Artificial intelligence isn’t here to replace doctors and nurses; it’s becoming their most powerful collaborator. Think of it as a tool that can sift through enormous mountains of data to help improve diagnoses, tailor treatments to individual patients, and even take over the tedious administrative work that bogs down a clinic. At its core, AI gives healthcare professionals the support they need to make quicker, more data-driven decisions, which ultimately leads to better care for patients.
How AI Is Reshaping Modern Healthcare
Picture a brilliant assistant who has read every medical journal ever published, can instantly recall a patient’s entire medical history, and can spot subtle patterns in an MRI scan that the human eye might miss. That’s the role AI is playing. It’s not about taking over; it’s about amplifying the skills and intuition of human experts.
The applications of AI in Healthcare Industry are already making a real-world difference across the entire patient journey. From the very first appointment where symptoms are discussed to crafting a long-term recovery plan, AI is becoming a vital part of the process. It helps cut down on human error, speeds up life-saving research, and lightens the massive operational load on hospitals and clinics.
Key Areas Where AI Is Making an Impact
While AI’s reach is broad, its influence is most profound in a few critical areas:
- Smarter Diagnostics: AI algorithms can analyze medical images—like X-rays, CT scans, and MRIs—with incredible accuracy. They often catch early signs of diseases like cancer or diabetic retinopathy long before they become obvious.
- Personalized Treatment Plans: By looking at a patient’s unique genetic code, lifestyle, and medical history, AI can help doctors move beyond one-size-fits-all treatments. This leads to personalized therapies that are far more effective.
- Streamlined Operations: AI is a game-changer for administrative tasks. It automates things like scheduling appointments, managing patient records, and handling billing, freeing up clinicians to spend more quality time with their patients.
This visual breakdown shows just how much value AI is adding across the board.
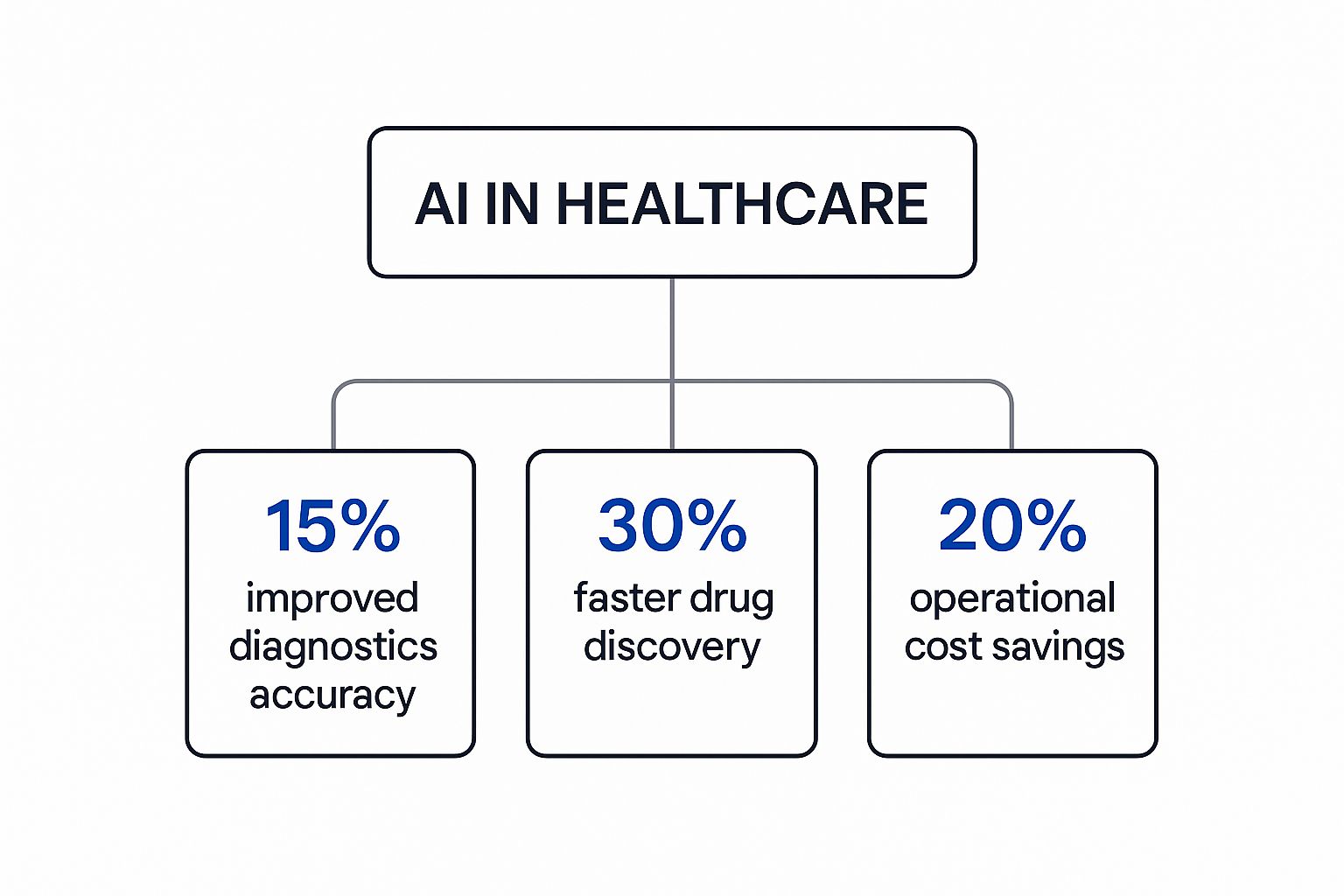
As you can see, the numbers point to huge improvements in diagnostic accuracy, operational speed, and overall cost savings. This is why healthcare systems everywhere are increasingly integrating AI into their workflows. For a more detailed look, the Artificial Intelligence for Healthcare: A Practical Medical Guide provides an excellent, in-depth exploration of these applications.
The key takeaway is that AI provides the data-backed insights that empower and elevate the judgment of medical professionals.
Key Ways AI Assists Healthcare Professionals
To give you a clearer picture, this table summarises the main domains where AI is actively helping medical professionals today.
| Healthcare Domain | How AI Helps | Primary Benefit |
|---|---|---|
| Diagnostics | Analyzes medical images (X-rays, MRIs) to detect anomalies. | Earlier and more accurate disease detection. |
| Treatment Planning | Assesses patient data to suggest personalized therapies. | More effective, customized care plans. |
| Drug Discovery | Simulates molecular interactions to speed up research. | Faster development of new medications. |
| Administrative Tasks | Automates scheduling, billing, and record-keeping. | Increased efficiency and more time for patient care. |
| Predictive Analytics | Identifies at-risk patients before a health crisis occurs. | Proactive and preventative healthcare. |
Ultimately, these tools work together to create a more efficient, accurate, and patient-centred healthcare system for everyone.
Speeding Up Diagnosis with Intelligent Systems

One of the most powerful and immediate ways AI is making its mark on healthcare is in medical diagnostics. Think of an AI model as a tireless assistant that’s had the chance to study more medical images than any human could in a dozen lifetimes. That’s the real power behind AI-driven diagnostic tools.
By training on vast libraries of X-rays, MRIs, and CT scans, these systems learn to spot subtle patterns and tiny anomalies that often signal the very first signs of disease. They can pick out microscopic cancerous cells, flag potential strokes in brain scans, or identify diabetic retinopathy from retinal photos with incredible speed and precision.
Making Medical Imaging More Accurate
For radiologists and pathologists, AI is essentially a second set of eyes—a highly vigilant one at that. It doesn’t replace their deep expertise; it supports it. Picture a radiologist carefully examining a chest X-ray for any hint of a tumour. An AI can scan that same image, pixel by pixel, in just seconds and highlight specific areas of concern that need a closer human look.
This partnership dramatically reduces the odds of human error, which can happen to even the best specialists, especially when they’re dealing with fatigue or overwhelming caseloads. The result is a more reliable and accurate diagnostic process. In fact, many studies show that AI algorithms can often spot abnormalities with an accuracy that matches or even surpasses human experts, making them an invaluable partner in the clinic.
This is especially critical when it comes to catching aggressive diseases early.
By finding trends and relations between health, environmental, and behavioural factors, AI models can aid the future of early detection, leading to interventions when treatments are most effective.
This moves diagnostics from simply reacting to symptoms to proactively predicting problems.
AI Diagnostics in the Real World
This isn’t just theory or something coming in the distant future—it’s already happening in clinics and hospitals today. Here are a few concrete examples of how AI is being used right now:
- Cancer Detection: AI tools are regularly used to analyze mammograms and CT scans for early signs of breast and lung cancer. There are documented cases where an AI has identified malignant cells that were missed during the initial human review.
- Ophthalmology: Companies have developed smartphone-based cameras that use AI to screen for diabetic retinopathy, a leading cause of blindness. This makes vital screening accessible and affordable, especially in remote or underserved communities.
- Pathology: In the lab, AI helps pathologists by automatically counting cells or identifying specific tumour features in tissue samples. This not only speeds up the workflow but also gives them solid, quantitative data to back up a diagnosis.
Making Faster Decisions When Time Is Critical
In an emergency like a stroke, every second is crucial. The faster the diagnosis, the sooner treatment can start, which can make all the difference for a patient’s recovery. AI algorithms are now able to analyze brain scans almost instantly, detecting signs of a blockage or bleed.
This rapid analysis gives medical teams the information they need to make critical decisions far more quickly than was possible with traditional methods. By shrinking the time from scan to diagnosis, AI is directly contributing to better patient outcomes in these high-stakes situations. It’s a perfect example of how intelligent systems are helping healthcare save lives by simply enabling us to work faster and smarter.
Personalizing Patient Treatment Plans With AI

AI isn’t just speeding up diagnoses. It’s charting each patient’s treatment journey, too.
Gone is the era of “one-size-fits-all” prescriptions. Today, AI plays the role of a digital detective, piecing together genetics, lifestyle habits and medical history into a single portrait.
It then cross-checks that tapestry of data against millions of past clinical trials and peer-reviewed studies. From there it teases out the most promising treatment path for every unique case.
Suddenly, treatment becomes a data-driven endeavour rather than a hopeful guess. Patients and doctors start with a clear, custom roadmap rather than trial and error.
Customizing Cancer Therapies
Oncology is where this level of detail really makes a difference. A tumour’s genetic signature can vary wildly, even between two patients with the same cancer type.
- AI algorithms analyse genomic profiles to forecast which chemotherapy drugs or targeted therapies will work best.
- Clinicians avoid slow trial-and-error cycles, sparing patients unnecessary side effects.
- Treatments can be re-evaluated in real time as the tumour evolves.
By mining deep genomic insights, AI helps predict how each treatment will perform against a specific tumour profile.
This sharper focus means every therapy plan fits as precisely as a custom suit.
Managing Chronic Conditions
Long-term illnesses like diabetes demand relentless balancing—diet, exercise and stress all swing blood sugar levels.
AI tools are stepping in to simplify daily care:
- Smart Glucose Monitors: They learn a patient’s blood sugar rhythms and forecast potential highs or lows before they occur.
- Automated Insulin Dosing: When paired with insulin pumps, they form a closed-loop system that adjusts doses in real time.
- Lifestyle Coaching: AI-driven tips on food choices and activity help keep levels stable without guesswork.
With this proactive support, patients experience fewer complications and gain more control over their lives. By fine-tuning every aspect of a treatment plan, AI ensures healthcare is not just more efficient, but genuinely patient-centred.
Making Hospitals Run Smoother with Smarter Admin

Beyond the patient’s bedside, AI is making a huge difference behind the scenes. It’s tackling the mountains of administrative work that can bog down hospitals, leading to inefficiencies and, frankly, burning out talented clinicians. Think of AI as an efficiency expert that never gets tired, handling the repetitive jobs that keep a hospital running day-to-day. This frees up doctors and nurses to do what they do best: care for people.
A huge chunk of this admin work is clinical documentation. Doctors and nurses can spend a staggering amount of time just typing up notes, filling out forms, and wrestling with electronic health records. This is where a technology called Natural Language Processing (NLP) steps in. In simple terms, NLP can act like a highly intelligent scribe, listening to a doctor’s conversation with a patient and turning it into a perfectly structured medical note.
This isn’t just a small convenience; it’s a game-changer. It slashes the time spent on manual data entry and helps fight clinician burnout. It’s no secret that EHR paperwork is a top reason doctors lose productive hours. Understanding what’s possible with AI for medical transcription shows just how much of this clerical weight can be lifted off clinical staff.
Fine-Tuning Patient Flow and Hospital Resources
AI’s knack for logistics is also being put to work managing the very pulse of a hospital. Getting patients scheduled, admitted, and into the right bed is a complex juggling act. AI systems can sift through historical patterns and real-time data to solve this puzzle with incredible accuracy.
Often, these solutions are part of custom healthcare software development projects, designed to help hospitals get the most out of every resource they have.
Here are a few ways AI is making a real-world impact:
- Smarter Scheduling: AI algorithms can predict when a patient is likely to be a no-show or cancel at the last minute. This lets staff proactively fill those spots, keeping the schedule full and waitlists moving.
- Predicting ER Wait Times: By looking at who’s coming in, who’s on shift, and what resources are free, AI can give a surprisingly accurate forecast of emergency room wait times. This helps manage patient expectations and lets the hospital shift staff where they’re needed most.
- Optimizing Bed Management: AI can keep a close eye on when patients are discharged, when rooms are cleaned, and who needs to be admitted next. This coordination ensures beds are turned over quickly, getting patients where they need to go without delay.
When you hand these complex logistical decisions over to AI, you don’t just get a more efficient hospital. You get a better patient experience—one with shorter waits and smoother, more organized care.
To see the difference clearly, let’s compare how things were done before with how AI helps now.
Traditional vs AI-Powered Administrative Tasks
This table illustrates the efficiency gains achieved by integrating AI into common healthcare administrative processes.
| Administrative Task | Traditional Method (Without AI) | AI-Powered Method | Key Improvement |
|---|---|---|---|
| Appointment Scheduling | Manual phone calls, staff-managed waitlists, high no-show rates. | AI predicts no-shows, automates reminders, and manages dynamic waitlists. | Reduced empty slots, lower administrative overhead. |
| Clinical Documentation | Physicians manually type notes into EHRs, often after patient hours. | NLP transcribes spoken conversations into structured EHR notes in real-time. | Saves hours of physician time daily, reduces burnout. |
| Bed Management | Manual coordination between departments via phone and whiteboards. | AI system tracks patient status and cleaning crews to optimize bed turnover. | Faster patient placement, increased hospital capacity. |
| Medical Billing & Coding | Human coders manually review charts to assign billing codes, prone to error. | AI analyzes clinical notes and suggests appropriate codes automatically. | Fewer claim denials, faster revenue cycle. |
As the table shows, the shift isn’t just about speed; it’s about making the entire system smarter and more responsive.
Taking the Headache Out of Medical Billing
Finally, AI is bringing some much-needed sense to the notoriously complex world of medical billing. New AI tools can scan a doctor’s notes and instantly suggest the correct billing codes. This job has always been done by hand, which means it’s slow and mistakes happen.
By automating this process, AI improves accuracy, which means fewer rejected insurance claims and faster payments for the hospital. By taking over these critical but tedious tasks, AI helps keep the institution financially healthy so it can focus its resources where they matter most—on patient care.
Navigating The Regulatory And Ethical Landscape
As AI tools weave deeper into healthcare, safety, privacy and accountability become non-negotiable. Patients need to know their data is protected and that clinical decisions rest on solid legal and ethical grounds.
A core principle here is the human-in-the-loop model. Think of AI as a knowledgeable consultant that:
- Offers data-driven suggestions
- Flags potential issues
Ultimately, a licensed healthcare professional reviews and signs off on every decision. This keeps human empathy and judgement at the centre of care.
Establishing Clear Guardrails For AI In Medicine
Regulators are drafting new laws to ensure AI amplifies, rather than overrides, medical expertise. The aim is simple: empower clinicians without replacing them.
California is leading by example. Recent legislation mandates physician supervision over AI outputs, safeguarding patient safety and professional autonomy. This hands-on approach shows that governance can keep pace with technological change.
This image outlines the key bills designed to enforce human oversight in AI-powered healthcare.
Ensuring Human Judgment Prevails
By 2025, California’s Assembly Bill 3030 requires any clinical communication generated by AI to be reviewed by a licensed provider before it reaches a patient. Likewise, Senate Bill 1120 protects physician autonomy in insurance reviews, preventing AI from making solo decisions that impact care. You can discover more about these legislative trends.
By prioritising accountability and mandating human oversight, these regulatory efforts ensure that as AI helps the healthcare industry evolve, it does so safely and ethically, always keeping the patient’s best interests at the forefront.
This layered framework reassures clinicians and patients alike. With clear legal and ethical standards, healthcare professionals can confidently adopt AI tools, knowing patient well-being remains the top priority.
Here is the rewritten section, designed to sound natural, human-written, and expert-led.
What’s Next for AI in Healthcare?
The relationship between AI and healthcare professionals is just getting started, and it’s poised to create some incredible breakthroughs. We’re moving beyond the applications we see today and stepping into genuinely new territory.
Think about drug discovery. AI is now being used to simulate how molecules interact, which can drastically cut down the time needed to develop new medicines. This is the kind of research that used to take decades, but AI can now pinpoint promising compounds in a fraction of that time. At the same time, predictive analytics are getting so sharp they can forecast disease outbreaks by sifting through public health data, giving officials a crucial head start.
A Partnership, Not a Replacement
It’s easy to get carried away and think AI is here to take over, but that’s not the reality. The goal has always been to augment the skills of clinicians, not replace them. This model—where human intuition is supercharged by machine precision—is quickly becoming the new standard of care. It’s all about helping doctors and nurses deliver better outcomes in an increasingly complex field.
This collaborative mindset is driving rapid adoption. By early 2025, an estimated 66% of doctors in the United States were already using some form of AI in their practices. States like California are leading the charge, but they’re also putting up important guardrails. Regulations there make it clear that AI is a tool, and it can’t replace human medical judgment. If you’re curious, you can discover more insights about California’s healthcare AI advisory to see how they’re handling this.
The real aim is to create a seamless partnership where technology does the heavy lifting with data, freeing up healthcare professionals to focus on what really matters: the patient.
This balanced approach isn’t just for clinicians; it extends to the tools we build for patients, too. For anyone building in this space, it’s vital to understand the key things to consider when developing a medical mobile app. When we successfully merge human expertise with AI’s analytical power, the future of healthcare starts to look a whole lot more efficient, personalised, and effective for everyone involved.
Your Questions About AI in Healthcare, Answered
As AI finds its way into more clinics and hospitals, it’s only natural to have questions. Getting to grips with what this technology can—and can’t—do is the best way to understand its real impact.
It’s crucial to remember that AI isn’t here to take over. The real goal is to give our healthcare professionals better tools. By letting AI crunch the complex data, we free up clinicians to do what they do best: care for patients.
Will AI Replace Doctors and Nurses?
Not a chance. Think of AI as an incredibly smart assistant, not a replacement. Its job is to spot patterns in data and handle repetitive tasks, which gives doctors and nurses more time for what really matters.
AI can’t replicate the empathy, complex judgment, and human touch that are so fundamental to patient care. The future isn’t about machines making decisions; it’s about a partnership where technology handles the heavy data lifting, allowing professionals to focus on patient connection and compassionate care.
How Is My Health Data Kept Safe?
Protecting patient data is non-negotiable. Any AI system used in a medical setting has to follow strict privacy laws like PIPEDA here in Canada. Before data is ever used to train an AI model, it’s anonymised and encrypted to strip out personal details.
On top of that, new regulations are always emerging to keep AI use transparent and hold providers accountable. The whole industry is focused on using data to improve health outcomes while maintaining the highest standards of privacy.
An AI-suggested diagnosis should be seen as a highly informed second opinion. Current best practices require a ‘human-in-the-loop’ system, where a qualified physician must always review, verify, and interpret AI findings in the context of the patient’s full health profile.
Can I Trust a Diagnosis Suggested by an AI?
You can trust it as a powerful piece of the puzzle, but the final diagnosis always comes from a human expert. An AI might flag a tiny anomaly on a scan with incredible accuracy, but it’s the doctor’s job to put that finding into context with your overall health.
Essentially, the AI brings speed and precision to the table, but the final medical decision rests with a qualified professional who knows your complete history. This human oversight is what makes the diagnostic process both safe and reliable.







