In healthcare, artificial intelligence has moved from a far-off concept to a core component that's actively reshaping medical software development. This isn't just about adding a new feature; it's a fundamental change in how we think about patient care, diagnostics, and the day-to-day running of medical facilities. By integrating AI, we’re building tools that are not only smarter but also safer, more precise, and ultimately more effective.
How AI is Reshaping Medical Software

The real story of AI in medical software development isn't about simple automation. It's about giving software the ability to analyse complex medical data at a scale and speed that's impossible for humans. Machine learning algorithms can sift through millions of data points, from patient records and lab results to genomic sequences and MRI scans, to spot patterns and generate insights that were previously hidden.
Think of it as a super-powered assistant for clinicians. This assistant can instantly review a patient's entire history and compare it against thousands of similar cases to flag potential risks or suggest a diagnostic path. This capability leads to earlier disease detection and opens the door to truly personalised treatment plans, designed around a person’s specific genetic makeup and health profile.
The New Reality in Healthcare Technology
This isn't just an upgrade; it's a complete rethink of what medical software can do. The job of software is no longer just to store information but to actively help us understand it. Getting this right requires a careful, strategic approach to building tools that are powerful, compliant, and genuinely useful in a busy clinical environment.
To give you a clearer picture, here’s a quick summary of where AI is making the biggest waves.
Key Areas of AI Transformation in Healthcare
| Domain | AI Application | Impact on Patient Care |
|---|---|---|
| Predictive Analytics | Models forecast disease outbreaks, flag high-risk patients, and predict hospital admission rates. | Allows for proactive interventions and better resource management, preventing crises before they start. |
| Diagnostic Assistance | Image recognition algorithms help radiologists and pathologists spot subtle anomalies in scans and slides. | Increases the speed and accuracy of diagnoses, reducing the chance of human error and catching diseases earlier. |
| Personalised Medicine | AI analyses genetic and clinical data to match patients with the most effective drugs and therapies. | Moves away from one-size-fits-all treatments toward care that is tailored to an individual’s unique biology. |
| Operational Efficiency | Automates administrative tasks like patient scheduling, medical coding, and clinical trial recruitment. | Frees up clinical staff from paperwork to focus on what matters most: patient care. |
As you can see, the goal is always to equip clinicians with better information for better decision-making.
By turning raw data into actionable intelligence, AI-powered software gives clinicians the tools to make more informed decisions, ultimately leading to better patient outcomes.
This guide is designed to be a practical roadmap for building and deploying these solutions. It highlights why working with skilled AI software development services is so important for navigating the technical and regulatory hurdles. A clear strategy is non-negotiable, a point we often stress in our general software development guide. The journey begins with a solid understanding of what AI can realistically achieve and how to apply it responsibly.
At Cleffex, we build on a deep foundation of custom software development expertise. Our team, which you can read more about on our About Us page, is committed to pushing the boundaries of what's possible in medical technology.
Real-World AI Applications in Healthcare

The theory behind AI in medicine is one thing, but where does the rubber meet the road? We're now seeing AI move out of the research lab and into the clinic, making a real difference in patient outcomes and how clinicians work. These tools aren't about replacing human experts; they're about augmenting their skills, helping them see more, connect the dots faster, and act with greater certainty.
This shift is especially clear in fields like diagnostic imaging and radiology. In Canada, for example, Health Canada is actively licensing AI-powered medical devices designed to help with diagnosis and disease prediction. They’ve recognised that old regulatory models don't quite fit the fast, iterative nature of AI.
Working alongside the US FDA and UK MHRA, they’ve published guidelines on 'Good Machine Learning Practice for Medical Device Development'. This is a big step toward setting international standards, ensuring AI is woven into our healthcare system safely and effectively.
AI-Driven Diagnostic Imaging
Medical imaging is probably one of the most mature and impactful applications of AI today. Think of a specialised AI model, like a Convolutional Neural Network (CNN), as a set of highly trained eyes. It’s been shown millions of scans and has learned to spot patterns that a busy human radiologist might miss.
These algorithms can comb through X-rays, CT scans, and MRIs to find incredibly subtle signs of conditions like cancer, stroke, or diabetic retinopathy with stunning accuracy. The AI’s job isn't to make the final call, but to flag areas of concern, acting as a tireless second opinion. This lets radiologists zero in on what matters most, leading to quicker, more reliable diagnoses.
As we covered in our deep dive on AI for medical imaging and diagnostics, this partnership between human expertise and machine precision is a game-changer.
By highlighting potential anomalies that need a second look, AI helps radiologists manage their workload, combat burnout, and ultimately deliver more accurate reports.
Unlocking Insights with Natural Language Processing
Hospitals are swimming in text-based data – clinicians' notes, patient records, research papers, you name it. Natural Language Processing (NLP) is the technology that helps make sense of this mountain of unstructured information. It's designed to read and interpret human language, turning dense clinical stories into organised, actionable data.
A fantastic real-world example is how NLP is automating clinical documentation. For instance, AI in medical transcription can listen to a doctor's spoken notes and instantly turn them into perfectly organised text right inside the patient's electronic health record (EHR). That alone saves clinicians from hours of tedious administrative work every single day.
But it doesn't stop there. NLP is also being used to:
Scan clinical notes to find patients who are a perfect match for clinical trials.
Analyse patient feedback to spot trends in care quality and safety concerns.
Condense long, complex medical histories into a quick summary for doctors.
Forecasting with Predictive Analytics
Predictive analytics is about using past data to get a glimpse into the future. In a healthcare context, that could mean anything from anticipating flu outbreaks and identifying patients at high risk for chronic disease to predicting who is likely to be readmitted to the hospital.
For example, public health officials can feed anonymised location data and health reports into an AI model to forecast how influenza might spread through a community. This kind of foresight allows for proactive healthcare. Hospitals can get ahead of staffing and resource needs, while doctors can intervene with preventative care before a patient's health takes a turn for the worse. It’s a fundamental move away from reactive treatment toward data-driven prevention.
Personalising Medicine with Genomic Analysis
Finally, AI is the engine driving personalised medicine forward. The human genome is a staggering collection of billions of data points, and AI algorithms are the only tools capable of analysing that level of complexity. By cross-referencing a patient's unique genetic code with their clinical data, AI can help pinpoint the single most effective treatment for their specific biology.
This is having a massive impact in oncology. AI can match cancer patients with targeted therapies that work better and have fewer side effects than one-size-fits-all chemotherapy. By understanding the specific genetic triggers of a tumour, doctors can prescribe the right drug for the right patient, at the right time.
Navigating Data Privacy and Regulatory Compliance
When you're building medical software with AI, protecting patient data isn’t just a feature on a list – it's the absolute foundation of everything. Trust is the currency of healthcare, and every algorithm and database has to be built on a rock-solid base of security and strict compliance with global regulations. This isn't just a good idea; it's a non-negotiable.
Losing that trust doesn't just damage your reputation; it can cause real harm to patients and bring about crippling legal and financial consequences. You have to navigate a complex web of rules, particularly the Health Insurance Portability and Accountability Act (HIPAA) in the United States and the General Data Protection Regulation (GDPR) in Europe. These aren't afterthoughts; they need to be woven into your project from the very first line of code.
The Pillars of Health Data Regulation
At their core, HIPAA and GDPR are all about giving people control over their own health information. While they share that common goal, they go about it in different ways, with specific requirements that have a huge impact on how you train and deploy AI models.
Getting these rules right is critical. For example, both frameworks require some form of patient consent, but GDPR is far more stringent. It introduces the 'right to explanation,' which means you must be able to explain the logic behind an AI-driven decision, like a diagnosis, to a patient. That’s a massive technical and ethical consideration for any medical software development team.
Comparing HIPAA and GDPR for AI Medical Software
To get a clearer picture, it helps to see these two major regulations side-by-side. Their differences have significant implications for how you design and build AI-powered healthcare tools, especially if your software will be used internationally.
Here’s a breakdown of the key distinctions you need to keep in mind:
| Compliance Aspect | HIPAA Requirement | GDPR Requirement |
|---|---|---|
| Data Scope | Protects "Protected Health Information" (PHI) created or received by covered entities in the US. | Protects "personal data" of any EU resident, a much broader category that includes health, genetic, and biometric data. |
| Patient Consent | Consent is often implied for treatment, payment, and healthcare operations. | Requires explicit, unambiguous consent for specific data processing purposes. Patients must actively opt-in. |
| Data Anonymisation | PHI can be de-identified by removing 18 specific identifiers, making the data non-personal. | Uses terms like pseudonymisation and anonymisation, with stricter standards for what counts as truly anonymous data. |
| AI Decision-Making | Does not explicitly address a "right to explanation" for automated decisions. | Includes the "right to explanation," requiring transparency in how automated decisions affecting individuals are made. |
As you can see, what works for HIPAA compliance alone won't necessarily cut it for GDPR. Building for a global market means designing for the strictest standard from day one.
Building Compliance into the Code
Compliance isn't a final hurdle you clear before launch; it's a continuous mindset that has to be baked into the entire development lifecycle. This is often called "privacy-by-design" – a philosophy where data protection is treated as a core system requirement, not an add-on.
Thankfully, new techniques are making it possible to build powerful AI systems that respect patient privacy from the ground up. One of the most important is federated learning.
Federated learning is a game-changer for privacy. It allows an AI model to learn from data across multiple hospitals or clinics without the sensitive patient information ever leaving its original, secure location. The model trains locally on the data, and only the anonymised insights are shared and combined. The raw data stays put.
This single technique dramatically cuts the risk of data breaches during the model training phase. For a closer look at the unique challenges and solutions within Canada's privacy landscape, our guide on AI in healthcare data privacy in Canada offers some really practical insights.
Actionable Strategies for Secure Development
To make sure your AI medical software is both effective and compliant, you need to turn these principles into practice. Here’s where to focus your efforts:
Strict Data Anonymisation: Go beyond just stripping out names and addresses. Use advanced statistical methods to ensure individuals can't be re-identified, even if the data is cross-referenced with other public information.
Robust Consent Management: Your user interface must have clear, simple consent workflows. Patients need to understand exactly what data is being used and why, and they must have an easy way to opt out at any time.
Audit Trails and Explainability: You need to log every time an AI model accesses patient data. More importantly, you should be developing "explainable AI" (XAI) techniques that can provide clear, human-readable reasons for a model's conclusions.
For any company dealing with data from EU residents, keeping up with GDPR is an ongoing task. This comprehensive GDPR compliance checklist is a great resource for staying on top of its demands.
Ultimately, these practices ensure the solutions you build are not just clinically effective but also fundamentally trustworthy. In modern healthcare, that trust is everything.
A Practical Framework for Building Medical AI Models
Building an AI model for a medical setting isn't just a coding exercise. It’s a highly disciplined, cyclical process designed to ensure the final tool is safe, effective, and something a clinician can actually rely on. This whole system, often referred to as Machine Learning Operations (MLOps), provides a structured path from a rough idea to a fully deployed clinical tool. Navigating this journey correctly is complex and calls for specialised AI software development services that genuinely understand the unique pressures and standards of healthcare.
The MLOps lifecycle in healthcare always starts with a deep dive into the clinical problem you're trying to solve. From there, it moves to the painstaking work of collecting and preparing high-quality, relevant data; this is the fuel for any AI model. Without clean, well-curated data, even the most sophisticated algorithm is destined to fail.
The Core Stages of Medical AI Development
Once your data is in good shape, the real work on the model can begin. This means choosing the right kind of algorithm, training it on your dataset, and then putting it through its paces with rigorous testing. This is never a one-shot deal; it's an iterative loop of training, testing, and tweaking until the model consistently hits the required accuracy and safety benchmarks.
A huge challenge here is wrestling with the unique quirks of medical data. For instance, datasets are often wildly imbalanced. You might have thousands of scans showing healthy tissue for every single one that shows a rare, but critical, disease. You need to use specific techniques to stop the model from simply learning to ignore those rare cases.
The goal is to build a model that doesn't just perform well on paper but makes clinically valid and trustworthy predictions in the real world. This requires a focus on explainability, ensuring clinicians can understand why the AI reached a particular conclusion.
This infographic breaks down the foundational principles for building AI that is both secure and ethical, zeroing in on anonymisation, consent, and explainability.
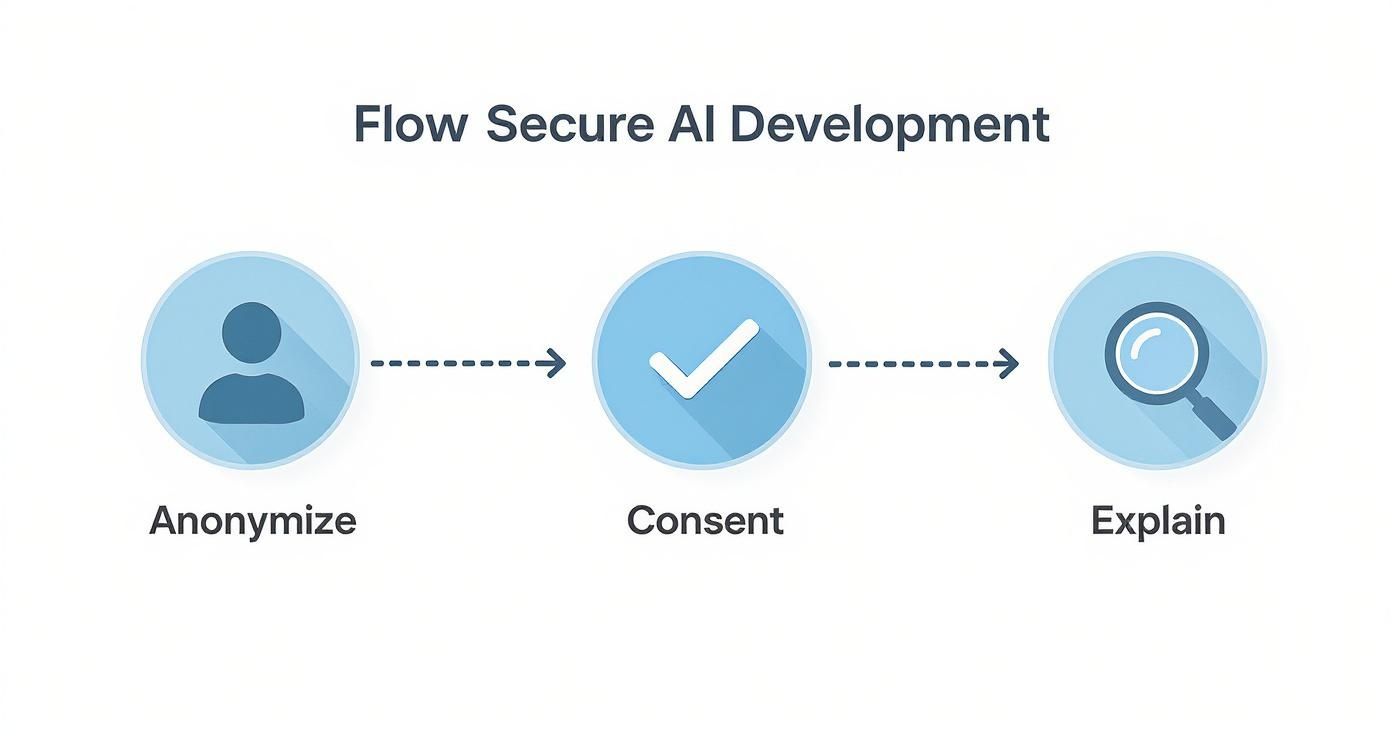
The process it shows is essential for building trust. When you put patient privacy and transparency first, you create a solid foundation for a reliable medical AI system.
Rigorous Validation and Clinical Proof
After a model is trained and performs well in a controlled "lab" environment, it has to face a gauntlet of strict validation. This is where the world of medical software development really separates from other industries. Validation isn't just about checking for bugs in the code; it involves multiple layers of intense scrutiny.
Technical Validation: This first step confirms the model’s predictive accuracy, precision, and other statistical metrics using a completely separate, "unseen" dataset. It answers the basic question: "Is the model mathematically sound?"
Clinical Validation: Next, the model's outputs are compared against the judgment of human clinical experts. This stage is absolutely critical for proving that the AI's predictions are not just statistically correct but also clinically meaningful and genuinely useful.
Regulatory Approval: Before any deployment, the model – as a component of a medical device – must clear regulatory hurdles from bodies like Health Canada or the FDA. This involves putting together exhaustive documentation on the entire development and validation process.
This multi-stage validation process is non-negotiable for managing risk and ensuring patient safety.
Deployment and Continuous Monitoring
Once a model is validated and approved, it can finally be deployed into a live clinical environment. But the work doesn't stop there. A core principle of MLOps is continuous monitoring to make sure the model's performance doesn't degrade over time. The real world is messy – data can shift, patient populations evolve, and clinical practices change. What worked perfectly during development might become less accurate down the line.
This entire framework, from data collection all the way to ongoing monitoring, is a testament to the engineering discipline needed for AI in medical software development. As we explored in our software development guide, adopting these MLOps best practices is the only way to build systems that aren't just intelligent but also dependable and scalable. This structured approach, a hallmark of high-quality custom software development, is how AI tools truly earn their place in the modern clinic. Our team, which you can learn more about on our About Us page, is dedicated to upholding these essential standards.
Integrating AI into Clinical Workflows
You can have the most accurate AI model on the planet, but if it disrupts how doctors and nurses actually do their jobs, it’s practically useless. The real measure of success for any AI-powered medical software is how smoothly it fits into the fast-paced, high-stakes environment of a hospital or clinic.
If a tool adds extra clicks, forces clinicians to jump between screens, or just complicates an already demanding workflow, it will be quickly cast aside.
The ultimate goal is to make the AI feel almost invisible. It should be a natural extension of the tools clinicians rely on every day, like Electronic Health Records (EHRs) and Picture Archiving and Communication Systems (PACS). The insights from the AI need to pop up exactly when and where they’re most valuable, without creating any friction.
Overcoming Data Silos and Legacy Systems
One of the biggest roadblocks in healthcare tech is that crucial patient data is often locked up in different, disconnected systems. These "data silos" make it impossible to get a complete picture of a patient's health. They also starve AI models of the comprehensive data they need to perform at their best.
True integration is about tearing down these digital walls. This is where interoperability standards become absolutely critical for any medical software project.
HL7 (Health Level Seven): This is the classic, long-established set of standards for swapping clinical and administrative data between different software systems.
FHIR (Fast Healthcare Interoperability Resources): As a more modern standard, FHIR leverages web-based tech to make data exchange far simpler and more flexible. It’s perfect for integrating with mobile apps and cloud-based AI.
By building with these standards, developers can create a solid bridge between a new AI tool and a hospital's existing EHR, ensuring information flows securely and without a hitch. We dive deeper into how this works in our article on AI-driven EHR solutions for modern healthcare.
The User-Centred Design Imperative
But technology alone isn't the whole story. The secret to creating tools that clinicians will actually embrace is a relentless focus on user-centred design. This means bringing doctors, nurses, and other healthcare staff into the design and testing process right from the start.
You can't design a great clinical tool from an ivory tower. You have to get into the trenches and understand the real-world pressures, workflows, and pain points of the people who will be using it every single day.
When you co-create solutions with the people on the front lines, you guarantee the final product solves a real problem in a way that feels helpful and intuitive, not like another burden.
This user-first approach is especially vital in Canada, where the health tech sector is growing rapidly. The percentage of Canadian healthcare businesses planning to adopt AI was expected to more than double by 2025, jumping from 11.4% to 23.2%. This growth is fuelled by AI in diagnostics and remote care – areas that absolutely depend on trust and seamless interoperability. To scale these innovations, you need a deep understanding of the unique operational challenges within Canadian health systems.
In the end, successful AI integration isn't about flashy features. It's about thoughtful, empathetic design that respects the realities of the healthcare frontline.
Building Your Strategic AI Roadmap
Moving from AI theory to real-world application demands a clear, well-thought-out plan. For healthcare leaders, bringing AI into medical software development isn't just about grabbing the latest tech. It's about fundamentally improving patient care and making your operations smarter and more efficient. A winning strategy starts by defining success in terms that go beyond a simple financial return.
The true return on investment (ROI) for medical AI is ultimately measured in better patient outcomes, not just dollars saved. Your key performance indicators should focus on things like lower diagnostic error rates, higher patient satisfaction scores, and reduced clinician burnout. When you frame the business case around these tangible improvements, it resonates with everyone, from the boardroom to the front-line clinic staff.
Defining Your Implementation Path
A phased approach is the smartest way to manage risk and show value early on. Forget about a massive, organisation-wide overhaul. Instead, kick things off with a targeted pilot project that solves a specific, high-impact problem. This could be as simple as automating a repetitive administrative task or implementing a diagnostic aid in a single department.
This step-by-step process lets you:
Test and Validate: You can confirm the AI solution actually works as expected in a controlled, real-world setting.
Gather Feedback: It's a chance to collect crucial insights from clinicians to refine the tool and make sure it genuinely meets their needs.
Build Momentum: A successful pilot project is your best tool for getting broader buy-in to scale the solution.
Getting clinicians on board is absolutely critical. Interestingly, recent survey data shows that patient and provider comfort with AI in Canada is on the rise, particularly when it’s tied to positive digital health experiences. And while younger Canadians might know more about AI, older Canadians are often more comfortable with its use for health monitoring and diagnostics. This really underscores the need to build trust across every demographic. You can read the full research about these demographic findings here.
Securing Buy-In and Managing Change
Successfully weaving AI into your workflows is as much about people as it is about technology. Any new medical software development project introduces organisational change, and managing that requires transparent communication and strong leadership. Your stakeholders need to understand not just what the AI does, but why it matters – how it will lighten their workload and lead to better patient outcomes.
The most effective AI adoption strategies are built on a foundation of collaboration. By involving clinicians, IT staff, and administrative leaders from the very beginning, you transform a top-down mandate into a shared mission for better healthcare.
This journey calls for a partner with deep expertise in both the technology itself and the unique complexities of the healthcare sector. At Cleffex, our background in custom software development and our forward-thinking approach to AI software development services mean we’re perfectly positioned to guide your organisation through every stage. As our About Us page highlights, we're all about building solutions that deliver real-world, measurable value.
Frequently Asked Questions
When it comes to bringing AI into medical software development, a lot of questions pop up for hospital leaders, doctors, and developers alike. Getting clear, straightforward answers is the first step toward building confidence and making smart decisions. Here are some of the most common things we get asked.
How Do You Ensure AI Algorithms in Medical Software Are Not Biased?
This is easily one of the most important and toughest challenges we face. Bias isn't always obvious; it can quietly find its way into a model if the data used to train it doesn't reflect the real-world diversity of patients. For instance, an algorithm trained mostly on data from a single demographic group could fail spectacularly when used with others.
Tackling this requires a constant, multi-pronged effort.
Diverse and Representative Data: It all starts here. We have to be obsessive about gathering high-quality, balanced datasets that account for real-world differences in age, gender, ethnicity, and other crucial factors.
Rigorous Auditing: You can't just "set it and forget it." The models need to be checked and re-checked for biased outcomes across different patient groups, both before they go live and long after.
Explainable AI (XAI): We use XAI methods to peek under the hood. This helps everyone – from developers to clinicians – understand why an AI made a certain prediction, making it much easier to catch and fix flawed or biased logic.
What Is the First Step for a Hospital Looking to Implement an AI Solution?
My advice is always the same: start small, but aim for a big impact. Don't try to boil the ocean by overhauling your entire system at once. Instead, pinpoint a specific, nagging problem where AI could make a tangible difference. This might mean streamlining the appointment booking chaos, automating the initial read of certain medical images, or flagging patients who are at high risk of being readmitted.
The best way to begin is with a well-defined pilot project. This approach lets you prove the technology’s value on a small scale, get essential feedback from your clinical team, and build a rock-solid business case for rolling it out more widely. It’s a low-risk strategy for learning and showing real results.
How Does AI Impact the Roles of Healthcare Professionals?
AI is a tool, not a replacement. Think of it as an incredibly capable assistant that frees up doctors and nurses from repetitive, data-heavy work so they can focus on what they do best: complex clinical thinking and caring for patients.
For example, an AI can scan millions of patient records in seconds to pull up a crucial piece of information or highlight a barely perceptible anomaly on a scan that a busy radiologist might miss. This saves a huge amount of time, lessens the mental strain on clinicians, and ultimately helps combat burnout. The goal is always to augment human expertise, not replace it, especially in something as nuanced as medical software development.
What Are the Biggest Security Risks with AI in Healthcare?
When you’re dealing with AI, the security stakes are incredibly high, mostly because of the sensitive patient data involved. One of the most serious threats is something called an adversarial attack, where someone deliberately feeds the AI bad or misleading data to fool it into making a wrong diagnosis. Another major concern is a massive data breach, which becomes a bigger risk when you pool large datasets for training.
This is why rock-solid cybersecurity measures are non-negotiable. We rely on things like end-to-end encryption and advanced techniques like federated learning (where the model trains on local data without it ever leaving the hospital) to keep information safe. Building secure, trustworthy systems is at the very heart of quality AI software development services and a foundational principle for any custom software development project. You can read more about our approach and our team's dedication on our About Us page.