The digital transformation of healthcare is far more than just swapping paper files for computer screens. It’s a complete overhaul of how healthcare is delivered, moving from a system of isolated, manual processes to a fully connected, data-driven ecosystem. At its heart, this shift is about using digital tools, like secure apps, artificial intelligence, and cloud data, to make patient care smarter, faster, and more personal.
The New Reality of Patient Care

Picture two clinics. In the first, patient charts are piled high on desks, phones ring endlessly for appointments, and critical lab results arrive slowly by fax. In the second, a patient checks in using a tablet, the doctor instantly pulls up a comprehensive digital health history, and follow-up care is coordinated through a secure patient portal.
This isn't a glimpse into the future; it's the reality of healthcare's digital evolution happening right now. It mirrors how banking moved from long teller lines to powerful mobile apps. The service is the same, but the delivery is built around convenience, instant data access, and putting the user first.
From Paper Files to Digital Ecosystems
The traditional healthcare model was inherently fragmented. A patient's medical history was often scattered across various specialists' offices in thick, cumbersome folders. This created dangerous information gaps and frustrating inefficiencies.
Today's digital approach connects those scattered dots into a single, cohesive health story. This fundamental change is built on a few key pillars:
Data on Demand: Moving information from locked filing cabinets to secure, cloud-based Electronic Health Records (EHRs) that authorised clinicians can access anytime, anywhere.
Smarter Communication: Shifting from endless phone tag to automated Health Care SMS reminders, online patient portals, and direct, secure messaging.
Care Beyond Clinic Walls: Expanding services through telemedicine consultations, remote monitoring with wearable devices, and mobile health apps that empower patients to manage their own well-being.
The real change isn’t just about installing new software. It’s about completely rethinking workflows to be more proactive and patient-centred, which ultimately leads to better health outcomes and a more sustainable system.
To give you a clearer picture of this shift, let's compare the old way with the new.
Healthcare Evolution At a Glance
The following table breaks down how specific aspects of healthcare are changing, making it easy to see the direct benefits of going digital.
| Healthcare Aspect | Traditional Approach | Digital Approach |
|---|---|---|
| Patient Records | Paper charts, siloed in one office, prone to loss or damage. | Centralised EHRs are accessible to all authorised providers. |
| Appointments | Phone calls, manual scheduling, paper reminder cards. | Online booking, automated SMS/email reminders, and calendar sync. |
| Consultations | In-person visits are required for nearly all interactions. | Telehealth video calls for routine check-ins and consultations. |
| Prescriptions | Handwritten scripts, potential for errors, and physical pickup. | E-prescriptions are sent directly to the pharmacy, reducing errors. |
| Patient Monitoring | Reliant on in-clinic visits for vital sign checks. | Wearable devices and IoT sensors for continuous remote monitoring. |
| Communication | Phone calls, often leading to delays and miscommunication. | Secure patient portals for messaging, lab results, and education. |
This table highlights just how deep the changes run. Every touchpoint in the patient journey is being reimagined for efficiency and effectiveness.
This guide will walk you through this essential evolution. We'll explore the core technologies driving this change, the strategies that ensure successful adoption, and how it all comes together to create a smarter, more connected healthcare system. To get a head start, you can learn more about how patient engagement technology in healthcare is already reshaping modern medicine.
Understanding the Forces Driving This Change
The big shift toward digital healthcare isn’t happening in a vacuum. It's really the result of several powerful currents all converging at once, creating an undeniable momentum for change. It’s less of a single decision and more of a necessary response to where the world is heading.
One of the biggest drivers? Patient expectations have completely changed. Today’s patients are also consumers, used to the seamless, on-demand experiences they get from banking or shopping online. They now expect that same level of convenience from their healthcare providers, everything from booking an appointment online to getting instant access to their own health records. This demand for a more consumer-friendly model is a major reason organisations are being pushed to modernise.
The Rising Tide of Internal Pressures
At the same time, healthcare systems are grappling with immense internal strain. Skyrocketing operational costs and widespread staff burnout have made finding efficiencies a matter of survival. Old-school, paper-based processes aren't just slow; they're expensive and riddled with potential for error. Digital tools offer a direct path forward by automating tedious admin tasks, improving communication, and letting clinicians focus more on patients instead of paperwork.
This isn't just about plugging in new technology. It's about fundamentally re-engineering how healthcare systems work to get three things right: improving the patient experience, delivering better clinical outcomes, and running a more efficient operation.
The COVID-19 pandemic threw gasoline on this fire. Almost overnight, virtual care went from a nice-to-have service to an absolute necessity. This forced the rapid adoption of telemedicine, remote patient monitoring, and digital communication tools, proving they could work on a massive scale. The crisis effectively shattered years of resistance and showed just how resilient a digital-first approach could be.
Data As the New Frontier in Medicine
Beyond these immediate pressures lies an even bigger opportunity: the power of data. As healthcare goes digital, it unlocks vast amounts of information that were previously stuck in filing cabinets. By using data analytics and artificial intelligence, providers can finally move from a reactive model of simply treating sickness to a proactive and even predictive one.
This data-driven approach opens up incredible possibilities:
Predictive Analytics: We can now identify patients at high risk for certain conditions long before symptoms even appear.
Personalised Medicine: Treatments can be tailored to a person’s unique genetic profile and lifestyle.
Population Health Management: It's easier to spot public health trends and direct resources where they’ll have the most impact.
You can see this playing out right here in Canada. The country's digital health market is booming, largely driven by the huge demand for telemedicine and remote monitoring services. With nearly everyone having a smartphone and reliable internet, mobile health apps and online doctor consultations have become a reality for millions. This trend is also being helped along by government initiatives aimed at controlling rising healthcare costs. You can find more detailed insights on Canada's digital health growth on Statista.
When you combine patient demand, internal pressures, and the sheer potential of new technology, the case for the digital transformation of healthcare becomes impossible to ignore.
The Core Technologies Powering Modern Medicine
The shift to digital healthcare isn't about flipping a single switch; it's more like an orchestra, where a whole range of interconnected technologies have to work in harmony. To really grasp this change, you need to understand what each instrument does. Every piece of this puzzle plays a crucial role in building a healthcare system that's more intelligent, responsive, and ultimately, focused on the patient.
Think of these technologies as a team of specialists, each bringing a unique skill to the table. From creating a single, reliable source for a patient's entire medical history to delivering care right into someone's living room, these tools are the backbone of this new era in medicine.
Let's break down the key players driving this change.
Electronic Health Records: The Central Nervous System
At the very heart of it all, you have Electronic Health Records (EHRs). An EHR is so much more than a digital version of an old paper chart; it’s the living, breathing story of a patient's health journey. It pulls together everything from lab results and diagnoses to medications and allergies into one unified, accessible record.
This centralisation is the game-changer. It means every authorised clinician, whether it's a family doctor, a specialist, or an emergency room physician, is working from the same complete and current information. This simple fact helps eliminate dangerous information gaps and dramatically reduces the risk of medical errors.
These systems are now incredibly common. In Canada, for instance, a staggering 95% of physicians in acute care settings rely on EHRs. But while adoption is high, new problems have surfaced. A significant 73% of these physicians point to poor integration between different EHR systems as a major operational headache. You can read more about these findings on EHR adoption and satisfaction in Canada.
Cloud Computing: The Secure Foundation
If EHRs are the nervous system, then cloud computing is the skeleton that supports it all. Cloud platforms provide the secure, scalable, and readily available foundation needed to manage massive amounts of sensitive health data. Instead of being locked away on a local server in one hospital, patient data can be safely accessed by authorised providers from anywhere, at any time.
This is essential for modern healthcare. It’s what makes things like this possible:
Remote Access: Doctors can review patient charts from home or while consulting with specialists in other cities.
Disaster Recovery: Critical patient information is safely backed up, protecting it from physical damage like fires or floods.
Scalability: Hospitals can easily expand their data storage as they grow, without having to buy and maintain expensive new hardware.
AI and Machine Learning: The Intelligent Brain
Artificial Intelligence (AI) and machine learning are the intelligent brain of the digital health ecosystem. These technologies are brilliant at sifting through enormous datasets to find patterns that would be impossible for a human to spot. They are helping shift healthcare from a reactive model to a predictive one.
AI's true power in medicine isn't about replacing doctors. It's about augmenting their expertise, giving them powerful tools to see connections and risks they couldn't see before, ultimately leading to earlier diagnoses and more personalised treatments.
For example, AI algorithms can analyse medical images like X-rays or MRIs to spot early signs of disease, often with incredible accuracy. They can also predict which patients are at high risk for developing conditions like sepsis, giving clinical teams a chance to intervene early. If this area piques your interest, you might find value in our detailed guide on AI-powered healthcare solutions.
Telemedicine and IoT: The Eyes and Ears
Finally, we have telemedicine and the Internet of Things (IoT), which extend the reach of care far beyond the clinic’s walls.
Telemedicine acts as the digital front door. It allows patients to connect with their doctors through video calls for consultations, follow-ups, and mental health support. This has been a lifeline for people in rural areas or for those who have trouble with mobility, dramatically improving their access to care.
IoT devices, such as wearable fitness trackers, smart blood pressure cuffs, and continuous glucose monitors, are 24/7 health monitors. They are the eyes and ears on the ground, collecting a steady stream of real-time data and sending it back to care teams. This continuous monitoring allows for proactive management of chronic conditions, helping catch potential problems before they become emergencies.
Your Strategic Roadmap for Digital Implementation
Jumping into a full-scale digital overhaul without a clear map is a recipe for getting lost. To navigate the complexities of modernising healthcare, you need a structured, strategic roadmap. This isn't about chasing the latest shiny tech; it's a deliberate, phased approach designed to solve real-world problems and create lasting value for patients and staff alike.
A well-defined plan acts as your North Star. It ensures every initiative, whether it's launching a new patient portal or deploying an AI diagnostic tool, aligns perfectly with your organisation's core objectives. It brings clarity to your teams, helps you manage budgets, and keeps the focus exactly where it should be: on improving patient care and operational performance.
The diagram below shows how these modern medical technologies flow together, starting from the moment data is collected and ending with a better patient interaction.
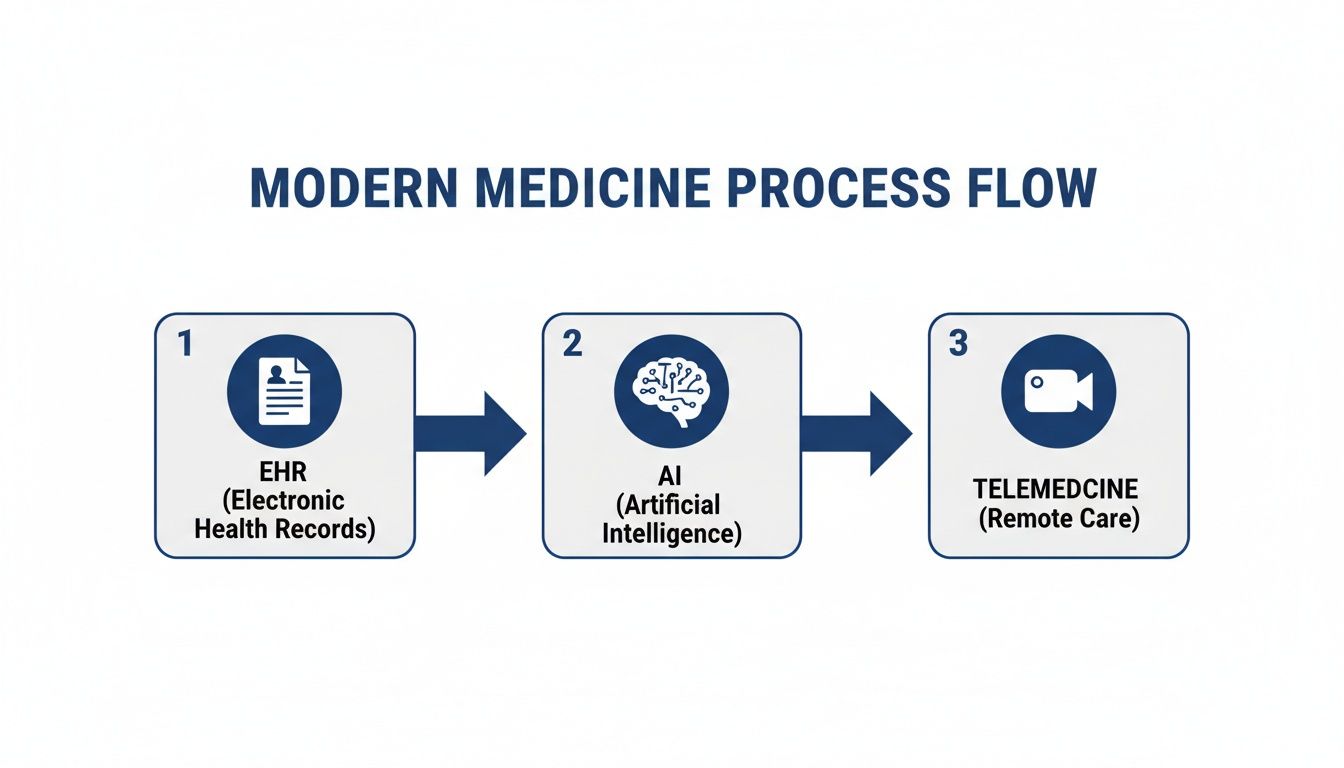
As you can see, foundational EHR data is the fuel for intelligent AI systems. Those systems, in turn, make services like telemedicine much more effective and accessible for the people who need them most.
Phase 1: Assess and Strategise
The very first step is an honest self-assessment. Before you can build the future, you have to get a firm grip on the present. This means taking a hard look at your current processes, legacy systems, and team capabilities to find the most significant pain points holding you back.
Where is the friction? Maybe administrative tasks are burying your clinicians in paperwork. Perhaps patients are frustrated with long wait times or confusing communication. Or it could be that different departments are operating in silos, unable to share critical information. Pinpointing these issues is your starting line.
Once you know the problems, you can set clear, measurable goals. A vague objective like “improve efficiency” is simply not good enough. Instead, get specific:
Reduce patient check-in time by 30% within six months.
Decrease billing errors by 50% in the next fiscal year.
Boost patient portal adoption to 70% within one year.
These concrete targets will guide every decision you make and give you a clear benchmark for what success looks like.
Phase 2: Prioritise and Plan
With your goals locked in, it's time to prioritise. It can be tempting to try to fix everything at once, but that path often leads straight to burnout and blown budgets. The key is to focus on high-impact projects that deliver tangible results early on.
A successful digital transformation is built on momentum. Scoring early victories, like streamlining billing or launching a simple online appointment scheduler, builds confidence and secures buy-in from staff and leadership for the bigger, more ambitious projects ahead.
Next, create a detailed plan outlining the scope, timeline, budget, and resources needed for each project. This is where you manage expectations and get everyone on the same page. For a more structured approach, our guide on creating a technology roadmap template can help keep your projects organised and on track.
Phase 3: Choose Partners and Implement
Picking the right technology partner is one of the most important decisions you'll make. You don't just need a vendor; you need a partner who genuinely understands the unique regulatory and security challenges of the healthcare sector, including compliance with standards like PHIPA in Canada.
Look for a team with proven expertise in healthcare software and a commitment to agile development. An agile approach gives you flexibility. It lets you test, learn, and adapt as you go, rather than getting locked into a rigid plan that can't change with your needs.
The implementation itself must go hand-in-hand with a strong change management strategy. This includes:
Comprehensive Staff Training: Make sure everyone, from front-desk staff to senior surgeons, feels comfortable and capable with the new tools.
Workflow Integration: New technology should fit neatly into daily routines, making jobs easier, not adding another layer of complexity.
Clear Communication: Keep your teams informed about the "why" behind every change, always highlighting how it benefits both them and their patients.
Phase 4: Measure and Scale
The journey isn't over just because a new system is live. The final phase is really a continuous cycle: measure, iterate, and scale. Use the key performance indicators (KPIs) you defined back in phase one to track your progress and see the real-world impact of your work.
Are you hitting your targets for reduced wait times or improved patient satisfaction? This data will tell you what's working and where you might need to make adjustments. This feedback loop is what enables you to refine your strategy and make smart decisions about where to invest next.
Once a project proves its worth on a smaller scale, you can confidently plan to scale it across other departments or facilities, ensuring your growth is both sustainable and truly impactful.
Navigating Common Challenges and Obstacles

Let's be realistic: making big technological shifts in healthcare isn't a walk in the park. Any major change comes with its own set of hurdles that can slow you down or even stop a project in its tracks. The key is to know what they are ahead of time.
Forward-thinking organisations don't see these challenges as stop signs. Instead, they treat them as problems that need to be solved. Facing them with a practical plan is what separates a stalled initiative from a successful one.
Data Security and Regulatory Compliance
The second you move patient information into a digital format, security and compliance have to be your top concerns. Here in Canada, regulations like the Personal Health Information Protection Act (PHIPA) have strict rules about how patient data is managed. A single breach doesn't just lead to huge fines; it can completely shatter patient trust, which is much harder to rebuild.
The only way forward is to build security into the DNA of your systems, not just bolt it on as an afterthought. This means partnering with technology experts who live and breathe healthcare compliance and who design their solutions with security at the very core.
The Interoperability Puzzle
One of the most stubborn technical headaches is interoperability, or, in simple terms, getting different systems to talk to each other. A hospital might have one system for electronic records, another for lab results, and a totally separate one for billing. If those systems can't share information easily, you end up with data silos that defeat the whole purpose of going digital.
The fix is to insist on technologies built on open standards like FHIR (Fast Healthcare Interoperability Resources). Making these standards a requirement ensures that new tools can plug into your existing setup without creating more disconnected islands of data. It’s how you build a connected environment where information flows securely to the right people at the right time.
Managing High Implementation Costs
The price tag for new software, hardware, and training can feel intimidating, particularly for smaller clinics or organisations on a tight budget. The fear of a massive upfront investment often leads to hesitation, which only delays necessary improvements.
A phased, MVP-first (Minimum Viable Product) approach is a smart way to manage these costs. Instead of trying to build the perfect, all-in-one system from day one, you start small. Launch a focused solution that solves one critical problem first. This gets you a quick win, lets you learn from real user feedback, and allows you to reinvest in the next phase, making the financial side much less scary.
The goal isn’t to launch everything at once. It’s to deliver immediate value by solving the most pressing pain point first, then using that success to fuel the next stage of growth.
Overcoming Staff Resistance
Maybe the biggest obstacle isn't technical at all; it's human. Clinicians and admin staff are used to their workflows, and bringing in new technology can be met with scepticism. People worry it will make their jobs more complicated, not less.
This is where good change management comes in. It’s about more than just a one-off training session; it’s a sustained effort to explain the "why" behind the change.
Demonstrate Clear Benefits: Show your staff exactly how a new tool will cut down on their paperwork, save them time, or help them provide better care.
Provide Robust Training: Offer hands-on training tailored to different roles so everyone feels confident with the new systems.
Involve Them in the Process: Ask for feedback. Involve your end-users in choosing and rolling out the technology to give them a real sense of ownership.
By communicating clearly and showing people the real-world benefits, you can turn hesitant staff into your biggest champions for digital change.
Finding the Right Partner to Guide Your Transformation
Tackling a full-scale digital transformation in healthcare is a massive undertaking, and it's not something you should do alone. Think of it this way: when faced with a complex medical case, you bring in a specialist. The same logic applies here. A strategic technology partner can help you move faster, sidestep common pitfalls, and ultimately get more value from your investment.
Choosing this partner is one of the most critical decisions you'll make. You're not just buying a piece of software; you're forging a relationship with a team that has to understand the high-stakes environment of healthcare. They need to speak the language of data security, regulatory compliance, and patient-first design.
What To Look For in a Technology Partner
The right partner is a guide, not just a vendor. They bring a mix of technical know-how and deep industry knowledge that's absolutely vital for success. When you're looking for someone to guide your transformation, it's crucial to find a team with proven expertise in healthcare industry solutions.
Your ideal partner should have a solid track record in a few key areas:
Healthcare Compliance: They absolutely must have experience building secure systems that meet strict Canadian regulations like PHIPA.
Agile Development Practices: An agile approach brings much-needed flexibility. It lets you start with a focused solution and build on it as your needs change and grow.
Custom Software Expertise: One-size-fits-all products rarely work in healthcare. A partner who excels at custom development can create solutions that solve your specific operational headaches.
AI and Cloud Capabilities: To build systems that are both smart and scalable, your partner needs to be an expert in modern tech like artificial intelligence and cloud infrastructure.
A true partner doesn't just build what you ask for; they work with you to solve the right problems. Their goal is to get to the heart of your challenges and design technology that genuinely improves patient outcomes and makes your operations more efficient.
Turning Your Vision into Reality
Let’s get practical. Maybe you need a custom module for your EHR to better track chronic disease management. Or perhaps you're thinking about a simple, intuitive mobile app that lets patients book appointments and see their lab results. Maybe your biggest challenge is just getting an old, clunky data system onto a modern, secure cloud platform.
This is exactly where a strategic partner makes all the difference. Using agile development, they can deliver these kinds of solutions in a way that’s both scalable and affordable. They focus on solving your real-world business problems, whether that’s creating smoother workflows for your staff or building better digital experiences for your patients.
The end goal is to find a team that can help you achieve lasting growth. They bring the technical muscle and strategic thinking needed to turn your vision of a more connected, efficient healthcare system into a reality, ensuring every step you take is secure, compliant, and makes a real impact.
Got Questions? We’ve Got Answers.
Leaping into digital healthcare brings up a lot of questions. It’s a big move, and it's natural to wonder where to start, how to keep data safe, or what it all costs. Let's break down some of the most common concerns we hear from healthcare providers.
What’s the Best First Step for a Small Clinic?
If you’re running a small clinic, the best place to start is with your biggest headache. More often than not, that’s the mountain of administrative work that eats up your day.
Instead of trying to do everything at once, focus on a single, powerful move: adopting a modern, cloud-based Practice Management System (PMS) with a built-in EHR. This one tool can immediately streamline your scheduling, billing, and patient records. It creates a solid foundation you can build on later by adding things like telemedicine or a patient portal when you're ready.
How Can We Guarantee Our Patient Data Stays Secure?
Keeping patient data secure isn't about finding a single magic solution. It’s about building a multi-layered defence, especially with strict privacy laws like Canada's PHIPA. Think of it as a combination of smart technology and smart habits.
Choose the Right Partners: Only work with technology providers who live and breathe healthcare compliance. Their products should have security baked in from the very beginning, not bolted on as an afterthought.
Use a Secure Cloud: Opt for trusted cloud platforms that offer features like end-to-end data encryption. For Canadian clinics, ensuring your provider offers Canadian data residency is non-negotiable for meeting regulatory demands.
Lock Down Your Internal Processes: Implement strict access controls so staff members can only see the information they absolutely need to do their jobs. Regular security training is also a must; human error is still one of the biggest risks.
Is This All Too Expensive for a New Practice or Startup?
It absolutely doesn't have to be. The biggest mistake you can make is trying to build a massive, all-in-one system right out of the gate. A much smarter and more budget-friendly approach is to start small and grow.
The key is to develop a Minimum Viable Product (MVP) that solves your single most urgent problem. This agile approach keeps initial costs down, delivers value to your practice quickly, and provides real-world feedback to guide what you build next.
This way, you can learn as you go, reinvesting in new features and tools as your practice grows and your revenue streams become more established.
How Do We Actually Measure the ROI of All This?
Measuring the return on your investment in digital tools goes way beyond just dollars and cents. You need a balanced view that includes clinical, operational, and financial wins.
Before you implement anything, set your benchmarks. For example, clinical success could be measured by improved patient outcomes or a drop in hospital readmission rates. Operationally, you could track things like shorter patient wait times or how many fewer hours your staff spends on paperwork. On the financial side, ROI shows up as lower operating costs, quicker billing cycles, and the ability to serve more patients.
Ready to start your digital transformation with a partner who understands healthcare? Cleffex Digital Ltd specialises in creating secure, compliant, and scalable software that solves real-world challenges for practices like yours. Learn how we can help you build the future of your practice.







