Ever tried to fit a square peg in a round hole? That’s often what it feels like when Canadian healthcare providers try to use off-the-shelf software. You’re not just imagining it; that feeling of frustration is real, and it’s a sign that you need a system built for your reality, not a generic one.
Why Generic Software Fails Canadian Healthcare
Off-the-shelf software promises a quick fix, but it often operates on a one-size-fits-all model. In a field as precise and regulated as Canadian healthcare, that approach just doesn’t cut it. These pre-packaged platforms can end up creating more friction than they resolve, forcing your team to contort their proven workflows to fit the software's rigid structure.
This fundamental mismatch can be a drag on efficiency, a source of constant frustration for your staff, and ultimately, a risk to patient care. Let's be honest, a clinic in Ontario has different provincial rules to follow than one in British Columbia. It’s a level of detail that generic software almost always misses.

The Problem with a Standardised Approach
The central issue here is a lack of specificity. Generic systems rarely provide the nuanced features, like innovative healthcare documentation automation solutions, that are so vital for running a modern Canadian practice. Our healthcare landscape has unique challenges that demand a purpose-built solution.
Here’s where pre-built software typically falls short:
Regulatory Disconnect: Many off-the-shelf products, especially from international developers, aren't built from the ground up to comply with Canada’s tough privacy laws like PIPEDA or provincial legislation like Ontario’s PHIPA.
Workflow Inflexibility: They make your skilled clinicians and admin staff resort to clunky workarounds. This wastes precious time that should be focused on what truly matters – your patients.
Integration Roadblocks: These systems often create data silos because they can't properly connect with essential Canadian services, like provincial health networks, local labs, or pharmacy systems.
The decision between custom and off-the-shelf software is a critical one. For any Canadian healthcare organisation, picking a system that truly understands and adapts to local requirements isn't just an IT decision; it's a clinical and business imperative.
This is exactly why so many organisations are moving toward custom healthcare software Canada. Building a platform from the ground up means it’s designed to align perfectly with your clinical workflows, provincial compliance demands, and future goals.
As we cover in our guide on custom software vs off-the-shelf software, a solution made just for you delivers huge advantages in scalability and user adoption. It lays the groundwork for better patient care and operational excellence, and this guide will walk you through exactly how to plan, build, and launch a system that works for you, not against you.
Mastering Canadian Healthcare Compliance
Navigating Canada's healthcare regulations can feel like a maze, but it’s the bedrock of patient trust. When it comes to custom healthcare software, building compliance from the ground up isn't just an option; it's a requirement. This is about more than just dodging fines; it’s about showing an unwavering commitment to protecting incredibly sensitive personal information.
Think of it this way: The Personal Information Protection and Electronic Documents Act (PIPEDA) is the national rulebook for privacy, setting the standard for how private-sector organisations must handle personal data. But then, provinces often have their own, more detailed laws. Ontario’s Personal Health Information Protection Act (PHIPA) and Alberta’s Health Information Act (HIA) are perfect examples – they act like local bylaws, adding another critical layer of rules you must follow.
The Pillars of Canadian Healthcare Privacy
To build a compliant software solution, you need to get a firm grip on a few core principles. These aren't just legal roadblocks; they are the essential ingredients for creating a secure, trustworthy platform that patients and providers can rely on.
Here are the three areas that demand your full attention:
Data Residency: This is a straightforward but non-negotiable rule. The personal health information of Canadians must, in most cases, be stored on servers physically located within Canada. This ensures Canadian privacy laws, not foreign ones, are always in control.
Strong Encryption: Imagine encryption as a digital, unbreakable vault. All patient data, whether it's just sitting on a server (at rest) or being sent between systems (in transit), has to be encrypted to block any unauthorised eyes.
Access Controls: Not everyone in your organisation needs to see every piece of patient data. Role-based access control (RBAC) is the solution, ensuring that clinicians, administrative staff, and others can only see the specific information they need to do their jobs, and nothing more.
Getting these legal frameworks right is the first step for any project. For a deeper dive into the national regulations, it's worth reading up on the specifics of Canadian data privacy laws.
The Language of Interoperability
Beyond privacy laws, your software needs to "talk" to other healthcare systems securely. This is where interoperability standards come into play.
Think of HL7 (Health Level Seven) and FHIR (Fast Healthcare Interoperability Resources) as the universal languages of health data. Adhering to these standards ensures your custom platform can safely exchange information with labs, pharmacies, and provincial health networks, preventing the creation of isolated data silos. As we explore in our guide on healthcare app development in Canada, building with HL7 and FHIR from day one is the key to creating a truly connected care experience.
This screenshot from the Office of the Privacy Commissioner of Canada's website points you directly to the official resources for understanding PIPEDA.

The site offers a clear breakdown of the act, who it applies to, and what your obligations are, making it an essential bookmark for any development team.
To help you keep track of these crucial elements, here is a quick checklist summarising the key compliance areas for healthcare software in Canada.
Canadian Healthcare Compliance Checklist
| Requirement Area | Key Considerations | Governing Legislation |
|---|---|---|
| Data Privacy | Obtain clear consent for data collection and use. Implement privacy policies and assign a privacy officer. | PIPEDA, PHIPA (ON), HIA (AB), and other provincial acts |
| Data Residency | Store all Personal Health Information (PHI) on servers physically located within Canada. | Provincial legislation (e.g., PHIPA in Ontario) |
| Security Safeguards | Use strong encryption for data at rest and in transit. Conduct regular security audits and penetration testing. | PIPEDA, Provincial Acts |
| Access Control | Implement role-based access controls (RBAC) to ensure users only access necessary data. Maintain detailed audit logs. | PIPEDA, PHIPA, HIA |
| Interoperability | Adhere to HL7 and FHIR standards to ensure secure data exchange with other healthcare systems. | Pan-Canadian Standards |
| Breach Notification | Establish clear procedures for identifying, reporting, and responding to data breaches as required by law. | PIPEDA, Provincial Acts |
This table is a starting point, but it highlights the multi-faceted nature of compliance. It’s a continuous process, not a one-time setup.
The focus on compliance is also a major market driver. The Canadian Healthcare IT Market is growing rapidly, projected to hit USD 11,213.83 billion by 2032, according to Data Bridge Market Research. This surge is fuelled by healthcare providers seeking custom solutions that not only boost efficiency but also meet these stringent regulatory demands.
Ultimately, getting compliance right from the start is the foundation of any successful project in this sector. It’s what builds the trust and security that both patients and providers depend on every single day.
Building Blocks of a Modern Health Platform
A great custom healthcare platform isn't one single piece of software. It’s more like an ecosystem of interconnected tools, all working in concert. These are the core building blocks that turn a collection of separate administrative and clinical tasks into a smooth, patient-focused experience. Let's move past a simple feature list and look at how these essential components come together to create a powerful, cohesive system for any Canadian practice.
Think about a typical patient journey. It might start with them booking an appointment online through a secure portal, then having a telehealth call from their living room. In the background, their electronic health record gets updated instantly, and the billing module automatically gets the claim ready. This isn't science fiction; it’s what happens when the core modules of custom healthcare software are designed to speak the same language.

Core Modules That Drive Clinical Excellence
To build a platform that actually makes a difference, you need a few key modules. Each one solves a specific operational headache, and when they work together, they slash administrative time and elevate the quality of care.
The foundational modules nearly every practice needs include:
Electronic Health/Medical Records (EHR/EMR): This is the heart of the system. It’s the central, secure hub for all patient information. A custom-built EHR/EMR can be designed around your speciality’s unique charting requirements, ensuring clinicians can capture the right data without fighting the software.
Patient Portal & Appointment Scheduling: Giving patients control is a game-changer. A well-designed portal lets them book their own appointments, check lab results, message their provider securely, and manage their health info – all of which lightens the load on your front desk.
Telehealth & Virtual Care: Remote care is here to stay. An integrated telehealth module gives you a secure, PIPEDA-compliant video platform right inside your system, making virtual appointments ridiculously simple for both patients and practitioners.
The market reflects this shift. Canada's Healthcare Software as a Service (SaaS) sector is booming, with a projected compound annual growth rate of 19.53% between 2023 and 2033. The telemedicine segment alone grabbed 16.93% of that market revenue, which tells you just how critical virtual care has become.
Automating Administrative and Financial Workflows
A modern health platform does more than just manage clinical charts; it streamlines the entire business side of your practice. The right administrative modules can dramatically reduce manual grunt work and the risk of costly errors.
By automating routine tasks like billing and scheduling, healthcare providers can reallocate staff time from administrative duties to direct patient interaction, improving both operational efficiency and the quality of care.
Key modules for the back office include:
Billing & Revenue Cycle Management: Custom billing modules can be built to navigate the complexities of provincial health plans (like OHIP or AHCIP), private insurance, and direct patient payments. Automating this process means claims go out faster and with fewer rejections.
Prescription Management (e-Prescribing): This module lets clinicians fire off prescriptions directly to pharmacies electronically. It’s a huge win for patient safety, eliminating messy handwriting errors and automatically checking for potential drug interactions or allergies.
In the end, these aren't just isolated features. They are the gears that make a modern healthcare practice run. As we've covered in our guide to cloud-based medical systems, pulling these components together into a unified, cloud-based platform is the secret to scaling and accessibility. The goal is to weave these building blocks into a solution that feels smart, intuitive, and absolutely essential to your daily work, creating a better experience for everyone involved.
Choosing the Right Development Partner
Let's be blunt: picking your development partner is the single most important decision you'll make in this entire process. It’s a choice that will have a direct ripple effect on the quality, compliance, and ultimate success of your custom healthcare software. Forget the generic advice. What you need is a practical way to find a partner who genuinely gets the unique quirks of the Canadian healthcare system.
The right team does far more than just write code. They need to be a strategic ally, someone who understands the tangled web of provincial regulations and national privacy laws. Their expertise has to go beyond the technical and into the day-to-day reality of clinical workflows. This is the only way you'll get a final product that isn't just functional, but is actually intuitive and helpful for your clinicians and staff.
Verifying Canadian Healthcare Expertise
When you start talking to potential partners, your first filter should be their real-world experience in the Canadian healthcare sector. A flashy portfolio of general software projects just doesn't cut it. You need hard proof that they've been in these trenches before and successfully navigated the specific challenges our regulated industry throws at them.
Here’s what to dig for:
Fluency in PIPEDA and Provincial Laws: Don't just ask if they're compliant. Ask them to walk you through specific examples of how they've designed systems to meet PIPEDA and provincial rules like Ontario's PHIPA or Alberta's HIA. They should be able to talk confidently about data residency and why it matters.
Canadian Case Studies: Ask to see case studies or, even better, speak to references from their other Canadian healthcare clients. A partner with a solid track record in Canada won't be shy about sharing their successes.
Deep Interoperability Knowledge: Gauge how well they really understand HL7 and FHIR standards. Building a system that can securely talk to provincial health networks, labs, and pharmacies isn't a "nice-to-have"; it's a fundamental requirement for creating connected care.
Choosing the right partner means digging deep to verify their experience, scrutinising their portfolio, and understanding what happens after the project goes live.
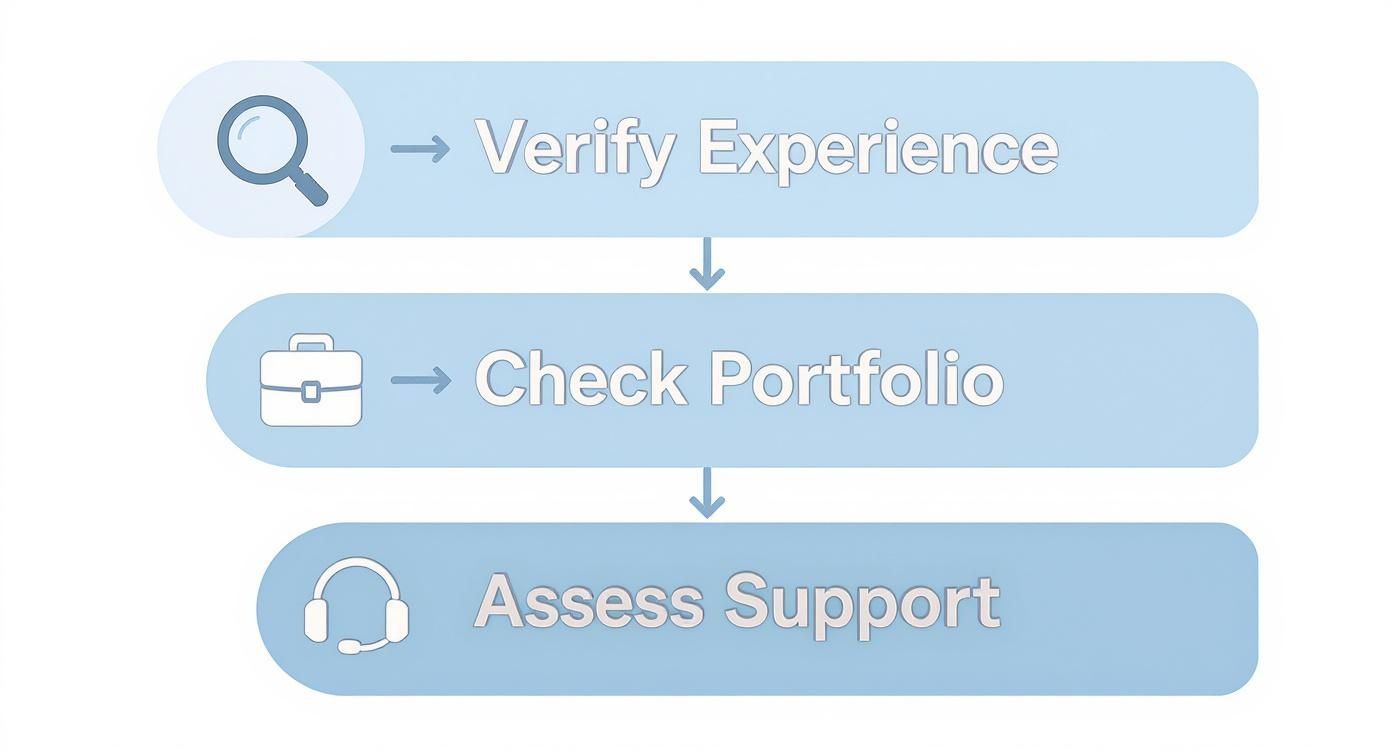
This entire process is about more than just technical skill; it’s about finding a team with proven local experience and a real commitment to a long-term partnership.
Assessing Project Management and Long-Term Support
Building software isn't a one-off transaction; it's a long-term relationship. You need a partner whose working style meshes with your organisation's culture. Things like clear communication, transparency, and a solid plan for post-launch support are every bit as important as the initial build. A great partner for custom healthcare software in Canada is one who is already thinking about year two and beyond.
A true partnership is built on transparency and a shared vision. Make sure you ask about their project management style, whether it's Agile or another iterative method, to ensure it gives your clinical team regular opportunities to provide feedback.
To help you vet potential partners, we've put together a checklist. Think of this table as your guide during those crucial initial conversations.
Vendor Selection Criteria Comparison
| Evaluation Criterion | Why It Matters | Key Questions to Ask |
|---|---|---|
| Canadian Healthcare Portfolio | You need proof, not promises. Their past projects are the best indicator of their ability to handle your specific regulatory and clinical needs. | "Can you show us 2-3 case studies from Canadian healthcare clients?" |
| "Can we speak with a past client?" | ||
| PIPEDA/PHIPA Compliance | Non-compliance can lead to massive fines and a total loss of trust. This is non-negotiable. | "Walk us through how you ensure data residency and privacy controls in your architecture." |
| "Have you undergone a third-party security audit?" | ||
| Interoperability (HL7/FHIR) | Your software can't be an island. It must communicate with the rest of the healthcare ecosystem securely and efficiently. | "Describe a project where you integrated with a provincial health information exchange or a hospital EMR using FHIR." |
| Project Management & Communication | A poor process leads to delays, budget overruns, and frustration. You need transparency and a clear rhythm of communication. | "Who will be our single point of contact?" |
| "What's your process for handling scope changes mid-project?" | ||
| Long-Term Support & Maintenance | Software is a living asset that needs ongoing care, security patches, and updates to remain effective and secure. | "What do your support and maintenance plans include?" |
| "What are the associated costs and service level agreements (SLAs)?" | ||
| Technical Team & Scalability | The team building your software should have the right skills and be able to grow with your needs. | "Who are the key developers on the team, and what is their experience?" |
| "How do you ensure the platform can scale as our user base grows?" |
Using a structured checklist like this ensures you're comparing apples to apples and making a decision based on the factors that truly matter for a successful healthcare technology project.
Ultimately, you're looking for a team that brings more to the table than just technical competence in healthcare software development. You need a partner who shows a genuine commitment to your organisation's mission. Their deep understanding of the Canadian landscape is what turns a simple custom software development project into a strategic asset that will serve you for years to come. It’s the kind of specialised expertise we've built our reputation on, as you can learn more on our about us page, and it's what you should demand from any potential partner.
Your Project Roadmap: From a Bright Idea to a Working Reality
Taking a concept for a new healthcare application and turning it into a compliant, fully functional tool that people actually use is a journey. It’s not just about coding. This roadmap will walk you through the entire process, step-by-step, so you can see exactly how it’s done. Knowing these phases helps keep your project on schedule, on budget, and true to your original vision.
The real work starts long before anyone writes a single line of code. It all kicks off with a Discovery and Strategy Phase. This is where your team and your development partner get into a room (virtual or otherwise) and hammer out the fundamentals. What problem are we solving? Who is this for – clinicians, admin staff, patients? What do their daily workflows look like? Getting this foundation right is everything for a successful custom healthcare software project in Canada.
Designing for People, Not Just for a System
With a clear strategy in place, the spotlight turns to UI/UX (User Interface/User Experience) Design. In healthcare, you could argue this is the most critical stage of all. It doesn’t matter how powerful your software is on the back end; if the interface is clunky or confusing, clinicians simply won't use it. The goal is to create something so intuitive and efficient that it feels like a natural extension of their work, not another frustrating task.
This means building detailed wireframes and, more importantly, interactive prototypes. These aren't just static pictures; they're clickable mock-ups of the software. This lets your team actually feel the workflow and give concrete feedback before the heavy lifting of development even starts. It’s a cycle of trying, tweaking, and trying again until it just feels right.
This is where an Agile development approach really shines in healthcare. It’s built on short cycles, or "sprints," that allow for constant feedback. Clinical staff can review progress frequently and point out what’s working and what isn’t. This flexibility ensures the software adapts to real-world needs, saving you from a major and expensive rethink down the road.
The need for these specialised tools is driving serious growth. The Canadian healthcare IT software market, currently valued at USD 2.78 billion, is expected to hit USD 6.94 billion by 2031. This surge is fuelled by the demand for digital solutions like custom EMRs and telehealth platforms. You can read the full research about the Canadian healthcare IT software market to see the trends for yourself.
Building, Testing, and Going Live with Confidence
Once everyone agrees on the design, the Development Phase begins. This is where the developers take the blueprints and start building the actual application, piece by piece, integrating all the modules you defined earlier. At the same time, a parallel and equally important process kicks off: Quality Assurance (QA) and Testing.
In healthcare, testing has to be absolutely meticulous. It's not just about finding bugs. We have to cover several key bases:
Functional Testing: Does every single button and feature do exactly what it’s supposed to?
Security Testing: Have we identified and sealed any potential vulnerabilities that could expose sensitive patient data?
Compliance Testing: Does the software meet every single requirement under PIPEDA and relevant provincial laws? No exceptions.
Usability Testing: We put the software in front of actual users – nurses, doctors, admins – to see if they can navigate it easily and efficiently.
After the software has passed every test with flying colours, it’s time for the Deployment Phase. This is a carefully orchestrated event. It often involves migrating data from older systems and always includes thorough training for all staff. The whole process is managed to cause as little disruption to your daily operations as possible.
But the journey isn't over when you go live. The final, ongoing phase is Maintenance and Support. This ensures your software stays secure with regular updates, performs reliably, and continues to evolve as your organisation’s needs change. Following a clear roadmap like this is the key to any successful custom software development project, and it's a process we've refined over many years. It turns your vision into a real-world asset that makes a tangible difference in your practice. To make it happen, you need a team that lives and breathes this entire lifecycle – a commitment we stand by, as you can see when you learn more about us.
Budgeting for Your Custom Software Project
Sooner or later, every project discussion boils down to two critical questions: how much will it cost, and how long will it take? When it comes to building custom healthcare software in Canada, getting a clear, transparent answer is essential for planning. The final numbers are always a mix of project complexity, required integrations, and the detailed compliance work that’s non-negotiable in our sector.
Think of it like building a house. A small, simple bungalow has a very different price tag and build schedule than a multi-storey home packed with custom features and a high-tech security system. The same logic applies here.
Key Cost and Timeline Drivers
The scope of your project is, without a doubt, the single biggest factor that shapes the budget. A straightforward Minimum Viable Product (MVP) built to solve one specific problem will always be faster and more affordable to develop than a massive, enterprise-wide platform with a dozen interconnected modules.
Here are the main variables that will influence your investment:
Platform Complexity: A simple patient scheduling portal is worlds away from a full-featured Electronic Health Record (EHR) system designed to manage complex clinical data and workflows. The more unique features and user screens you need, the more development hours it will take.
Integration Requirements: Will your new software need to talk to existing systems? Think provincial health networks, labs, or pharmacy management software. Each one of those connection points adds a layer of complexity and requires precise engineering to keep data exchange secure.
Compliance and Security: Sticking to PIPEDA, PHIPA, and other regulations isn’t optional. This means specialised architectural design, thorough security audits, and meticulous documentation – all of which factor into the project's cost and timeline.
Data Migration: If you're pulling data out of an old legacy system and moving it into your new platform, that process needs careful planning and execution. You can't afford to lose or corrupt data along the way.
Budgeting for custom software isn’t about finding the cheapest path forward. It’s about investing in a secure, compliant, and scalable asset that delivers value for years to come. A good budget covers the initial build and the ongoing support.
Realistic Budget and Timeline Estimates
To set realistic expectations with your team and stakeholders, it helps to think in ranges based on project size. While no two projects are identical, these figures offer a general guideline for planning your investment in quality healthcare software development.
A focused MVP or a small-scale application can often be built in 3-6 months. A mid-sized project with several modules and a few integrations might take 6-12 months. A large-scale, enterprise-level system could easily take more than a year to complete. This whole journey, from the initial idea to a successful launch, needs a solid roadmap, much like the one we map out as we explored in our end-to-end software development solutions guide.
Understanding these factors helps you approach any custom software development project with your eyes wide open. It’s also why partnering with a team that gets these nuances is so important; it's a level of expertise we’ve built our reputation on, as you'll see when you learn more about us.
Frequently Asked Questions
Building a custom medical platform is a big undertaking, and it's natural to have questions. Here, we'll tackle some of the most common ones we hear from Canadian healthcare organisations to give you the clear, straightforward answers you need.
What's the Real Advantage of Custom Software Over an Off-the-Shelf EHR in Canada?
The single biggest advantage is that it’s built just for you. Think of it like a tailored suit versus one off the rack. While pre-packaged systems are designed to serve everyone reasonably well, custom healthcare software in Canada is meticulously crafted around your clinic's specific workflows, your speciality's unique needs, and how you want to interact with your patients.
This perfect fit isn't just a luxury; it translates into real-world benefits. Your staff will actually want to use it, which drives up adoption rates and boosts efficiency. It also gives you the freedom to innovate your care model without being constrained by a rigid system. Most importantly, a custom build ensures that compliance with Canadian regulations like PIPEDA and provincial data residency rules is baked in from day one, not bolted on as an afterthought.
How Can I Make Sure My New Software Will Talk to Other Systems, Like Labs and Pharmacies?
The key is to build it with a common language from the start. In healthcare, that language is built on interoperability standards, primarily HL7 (Health Level Seven) and its modern successor, FHIR (Fast Healthcare Interoperability Resources). You need to make this a non-negotiable requirement in your project plan.
Your development partner must have a proven track record of building APIs (Application Programming Interfaces) that let your system securely exchange information with others. This is what allows you to pull in lab results, send e-prescriptions to pharmacies, and connect with provincial health networks. Taking this approach from the outset prevents the creation of isolated data islands, which is a critical part of modern healthcare software development.
How Much Time Will My Clinical Team Need to Commit During Development?
A lot, and that's a good thing! Your clinical team's active and ongoing participation isn't just helpful; it's essential for success. They’re the ones who will use the software every day, and their hands-on expertise is something no developer can replicate.
Their input is vital right from the beginning to map out current workflows, during the design phase to make sure the interface is practical and intuitive, and throughout the testing process to confirm it works in real-world scenarios. A great strategy is to appoint a "clinical champion" – a dedicated point person from your team who can provide consistent feedback.
Is It Better to Host My Custom Software in the Cloud or On-Premise Here in Canada?
Both paths are possible, but the scales are definitely tipping toward cloud-based solutions (often called SaaS, or Software as a Service) for Canadian healthcare. Choosing a top-tier Canadian cloud provider, like AWS Canada or Microsoft Azure Canada, takes care of the data residency requirement and comes with a whole suite of security and compliance certifications.
The cloud offers the flexibility to scale up as you grow, avoids the hefty upfront cost of buying and setting up servers, and simplifies ongoing maintenance. On-premise hosting gives you total physical control, but it demands a significant initial investment and a skilled IT team to manage everything from security to system updates. Your budget and in-house IT capacity will be the deciding factors. This choice is a cornerstone of any custom software development project and, as we explored in our end-to-end software development solutions guide, influences everything that follows.
Ready to build a healthcare solution that meets Canada's unique demands? At Cleffex, we specialise in creating secure, compliant, and user-friendly software that empowers providers and improves patient care. Learn more about our team and our commitment to excellence on our about us page.