When you’re staring at a complex scan, you know the immense pressure to find those subtle, critical details. Now, imagine an expert co-pilot working alongside you, tirelessly scanning every single pixel and highlighting potential issues for you to analyse with your clinical expertise. That’s the practical reality of AI in radiology today.
The New Co-Pilot in Medical Imaging

Let's be clear: artificial intelligence isn't here to replace the expert radiologist. It's here to augment their abilities. Think of it less like an autopilot and more like a highly advanced co-pilot, capable of processing huge amounts of data at incredible speeds to support the final decisions made by a trained professional. This technology is a powerful safety net and a serious efficiency booster.
At its core, AI in radiology works by training sophisticated algorithms on thousands, or even millions, of labelled medical images. These systems learn to recognise patterns, anomalies, and anatomical structures within scans like X-rays, CTs, and MRIs. The process isn't all that different from how a junior radiologist learns by reviewing countless cases under supervision except the AI can do it on a massive scale without ever getting tired.
Augmenting Human Expertise
The main goal is to empower clinicians, not replace them. For instance, an AI algorithm might flag a tiny lung nodule on a chest CT that could be an early sign of cancer. Or it might detect subtle signs of a stroke on a head scan just moments after it’s taken. The radiologist then steps in, applying their extensive clinical knowledge and understanding of the patient's history to interpret these AI-generated findings.
This human-machine collaboration directly addresses some of the biggest challenges in the field today:
Managing Volume: The number of imaging studies is always climbing, putting enormous pressure on radiology departments. AI helps manage this crushing workload by prioritising urgent cases and automating routine measurements.
Reducing Burnout: By taking over repetitive tasks, AI frees up radiologists to focus their cognitive energy on complex diagnostic puzzles and patient care, which can help reduce professional fatigue.
Enhancing Accuracy: Think of AI as a second set of eyes. It consistently and objectively flags potential abnormalities that might otherwise be missed due to human factors like fatigue or a simple perceptual error.
By shifting the focus from manual detection to expert interpretation and validation, AI enables radiologists to perform at the top of their licence. The technology handles the laborious "search" function, freeing up the human expert for the critical "analysis" function.
This relationship is a powerful example of how technology is being thoughtfully woven into clinical practice. It’s a central theme in the wider discussion around artificial intelligence in healthcare, which is all about building systems that support, rather than supplant, medical professionals.
In this guide, we'll dig into exactly how these tools are improving diagnostic capabilities, making workflows more efficient, and ultimately leading to better outcomes for patients.
How AI is Reshaping Radiological Workflows
The idea of artificial intelligence in radiology isn't some far-off future concept; it's happening right now, fundamentally changing how modern medical imaging departments operate day-to-day. To really grasp its impact, let’s follow the path of a patient's scan and see how AI in radiology helps clinicians at every single step, from the moment the image is taken to the final report. The ultimate aim is to create a workflow that’s more efficient, more accurate, and less overwhelming for everyone.
This whole process kicks off the second a patient is on the scanner. AI tools can now optimize image acquisition protocols on the fly, adjusting scanner settings in real-time. This means we get the highest quality images possible with the lowest radiation dose, all tailored specifically to that patient's body.
Once the images are captured, the next big hurdle is the worklist. In any busy hospital, hundreds of scans can pile up, and they aren't all equally urgent. This is where AI-driven triage systems have become a game-changer.
Prioritising Critical Cases
Think of an AI triage algorithm as an incredibly fast initial screening. It automatically scans every single study that comes in, looking for red flags. The system has been trained to spot the tell-tale signs of conditions where every second counts.
For instance, it might immediately flag a head CT with signs of a brain bleed or a chest scan showing a potential pulmonary embolism. These high-stakes cases are then automatically bumped to the very top of the radiologist’s worklist.
This immediate prioritisation can shave critical minutes, or even hours, off the time to diagnosis for the most urgent cases. It ensures that patients who need immediate attention get it, fundamentally changing the "first-in, first-out" model of traditional radiology queues.
This automated sorting doesn't just help in emergencies. It also helps balance the department's entire workload, cutting down on bottlenecks and giving radiologists a much more manageable pace throughout their day.
Assisting with Image Interpretation
When it's time for the radiologist to interpret the images, AI acts like a tireless second pair of eyes. It meticulously analyzes the scan to segment organs, measure anatomical structures, and, most importantly, highlight suspicious areas that need a closer look. This kind of support is invaluable for catching subtle abnormalities that the human eye might miss, especially at the end of a long shift.
Here are a few common ways AI helps during interpretation:
Nodule Detection: Identifying and characterizing tiny nodules in the lungs on a chest CT scan.
Lesion Highlighting: Flagging suspicious lesions in mammograms that could point to early-stage breast cancer.
Volumetric Analysis: Automatically calculating the volume of a brain tumour or measuring changes in heart function from cardiac MRIs.
This infographic breaks down the basic flow of how AI takes imaging data and turns it into something that supports a clinical decision.
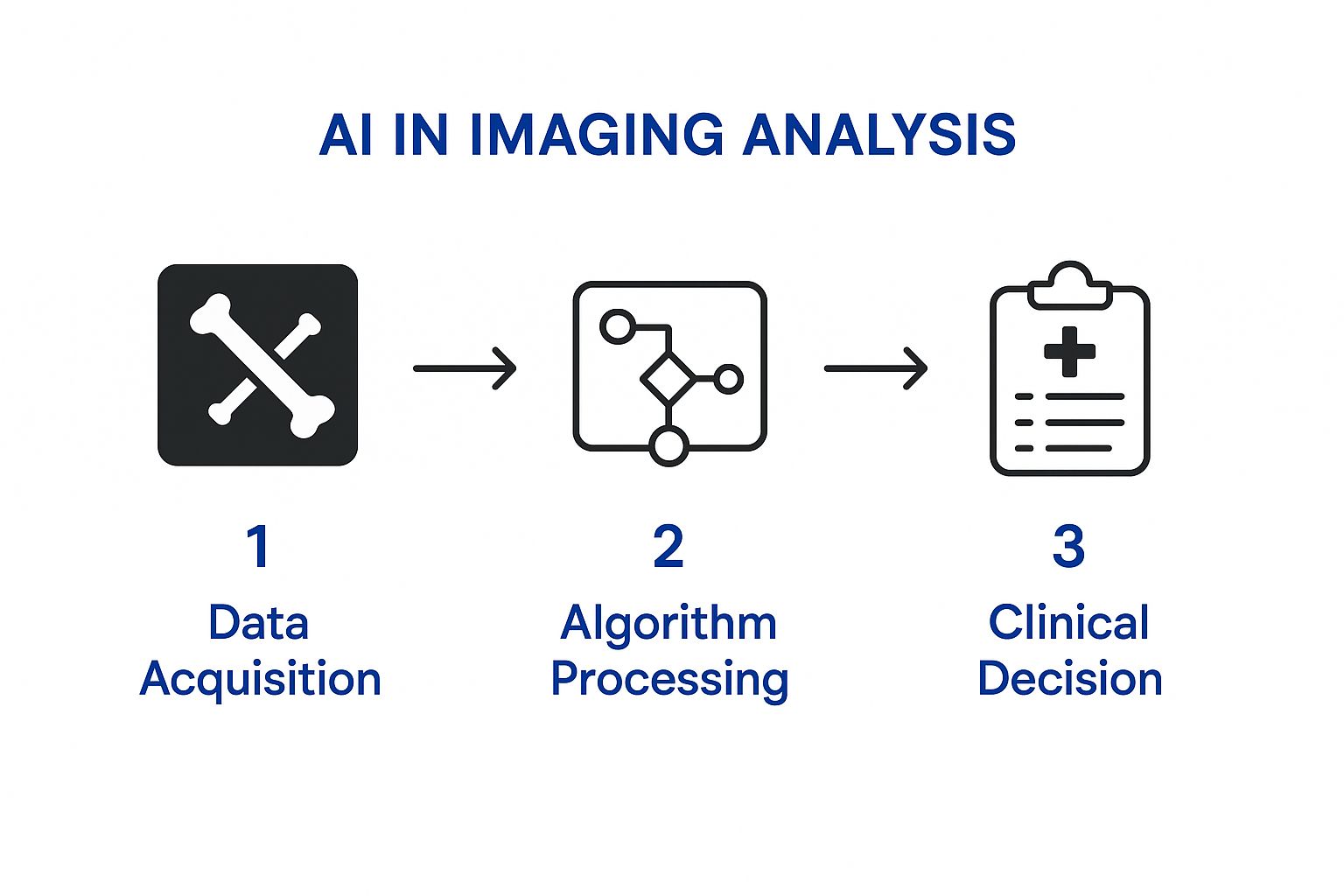
As you can see, the process is simplified into three key stages: raw data is acquired, an algorithm processes it, and then the output is presented as actionable information to help the radiologist make their final judgment.
Finally, AI even lends a hand during the reporting stage. It can auto-populate reports with standard measurements, findings, and other routine data. This doesn't just make reporting faster; it also makes it more consistent and cuts down on the risk of typos. By taking care of these repetitive tasks, AI frees up radiologists to focus their expertise on complex analysis and communicating their findings effectively.
The principles behind these improvements aren't just limited to medicine. For a broader look at how these systems streamline operations in other fields, it's worth exploring general strategies for optimizing workflows with AI. This rapid adoption in radiology is backed by serious regulatory momentum. By June 2025, the United States saw 777 artificial intelligence-enabled medical devices receive clearance from the U.S. Food and Drug Administration (FDA), with about two-thirds of U.S. radiology departments using AI in some form.
Core Applications of AI in Modern Radiology

The real strength of AI in radiology isn't as a single, all-purpose tool. Think of it more like a specialist's toolkit, filled with highly specific instruments designed to solve distinct clinical problems in different areas of medical imaging. We can really see its value when we look at how these applications are improving diagnostic certainty and patient care right now.
AI is already making a difference everywhere, from spotting the earliest signs of cancer to speeding up diagnoses in the emergency room. For each application, there's a clear clinical challenge, an intelligent solution, and a direct benefit to the patient, highlighting just how versatile and life-saving this technology can be.
Enhancing Cancer Detection in Oncology
In oncology, everything hinges on early and accurate detection. AI algorithms are proving to be fantastic assistants, trained to identify subtle patterns that might indicate a developing malignancy. They act like a digital magnifying glass, helping radiologists pinpoint abnormalities that are often too small or faint for the human eye to reliably catch on its own.
Take lung cancer screening, for instance. A radiologist has to meticulously go through hundreds of CT scan slices, searching for tiny nodules that could be cancerous. It's a demanding task.
An AI tool can pre-scan these images in seconds, flagging every single suspicious nodule. It can even provide an initial analysis of a nodule's size and density. This doesn't take the final decision away from the radiologist; instead, it sharpens their focus, ensuring even the most subtle findings get the attention they deserve. We're seeing the same thing in mammography, where AI helps detect faint calcifications or tissue distortions that are tell-tale signs of early-stage breast cancer.
Accelerating Treatment in Neurology
When a patient has a stroke or a serious head injury, every second counts. As the saying goes, "time is brain." The faster the diagnosis, the better the chance of a good recovery. This is where AI’s speed offers a huge clinical advantage, especially in a busy emergency department where radiologists are juggling a long list of critical scans.
AI tools designed for head CT scans can almost instantly detect signs of a brain bleed (intracranial hemorrhage). As soon as a bleed is found, the system immediately flags the study and sends an alert to the radiologist and the on-call stroke team. This simple step can shrink the time to treatment from hours down to just minutes, a delay that can be the difference between a full recovery and a lifelong disability.
This isn't just about being faster; it's about fundamentally redesigning the emergency response. By automatically pushing the most critical cases to the top of the reading list, AI ensures the sickest patients get immediate expert attention, which directly improves survival rates and long-term outcomes.
This rapid identification and prioritization is a perfect example of how AI in radiology is creating a more responsive and effective diagnostic environment for conditions where time is of the essence.
Precision Analysis in Cardiology
The heart is an incredibly complex, three-dimensional organ that’s always in motion. This makes cardiac imaging one of the trickiest areas in radiology. To assess how well a heart is functioning from an MRI, clinicians have to perform detailed, time-consuming manual measurements of chambers, walls, and blood flow. Not only is this slow, but the results can also vary from one person to another.
AI is now automating this entire process with remarkable precision. It can perfectly outline the heart's chambers on an MRI, calculate the ejection fraction (a vital indicator of heart health), and measure blood flow with a consistency that's nearly impossible to achieve by hand.
This automation brings a few key benefits to the table:
Greater Accuracy: AI delivers objective, repeatable measurements. This reduces the variability between different readers and leads to more dependable diagnoses.
Time Savings: A task that might have taken a radiologist or cardiologist 30 minutes or more can now be done in just a few minutes, freeing them up to focus on patient care.
Deeper Insights: By analysing subtle textures and motion patterns the human eye can't see, AI can uncover early signs of heart disease that traditional methods might miss.
This table gives a quick overview of how these tools are being applied across different specialties.
Key AI Applications Across Radiology Specialties
Specialty | AI Application | Primary Benefit to Patient Care |
|---|---|---|
Oncology | Nodule/lesion detection in CT & mammograms | Earlier cancer detection results in reduced miss rates for subtle findings. |
Neurology | Intracranial hemorrhage detection, stroke triage | Drastically reduced time-to-treatment for life-threatening conditions. |
Cardiology | Automated cardiac function measurements (e.g., ejection fraction) | More accurate and consistent assessment of heart health, faster diagnosis. |
Musculoskeletal | Fracture detection on X-rays | Improved accuracy in busy emergency rooms, prioritizing urgent cases. |
Abdominal Imaging | Organ segmentation, liver/spleen volume measurement | Precise monitoring of disease progression and treatment response. |
From spotting tiny tumours to measuring heart function, AI is helping turn complex medical images into clear, actionable data.
These developments are part of a much larger shift toward using intelligent systems for early diagnosis. To see how these ideas are applied more broadly, you can learn more about how specialists are using predictive healthcare with AI to get ahead of patient needs. Ultimately, whether in oncology or cardiology, the goal is the same: empower clinicians to make better, faster decisions for their patients.
The Real Hurdles to AI Implementation
Bringing AI into a radiology department isn’t like installing a new piece of software. It’s a fundamental change to how a healthcare organization operates, and while the potential is enormous, the road to getting it right is lined with serious challenges that demand careful thought.
The first, and often most frustrating, stumbling block is a technical one: integration. An AI tool is completely useless if it can't talk to the hospital's existing systems. We’re talking about connecting it seamlessly with the Picture Archiving and Communication Systems (PACS) and Radiology Information Systems (RIS) that form the digital backbone of the entire imaging department.
The Technical and Data Minefield
Making that connection work often takes a surprising amount of IT muscle and custom development. Get it wrong, and you create clunky, inefficient workflows that completely undermine the point of using AI.
This technical headache is tied directly to data. AI algorithms are hungry for huge volumes of clean, well-organized data to work properly. Ensuring your data is compatible, secure, and ready for the AI is a massive project in itself. Patient privacy, of course, is absolutely paramount. Any new system handling sensitive health information must have rock-solid security and comply with regulations like PHIPA in Canada.
Beyond the Wires: Clinical and Financial Realities
Even if the tech is perfectly integrated, you run into the "black box" problem. Many powerful deep learning models are so complex that it's not always obvious how they concluded. For a clinician, this lack of transparency is a huge barrier to trust.
Radiologists have to stand behind their diagnoses. If they can't understand the reasoning behind an AI's suggestion, how can they confidently rely on it? This need for explainable AI isn’t just about trust; it’s about accountability and medico-legal responsibility.
The true measure of an AI tool isn’t just its accuracy. It’s whether it can be a transparent, trusted partner in the diagnostic process. If a radiologist can’t understand the ‘why,’ the tool becomes a liability, not an asset.
Then there’s the money. The price tag for AI goes far beyond the initial software licence. You have to factor in:
Infrastructure Upgrades: Beefing up servers, storage, and networks to handle the processing demands.
Integration Fees: The cost of getting the AI to play nicely with your existing PACS, RIS, and electronic health record (EHR) systems.
Ongoing Maintenance: The reality of subscription fees, tech support, and essential software updates.
The People Problem
Finally, and perhaps most importantly, you have to manage the human element. Integrating AI isn't a tech project; it's a culture-change project. It requires continuous training to help radiologists adapt to a new way of working.
Their role is shifting from interpreting every single image to overseeing sophisticated diagnostic systems, allowing them to focus their deep expertise on the most complex cases and validating what the AI finds. This transition needs dedicated training programs so clinicians feel comfortable and capable with the new technology.
Without genuine buy-in from the people on the front lines, even the most advanced AI will just gather digital dust. The ethical dimensions of this shift are also critical, a topic that deserves its own focus within the broader conversation on ethics and AI in healthcare. Successfully navigating this mix of technical, financial, and human challenges is what separates a failed pilot project from a truly integrated clinical tool.
The Future of Radiology and Next-Generation AI

The evolution of AI in radiology is pushing beyond just finding what's already there. We're moving from simple detection to intelligent prediction. While today’s tools are incredibly good at spotting existing abnormalities, the next wave of AI is all about forecasting what happens next. This shift is set to turn radiology from a reactive field into a proactive, preventative cornerstone of modern medicine.
Think about an AI that doesn't just flag a tumour, but instead analyzes its deep biological makeup right from the initial scan. This system could predict how fast that specific tumour might grow or even how it will respond to various treatments. This is the whole idea behind radiomics, where AI pulls out huge amounts of quantitative data from images, details completely invisible to the human eye.
This kind of insight takes patient care to a whole new level of personalization. Instead of starting with broad, one-size-fits-most treatment protocols, doctors could use these AI predictions to pick the most effective therapy for a specific patient right from the get-go. That could save critical time and lead to much better outcomes.
Making AI Smarter and More Accessible
One of the biggest hurdles in developing powerful AI has always been the need for massive, centralized datasets, which naturally brings up major patient privacy issues. To get around this, researchers are championing a clever approach called federated learning.
Here's a simple way to picture it: instead of moving all the sensitive patient data to one central place to train a single algorithm, the algorithm itself travels to each hospital. It learns from the local data safely behind the hospital's firewall, then only sends back the general patterns it learned, never the private patient information. This happens over and over again at different institutions.
This collaborative model lets us build incredibly robust and accurate AI without ever exposing patient data. It also levels the playing field, allowing smaller hospitals with less data to contribute to and benefit from the same advanced tools.
The future isn't just about more powerful algorithms; it's about smarter, more secure ways of training them. Federated learning will accelerate innovation by creating a collaborative ecosystem where institutions can pool their knowledge without ever pooling their sensitive data.
Breakthroughs in data efficiency are also making AI in radiology more practical. Researchers at the University of California, San Diego (UCSD) developed an AI tool that drastically improves medical image segmentation. Their method cuts down the need for huge, expertly labelled datasets by up to 20 times. This is a huge win for healthcare systems, especially in places like Ontario and British Columbia, that want to adopt AI without a massive upfront investment. You can discover more about how this innovation helps clinics by reading the full story on their research.
These advancements, predictive analytics, federated learning, and more data-efficient models, aren't just science fiction. They are the real building blocks for the next era of medical imaging, where AI will give clinicians a glimpse into a patient's future health, empowering them to act on it today.
Frequently Asked Questions About AI in Radiology
As AI becomes a bigger part of the conversation in radiology, a lot of practical questions are coming up from clinicians and administrators alike. Getting a handle on what this technology really means for daily practice is the first step toward making smart decisions. Let's tackle some of the most common ones.
Will AI Replace Radiologists?
The short answer is no. The consensus among experts is clear: AI is here to assist, not to replace. Think of it this way: AI is fantastic at highly specific, repetitive tasks, like spotting a tiny nodule or measuring a lesion. It can sift through massive amounts of data in seconds.
But AI can't grasp the full clinical picture. It doesn't understand a patient's history, communicate with empathy, or apply the kind of nuanced, critical thinking that comes from years of experience. The future isn't AI instead of radiologists; it's radiologists empowered by AI. It's a co-pilot, handling the tedious work so the human expert can focus on complex diagnoses and patient care.
What is the Biggest Barrier to AI Adoption?
Surprisingly, it’s not always the algorithm itself. The single biggest hurdle is often the technical heavy-lifting of getting a new AI tool to play nicely with a hospital's existing systems.
Every radiology department runs on a Picture Archiving and Communication System (PACS) and a Radiology Information System (RIS). If a new AI solution doesn't integrate smoothly into that existing workflow, it can cause more headaches than it solves. A clunky system just adds clicks and frustration, completely wiping out any potential gains in efficiency.
Overcoming this integration challenge is paramount. A successful rollout is as much about change management, training staff and adapting routines, as it is about the technology itself.
How Are AI Radiology Tools Validated for Clinical Use?
An AI tool can't just be plugged in and used on patients. Before it ever reaches a clinic, it has to go through an incredibly rigorous validation and regulatory process. In Canada, this means getting the green light from Health Canada, a process similar to the FDA's role in the United States.
Developers have to provide a mountain of evidence from clinical trials demonstrating that their algorithm is both safe and effective for its specific job. This ensures that any tool used in patient care has met strict standards for accuracy and reliability. For radiologists trying to keep up with the latest validated tools, resources like an AI research paper summarizer can be a huge time-saver for digesting new studies and findings.
At Cleffex Digital Ltd, we specialise in developing secure, compliant, and intelligent software solutions that address the real-world challenges of the healthcare industry. Discover how our expertise can support your digital transformation by visiting https://www.cleffex.com.