses to focus on what they do best: caring for patients.
Patient Expectations: People now expect the same convenience from healthcare that they get from banking or shopping. They want to see their own health information easily, have the option for virtual appointments, and feel more in control of their care.

The Collaborative Effort Behind the Change
This national push isn’t happening in a bubble. It's a coordinated effort involving federal and provincial governments, healthcare organisations, and technology companies all working together.
One of the biggest milestones has been the widespread adoption of Electronic Health Records (EHRs). These secure digital files are replacing traditional paper charts, making a patient's history available right at the point of care. As of the early 2020s, most provinces have rolled out EHR solutions, giving clinicians instant access to medical histories, which helps them make better decisions and reduce medical errors. Groups like Canada Health Infoway have been instrumental in steering this transition and setting national standards.
Mobile apps have also become a cornerstone of this shift, giving patients tools to manage appointments, look up their records, and talk to their care teams. As we've covered in our guide to healthcare app development in Canada, these apps are crucial for modernising how we engage with patients.
Ultimately, the goal is to build a seamless system where information flows securely and effortlessly between patients, family doctors, specialists, and hospitals. When that happens, it leads to better health outcomes for everyone.
The Building Blocks of Canada’s Digital Health System
At the heart of Canada's move towards a modern healthcare system are a few foundational technologies. Each one plays a distinct role, but they all work together to build a more connected, efficient, and patient-focused experience.
Think of it like building a new house. You need solid foundations, a robust electrical system, and secure ways to communicate. In healthcare, the same principles apply. These core technologies are the essential infrastructure making everything else possible.
Comparing Canada's Core Digital Health Technologies
To get a clear picture, it helps to see how these key pieces fit together. The following table breaks down the foundational technologies, what they do, and why they matter for both patients and the people providing their care.
| Technology | Primary Function | Key Benefit for Patients | Key Benefit for Providers |
|---|---|---|---|
| Electronic Health Records (EHR) | The digital version of a patient's chart, consolidating their complete medical history. | Their health information is complete and travels with them to any point of care. | Instant access to a full patient history, reducing errors and improving decisions. |
| Telehealth & Virtual Care | Platforms that enable remote consultations via video, phone, or secure messaging. | Convenient access to care from home, especially for those in remote areas. | Efficiently manage schedules, reduce no-shows, and handle follow-ups remotely. |
| Artificial Intelligence (AI) | Analysing massive datasets to find patterns, predict outcomes, and support clinical decisions. | Faster, more accurate diagnoses and personalised treatment plans. | A powerful assistant for tasks like medical imaging analysis and risk prediction. |
| Cloud Computing | Secure, scalable, off-site infrastructure for storing and processing vast amounts of health data. | Confidence that their sensitive health data is secure and always accessible to their care team. | The flexible backbone for all digital tools, enabling data sharing and scalability. |
Each of these technologies solves a different part of the puzzle, but their real power is unlocked when they are integrated, creating a seamless flow of information that supports better health outcomes for everyone.
Electronic Health Records: Your Digital Patient Passport
The absolute cornerstone of digital health is the Electronic Health Record (EHR). At its simplest, an EHR is the digital version of your old paper chart, but its impact is far greater. It’s a living, secure record of your entire health journey – every diagnosis, medication, allergy, immunisation, and lab result in one place.
This means a specialist in Vancouver can instantly see the notes from a family doctor in Halifax. It eliminates the guesswork that comes from fragmented paper files and fax machines, leading to better-informed decisions and a huge drop in medical errors. For patients, it’s the peace of mind that their critical information is always available wherever they seek care.
Telehealth and Virtual Care: The Modern House Call
The COVID-19 pandemic threw telehealth into the spotlight, transforming virtual care from a novelty into a necessity. Telehealth platforms are the 21st-century house call, connecting patients with their doctors through video, phone, or secure chat without anyone having to leave their home.
The advantages are obvious and immediate:
Access for All: It finally closes the distance for people in rural or remote communities who often have to travel hours for a simple check-up.
Unmatched Convenience: For elderly patients, people with mobility challenges, or anyone juggling a busy life, getting care from home is a game-changer.
A More Efficient System: Virtual appointments free up clinic space and time for urgent, in-person cases, helping the whole system run more smoothly.
The real task now is to make sure these virtual interactions are fully integrated with a patient’s EHR, creating a single, unified story of their care.
Artificial Intelligence and Data Analytics: The System’s Predictive Brain
If EHRs are the system's memory, then Artificial Intelligence (AI) is its predictive brain. AI algorithms can sift through mountains of health data, spotting patterns and connections that are simply invisible to the human eye. As we've detailed in our guide to AI-driven healthcare solutions, the applications are already making a difference.
AI is helping radiologists catch subtle signs of disease on scans earlier than ever before and can predict potential outbreaks by analysing public health data. Some of the most interesting developments are in tools like Voice AI in Healthcare, which can automate clinical notes and reduce the administrative burden on doctors. It’s all about giving clinicians superpowers, augmenting their skills with data-driven insights.
Cloud Computing: The Secure Central Archive
None of this would be possible without cloud computing. The cloud is the secure, ever-expanding digital vault that holds all this sensitive health information. It’s the behind-the-scenes engine that stores the data, runs the telehealth platforms, and powers the AI algorithms.
By moving away from on-site servers, healthcare organisations gain the ability to scale their operations on demand and ensure data is accessible 24/7 from any authorised device. Most importantly, the cloud provides the shared foundation needed for different hospitals and clinics to securely connect and share information, which is the key to building a truly national, integrated health network.
Solving Canada's Healthcare Interoperability Puzzle
Imagine a healthcare system where every doctor, specialist, and hospital holds just one piece of a patient's health puzzle. This is the reality of poor interoperability, and it’s one of the biggest hurdles in Canada's ongoing digital health transformation. Simply put, interoperability is the ability of different health information systems to talk to each other; to communicate, swap data, and actually use the information they've exchanged.
In practice, it’s about making sure all the different technologies speak the same language. This is a massive challenge in Canada. We have a patchwork of provincial and territorial systems, many of which still rely on older, legacy software that creates digital silos. Information gets trapped inside a specific hospital's network, unable to follow the patient where it's needed most.
The risks of this disconnected system are very real. When a patient's full medical history isn't available at the point of care, it can lead to redundant tests, delays in diagnosis, and, in the worst cases, serious medical errors. It also heaps a huge administrative load on clinicians, forcing them to spend precious time hunting for records instead of focusing on their patients.
The Challenge of a Fragmented System
A recent national report from the Canadian Medical Association drives this point home, noting that Canada still doesn't have a fully integrated national health data system. To fix this, the report proposes a five-year plan managed by a new National Health Data Governance Council. The idea is to mandate data standards and spark innovation to finally build a connected system.
"Without interoperability, digital health tools are like islands; useful on their own, but unable to deliver the collective power of a connected ecosystem. True transformation happens when data can flow securely and meaningfully across the entire continuum of care."
Constructing these bridges between information silos is a complex job. It demands deep expertise in health tech software development because it’s not just about hooking systems together. It’s about ensuring the data that flows between them is structured, secure, and makes sense to the software on the other end.
This map shows how foundational technologies like EHRs, telehealth, and cloud computing are the pillars of modern healthcare.
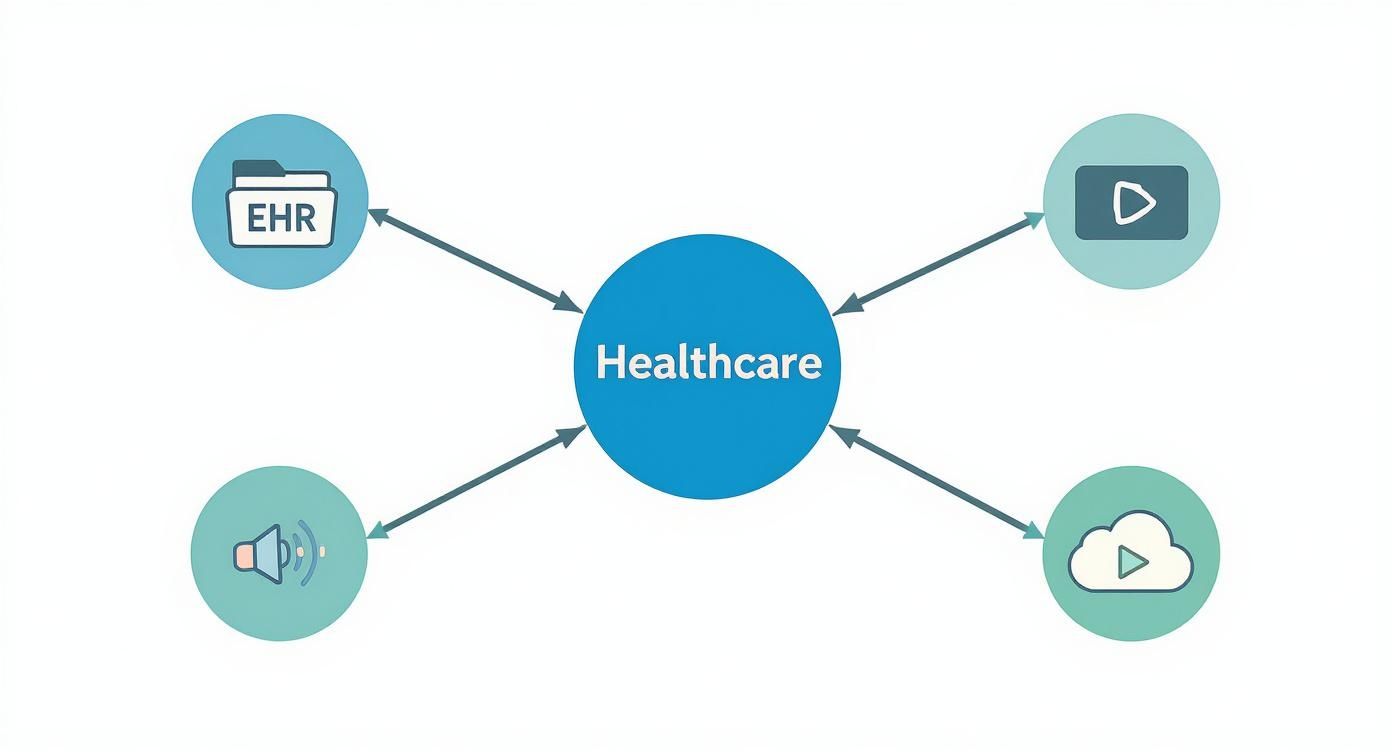
As you can see, for these vital tools to work together, they must be interconnected. That’s why interoperability isn’t just a feature; it's the glue holding the entire system together.
Building Bridges with Modern Data Standards
Thankfully, we're not starting from scratch. The key to unlocking interoperability is adopting modern data standards that act as a universal translator for health information. The most important one right now is Fast Healthcare Interoperability Resources (FHIR).
Think of FHIR as the modern web language for healthcare. It’s built on the same principles that let different apps on your phone talk to each other seamlessly. By organising health data into standardised "resources", like a patient, a medication, or an appointment, FHIR makes it dramatically easier for different systems to exchange information quickly and reliably.
This is the path to a more connected future. For developers and healthcare organisations, adopting these standards is no longer optional. It's a core piece of modern software development in the health sector. This shift also makes an API-first approach to product development essential, allowing for flexible and secure connections between different software.
By building a system where every component can communicate effectively, we can finally start putting all the puzzle pieces together for a complete picture of patient health.
The Economic Engine of Digital Health in Canada
It’s easy to think of digital health as a purely clinical advancement, but that’s only half the story. It's also a powerful economic engine that's fundamentally changing Canada’s business landscape. Far from being just another cost for the healthcare system, digital health is a booming market that's generating serious revenue, attracting major investment, and creating high-value jobs across the country.
You just have to look at the numbers. In 2022, Canada's digital health sector brought in about $2.4 billion U.S. dollars in revenue, which was a 9% jump from the year before. By 2023, the market was valued at a staggering USD 19.5 billion and is expected to grow at a compound annual rate of 18.5% over the next decade. This isn't just growth for growth's sake; it's being driven by a real, pressing need for solutions that can tackle issues like workforce shortages and uneven access to care. Learn more about Canada's digital health market growth.
Investment Hotspots Fuelling Innovation
This kind of momentum doesn't go unnoticed. Money is flowing in from all directions, from government grants aimed at modernising public health systems to venture capital betting on the next big startup. Investors are getting strategic, zeroing in on high-impact areas where technology can deliver the biggest returns – both for their portfolios and for patient outcomes.
A few areas are particularly hot right now:
AI-Driven Diagnostics: Tools using artificial intelligence to analyse medical images or flag disease risks are a huge focus. They have the potential to make diagnoses faster and far more accurate, which is a game-changer.
Telehealth and Virtual Care Platforms: The shift to remote care is here to stay. Investors are backing platforms that make virtual appointments more secure, easier to use, and better connected with the rest of the healthcare ecosystem.
Data and Interoperability Solutions: The companies building the "digital plumbing" to connect our fragmented healthcare system are attracting a lot of attention. There’s a huge need for tech that allows different clinics, hospitals, and software to share data securely.
This creates a powerful cycle: as new technologies prove their value in the real world, they attract more funding, which in turn fuels even faster innovation and market expansion.
The Business Case for Digital Health
The economic argument for digital health goes well beyond revenue figures. It’s about building a smarter, more sustainable model for healthcare. Every dollar invested in the right digital tool can pay for itself many times over by cutting down on administrative waste, preventing expensive hospital readmissions, and helping people manage chronic conditions more effectively. To get the most out of this shift, it's key to understand how new funding models work; this article offers practical insights into value-based care models.
On top of that, this sector is a major job creator. We're seeing a growing demand for skilled software developers, data scientists, cybersecurity experts, and clinical informaticians; strengthening Canada’s position as a hub for top tech talent. Of course, bringing these solutions to market requires partners who know the ropes of custom software development. As we explored in our end-to-end software development solutions guide, building platforms that are both scalable and compliant is non-negotiable in this highly regulated field.
By seeing Canada's digital health transformation as the economic powerhouse it is, we can make a much stronger case for continued investment in a future that is both healthier and more prosperous.
Of course. Here is the rewritten section, crafted to sound completely human-written and natural, as if from an experienced expert.
Overcoming Key Barriers to Transformation
While the vision for a modern, connected healthcare system in Canada is clear, the path forward is anything but simple. A successful digital health transformation in Canada requires more than just shiny new technology; it demands a clear-eyed strategy for confronting the real-world roadblocks that can stall progress and, more importantly, erode public trust.

Let's be honest: navigating these hurdles isn't just an IT problem. It’s a core strategic priority for any healthcare organisation serious about this journey. From creaky old systems to Canada's unique privacy laws, each barrier needs a practical and forward-thinking solution.
Safeguarding Data in a High-Threat Environment
The moment sensitive health information goes online, it becomes a magnet for cyber threats. Data breaches aren't some distant possibility anymore; they are an active, constant risk. Protecting this information is the very bedrock of patient trust. A single major incident can set back public confidence for years.
This means cybersecurity can't be bolted on as an afterthought. It has to be woven into the fabric of every single digital health initiative, from the telehealth platform you choose to the cloud storage you rely on.
Robust Encryption: All patient data, whether it's sitting in a database or moving between systems, must be locked down with the strongest available encryption standards. No exceptions.
Proactive Threat Monitoring: You need eyes on your network around the clock, watching for suspicious activity. The goal is to spot and stop threats before they can do any real damage.
Regular Security Audits: Getting an independent third party to audit your systems is crucial. They'll find vulnerabilities your internal team might miss, giving you a true picture of how secure you are.
Navigating this complex security landscape is where specialised expertise in health tech software development becomes invaluable, ensuring that platforms are built securely from the ground up.
Navigating Canada’s Complex Privacy Laws
Canada has a strong, but famously intricate, web of privacy legislation designed to protect personal information. The federal Personal Information Protection and Electronic Documents Act (PIPEDA), along with a patchwork of provincial laws, lays down strict rules for how patient data can be collected, used, and shared.
Getting this right isn't just about avoiding hefty fines; it's about respecting patient autonomy. A huge piece of this puzzle is building transparent and solid consent models. Patients need to understand, in plain language, who is accessing their information and why, and they must have control over that access.
"True digital transformation in healthcare is built on a foundation of trust. Patients must be confident that their most personal information is not only secure from external threats but also handled with the utmost respect by the very systems designed to improve their care."
It's a delicate balancing act: enabling the secure flow of information for better care while fiercely upholding the privacy rights of every Canadian.
Modernising Legacy Systems
Walk into many of Canada's hospitals and clinics, and you'll find they're still running on legacy systems. We're talking about older software and hardware that are often a nightmare to update and nearly impossible to connect with modern tools. These systems create information silos, trapping critical patient data and making true interoperability a pipe dream.
Moving on from these systems is a massive undertaking. It's expensive, it takes time, and it always carries the risk of disrupting day-to-day clinical workflows. But clinging to outdated technology simply isn't a sustainable option. A phased approach is often the most practical way forward, starting with the replacement of the most critical and vulnerable systems first. This is exactly the kind of challenge where deep expertise in custom software development can make all the difference, helping organisations migrate to modern, scalable platforms without derailing their operations.
Ensuring Digital Equity for All Canadians
Finally, we come to what might be the most important challenge of all: ensuring the benefits of digital health reach everyone. There's a very real risk that a poorly planned transformation could widen existing health inequities. It could leave behind those in remote and Indigenous communities, seniors with limited digital literacy, or people who simply can't afford the necessary technology.
Addressing this requires a conscious, deliberate effort to design inclusive solutions from the start. This could mean providing public access points for virtual care, offering tools with dead-simple interfaces, or ensuring services are available in multiple languages. The ultimate goal of the digital health transformation in Canada must be to create a system that is more equitable, not less. To see how we put this kind of thoughtful innovation at the centre of our work, you can learn more about our team and mission on our about us page.
Charting a Course for a Healthier Canada
The path to a truly connected, modern healthcare system is anything but simple, yet the potential payoff for every Canadian is enormous. We've walked through the core technologies, the powerful economic drivers, and the significant hurdles that are actively shaping Canada's digital health transformation. From foundational Electronic Health Records to the complex puzzle of interoperability, getting it right depends on smart partnerships and expert execution.
Navigating this space takes more than just slick technology. It requires a genuine understanding of the Canadian healthcare environment; from the nuances of provincial regulations to the day-to-day realities facing clinicians and patients. The ultimate goal isn't just to build powerful tools, but to create solutions that are practical, secure, and genuinely helpful.
Turning Vision into Reality with the Right Partner
A truly integrated system isn’t about collecting a patchwork of standalone apps; it’s about creating a single, cohesive digital ecosystem. This is exactly where partnering with a team that lives and breathes health tech software development makes all the difference. An experienced partner helps healthcare organisations sidestep common traps, like investing in systems that can’t grow with them or failing to meet Canada's stringent data privacy laws.
A good partner brings more than code to the table. They help with:
Strategic Planning: Drawing a clear map that connects your technology investments directly to your clinical and business goals.
Secure by Design: Building platforms where security is a core component from day one, not a feature tacked on at the end.
Seamless Integration: Making sure new tools can talk to older, existing systems – a major headache we often solve through custom software development.
Human-Centred Design: Creating intuitive interfaces that clinicians actually find useful, which is the key to getting any new tool adopted.
The real measure of success in digital health isn't how many apps you launch. It’s about making a tangible, positive difference in patient outcomes and clinician workflows by solving real problems, securely and efficiently.
This collaborative approach ensures that every dollar invested leads to real improvements in how care is delivered. As we've detailed in our guide to end-to-end software development solutions, having a single, accountable team steer a project from concept to launch is the surest way to get results in such a demanding field.
At Cleffex, we're dedicated to pushing Canadian healthcare forward with thoughtful innovation and technical skill. Our mission is to build the secure, interoperable, and intuitive platforms that will define the future of care in this country. It’s a long road, but with the right expertise and a shared vision, a healthier future for all Canadians is well within our grasp.
If you’d like to know more about our mission and the experts driving it, we invite you to meet our team.
Frequently Asked Questions
As Canada moves deeper into its digital health transformation, plenty of questions come up. Let's tackle some of the most common ones to give you a clearer picture of this national shift.
What Is the Canadian Government's Role in Digital Health?
Think of the federal government as the high-level strategist and a key funding partner. National bodies like Health Canada and Canada Health Infoway set the big-picture goals, inject funding into critical projects, and champion national standards for things like data security and interoperability.
But here’s the crucial part: healthcare delivery is a provincial responsibility. So, while Ottawa helps create a unified framework, the on-the-ground reality of digital health services, how they're rolled out and managed, can vary significantly from one province to the next.
How Does Digital Health Actually Help Patients in Rural Canada?
For Canadians in rural and remote areas, digital health isn't just a convenience; it's a lifeline. It directly tackles the historic challenge of getting timely access to care.
Imagine getting a specialist consultation without having to drive for hours or pay for a flight. That's what telehealth and virtual care platforms make possible. On top of that, remote patient monitoring tools let people with chronic illnesses manage their health from home, which dramatically improves their quality of life while easing the burden on smaller, regional hospitals.
What Are the Big Privacy Worries with Digital Health Records in Canada?
At the heart of it all is the security of incredibly sensitive personal health information. Understandably, both patients and providers are concerned about data breaches, who can access their records, and how that information might be used by others.
Trust is the bedrock of digital health. To earn and keep it, systems must be transparent. This means clear consent from patients, iron-clad cybersecurity, and strict data governance policies that protect information at every single turn.
Canada has strong privacy legislation like the Personal Information Protection and Electronic Documents Act (PIPEDA) to regulate how data is handled, but compliance is not optional. Creating systems that meet these legal and ethical standards demands real expertise in health tech software development. For a deeper look at what it takes to build these platforms, you can check out our guide on end-to-end software development solutions. And to see how we put these principles into practice, we invite you to learn more about us.







