Before you write a single line of code for your healthcare data management software, you need a rock-solid strategic foundation. This isn't just about brainstorming features; it's about deeply understanding the real-world clinical problems you're trying to solve. This discovery phase is, without a doubt, the single most critical factor in whether your product gets adopted by clinicians or left to gather dust.
Building Your Strategic Foundation in Healthtech
Truly great software solves a genuine need. In healthcare, these needs are often tangled up in complex clinical workflows, heavy administrative tasks, and frustrating data silos. Simply listing out features without understanding this context is a surefire way to fail. The real goal is to dig deep and find the core pain points your software can eliminate.
To do this, you have to get out of the boardroom and into the hospital corridors. The most valuable insights don't come from assumptions; they come from real conversations with the nurses, doctors, lab techs, and administrators who will be using your system every single day.
Uncovering Critical User Pain Points
To build software that people actually want to use, you need to become an expert in their daily frustrations. This means conducting detailed interviews and even shadowing them to map out how they currently get things done.
Your investigation should zero in on a few key areas:
Workflow Bottlenecks: Where do things slow down? Are clinicians relying on sticky notes, spreadsheets, or other manual workarounds to connect the dots between different systems?
Data Gaps: What crucial information is a struggle to access when it's needed most? How much of their valuable time is eaten up hunting for patient histories, lab results, or billing information?
User Frustrations: What specific parts of their current software drive them crazy or, worse, lead to errors?
The "Magic Wand" Question: If they could fix just one thing to make their job easier and improve patient care, what would it be?
The goal here isn't just to collect feedback; it's to build empathy. Understanding the stress a clinician feels when a system lags during a patient emergency will guide your development far better than a simple feature request ever could.
Defining Your Unique Value Proposition
Once you have a firm grasp of the problems, it's time to look at the market. Your software won't exist in a vacuum. A thorough competitive analysis will show you what other tools are doing right, where they're missing the mark, and how you can carve out a unique space for your product.
Look at both direct competitors and any adjacent tools they might be using. Are they built for massive hospital networks or small, independent practices? Is their main selling point powerful analytics, seamless interoperability, or an intuitive user interface? This analysis helps you find the gaps in the market, allowing you to position your software as the perfect solution for a specific, underserved need.
This groundwork is absolutely essential for creating a product that truly connects with its users and secures a sustainable place in the market. The healthcare enterprise software market is growing fast, with forecasts showing a Compound Annual Growth Rate of about 13.8% through 2034. In North America alone, the market is set to expand from roughly USD 43.62 billion to an incredible USD 158.63 billion by 2034, all fuelled by the demand for smarter data management. Your unique value proposition is your ticket to capturing a piece of that growth.
All this initial research comes together to form a clear, documented vision for the project. This vision acts as your North Star throughout the entire development process, ensuring every design decision and technical choice aligns with the core purpose of solving the problems you identified from day one. To help structure this vision, you might find our guide on building a technology roadmap template useful.
Designing a Future-Proof Software Architecture
Think of your software's architecture as its DNA. It determines everything, from how quickly you can add features to how it defends against threats and handles a growing user base. Nailing this blueprint from the start is absolutely critical for creating a solution that can adapt to the constantly shifting demands of healthcare.
One of the first big decisions you'll face is choosing the right architectural pattern. For most, the choice boils down to two main paths: monolithic or microservices. Each has its own set of pros and cons, especially in a healthcare context.
The groundwork for this decision is laid during the initial discovery phase, where you talk to users, understand their real-world needs, and clearly define what you're building.
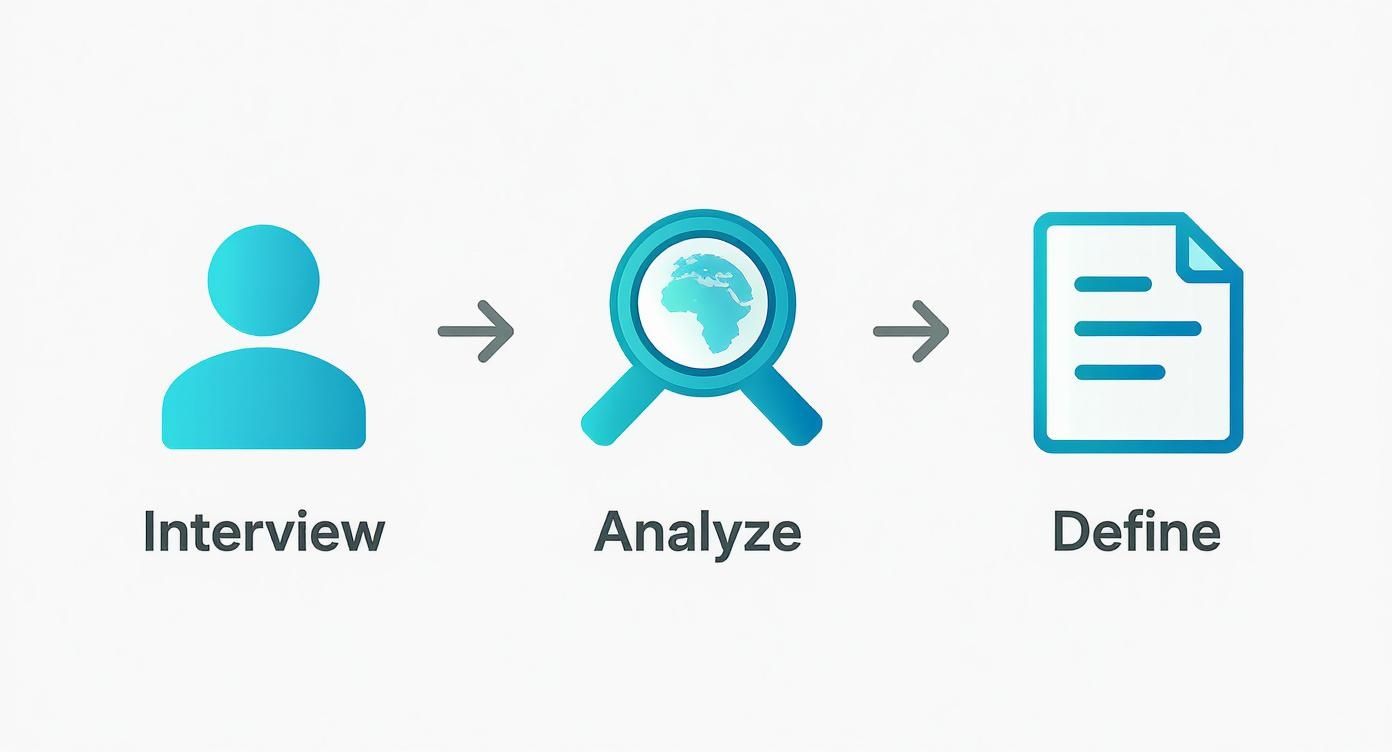
As you can see, insights from real-world stakeholder interviews directly shape the analysis and definition of the project, which is what allows you to make an informed architectural choice.
Monolithic vs. Microservices Architectures
A monolithic architecture is the traditional approach: the entire application is built as a single, tightly-knit unit. Everything from the user interface to the deep business logic and data layers is bundled together. If you're a startup aiming to get a Minimum Viable Product (MVP) out the door, this can be a smart move. Development is often quicker upfront, and deploying a single unit is far less complex.
The problems start to creep in as the system gets bigger. A tiny bug in one module can crash the entire application. Want to update a piece of your technology? You're looking at a massive, risky overhaul. Scaling specific functions, like a resource-heavy analytics engine, is also a huge pain because you have to scale the entire application along with it.
On the other hand, a microservices architecture chops the application into a collection of small, independent services. Each service is built around a specific business capability; think patient registration, billing, or appointment scheduling. These services then talk to each other through well-defined APIs.
This approach gives you incredible flexibility. Teams can build, deploy, and scale their services on their own timelines. If the e-prescribing service suddenly gets hammered with traffic, you can beef up its resources without touching anything else. This modularity also makes the system more resilient; if one service goes down, the rest of the application can often keep running.
For complex healthcare data management software, a microservices approach is almost always the better long-term bet. It keeps you agile and makes it far easier to integrate with new systems or adopt new technologies without having to tear everything down and start over.
To help you visualise the differences, here's a quick comparison of the two architectural patterns.
Comparing Architectural Patterns for Healthcare Software
This table compares the key characteristics of Monolithic and Microservices architectures to help you decide which is best for your healthcare software development project.
| Characteristic | Monolithic Architecture | Microservices Architecture |
|---|---|---|
| Development Complexity | Simpler to start, as it's a single codebase. | More complex initially due to the distributed nature. |
| Deployment | Straightforward; deploy the entire application at once. | Complex; requires coordinating multiple service deployments. |
| Scalability | All or nothing; the entire application must be scaled. | Granular; individual services can be scaled independently. |
| Technology Stack | Limited to a single, unified technology stack. | Polyglot; each service can use the best tech for its job. |
| Resilience | Low; a failure in one component can crash the system. | High; failure in one service is isolated and less likely to impact others. |
| Team Structure | Best for small, single teams. | Ideal for multiple, independent teams working in parallel. |
Ultimately, the choice depends on your project's scale, team size, and long-term vision.
Selecting the Right Technology Stack
Your architecture choice heavily influences your technology stack. There’s no magic bullet here; the "best" stack is the one that fits your team's skills, your project's specific needs, and your roadmap for the future.
Here's what you need to weigh:
Talent Availability: How easily can you hire developers? Sticking with a popular stack like Java with Spring Boot or Node.js with React can make recruiting a whole lot easier.
Development Speed: Frameworks like Ruby on Rails or Python with Django are fantastic for rapid development, which is a huge plus when you're trying to launch an MVP.
Scalability and Performance: For heavy-duty data processing, you might look at languages like Go or Kotlin, which are known for their raw performance and efficiency.
Long-Term Maintenance: Think about the ecosystem. A language or framework with strong community support will give you access to more libraries, tutorials, and critical security updates down the road.
You can get a deeper understanding of these options by exploring different enterprise application architecture patterns to see how they map to specific business challenges.
Implementing Essential Data Standards
In healthcare, no software is an island. Your platform must be able to talk to the vast web of existing systems, especially Electronic Health Records (EHRs). This makes interoperability standards completely non-negotiable.
Health Level Seven (HL7) is the old guard, but it's still the standard that powers much of the data exchange between hospitals, labs, and clinics today. You'll definitely encounter it.
Fast Healthcare Interoperability Resources (FHIR), however, is the future. It's a modern standard that uses common web technologies like RESTful APIs and JSON, making data exchange far simpler and more efficient. Building your architecture with FHIR at its core is one of the smartest things you can do to future-proof your software. It’s your ticket to seamlessly connecting with modern EHRs and new mobile health apps, which is key to delivering a truly connected care experience.
Embedding Security and Regulatory Compliance by Design
When you're building software for healthcare, security isn't just another feature on the roadmap. You can't just bolt it on at the end. It has to be baked into the very core of your application, right from the first line of code. The consequences of getting this wrong are severe; a single breach can shatter patient trust, ruin reputations, and lead to crippling legal penalties.
This philosophy is often called "security by design." It's a proactive mindset. Instead of waiting for problems to appear, you anticipate threats and build your defences into every single layer of the software. It fundamentally changes security from a final checkbox item into an ongoing, integral part of the development lifecycle.

The first step is always to get a firm grip on the regulatory frameworks that dictate how patient data must be handled. While the specific rules change from one country to another, they all share the same core principles: privacy, security, and patient consent.
Navigating Key Regulatory Mandates
Different jurisdictions have their own laws, but they all circle back to protecting patient privacy. For any healthcare data system to be truly robust and compliant, understanding data consistency principles is also absolutely critical to guarantee the information is both reliable and accurate.
Here are the heavy hitters you’ll almost certainly encounter:
PIPEDA (Canada): The Personal Information Protection and Electronic Documents Act is Canada's federal privacy law. It mandates that organisations get clear consent before collecting or using personal information and requires strong security safeguards. Don't take it lightly; fines can hit $100,000 CAD for each violation.
HIPAA (United States): The Health Insurance Portability and Accountability Act is the gold standard in the U.S. for protecting sensitive patient health information (PHI). It lays down strict rules about who can access data and has stringent breach notification requirements.
GDPR (European Union): The General Data Protection Regulation is arguably one of the toughest privacy laws on the planet. It demands explicit patient consent and enshrines rights like the "right to be forgotten." The penalties are massive, reaching up to €20 million or 4% of a company's global annual turnover.
While the legalese can feel overwhelming, these regulations boil down to one simple idea: treat patient data with the utmost respect and care. Your starting assumption should be that every single piece of data is sensitive and needs to be protected at all costs.
Implementing Core Security Measures
Turning those legal requirements into actual code and infrastructure involves a multi-layered strategy. There's no single magic tool; it's about combining multiple practices to create a truly secure environment.
Robust Access Controls
Think about it: not everyone in a clinic needs to see a patient's entire chart. This is where Role-Based Access Control (RBAC) becomes non-negotiable. You need to create specific user roles, like 'nurse,' 'doctor,' or 'billing specialist', and grant permissions based strictly on what's needed for their job.
A billing specialist, for instance, should see insurance details but have absolutely no access to clinical notes. This is the "principle of least privilege," and it dramatically shrinks your attack surface and the risk of accidental data exposure.
End-to-End Data Encryption
Data is vulnerable at every stage, whether it's moving across a network or sitting on a server. You have to protect it everywhere.
Encryption in Transit: Any data moving between a user's device and your servers must be encrypted using protocols like TLS (Transport Layer Security). This prevents eavesdroppers from pulling sensitive information out of the data stream in what's known as a "man-in-the-middle" attack.
Encryption at Rest: When data is stored in your database or on a hard drive, it also needs to be encrypted. This is your last line of defence. If someone physically steals a server, the encrypted data is just unreadable gibberish without the decryption keys.
Fostering a Culture of Proactive Security
Security is a moving target; it's never "done." It requires constant vigilance and a team-wide commitment to finding and fixing vulnerabilities before they can be exploited.
Regular Security Audits and Penetration Testing
You can't fix a problem you don't know you have. That's why scheduling regular, independent security audits is so important. These audits involve experts poring over your code, architecture, and policies to find any weak spots.
Penetration testing (or "pen testing") takes things a step further. You essentially hire ethical hackers to do their worst – to actively try and break into your system. These simulated attacks give you priceless, real-world insight into how an actual attacker thinks and operates, shining a bright light on the vulnerabilities you need to patch immediately. This isn't a one-time thing; it needs to happen periodically, especially after any major software update or architectural change.
Choosing Your Deployment and Analytics Strategy
You’ve got the architecture sorted out, but two massive decisions remain: where will your software live, and how will it think? The choice between on-premise servers and the cloud isn’t just a technical footnote; it fundamentally defines your software's cost structure, its ability to scale, and who can access it. This decision is directly tied to your ability to build in the powerful analytics needed to turn raw data into life-saving insights.
Your deployment model is the foundation for everything else. It dictates how you handle hardware, security, and updates, so it's a strategic call you need to get right from the start.

Weighing On-Premise vs. Cloud Deployment
Going with an on-premise deployment means you’re hosting everything on your own servers, inside your own physical data centre. This approach gives you the absolute maximum control over your data and infrastructure. For a large hospital network with an established IT department and strict data sovereignty rules, this can seem like the safest bet.
But that control comes with a hefty price tag. You're on the hook for everything – buying and maintaining expensive hardware, managing constant security patches, and figuring out disaster recovery. Need to scale up? That means a huge capital investment and a long, painful procurement process. It’s not exactly agile.
On the other hand, a cloud-based deployment using a provider like Amazon Web Services (AWS), Google Cloud Platform (GCP), or Microsoft Azure passes that entire infrastructure headache to someone else. This gives you incredible flexibility. You can spin up new resources almost instantly and, crucially, only pay for what you actually use.
For most modern healthcare applications I've worked on, the cloud is the clear winner. The ability to elastically scale services to meet fluctuating demand, combined with the robust, pre-certified compliance features these providers offer, makes it a more practical and often more secure choice than trying to manage everything in-house.
Let’s be honest, the major cloud platforms invest billions in security. They also offer specific, healthcare-focused services that already meet regulations like PIPEDA and HIPAA. This takes a huge compliance burden off your team's shoulders.
Unlocking Actionable Insights with Analytics and AI
In healthcare, just storing data isn't enough anymore. The real magic happens when you use that data to predict trends, improve patient outcomes, and make operations more efficient. This is where a smart analytics strategy, often powered by artificial intelligence (AI), becomes a game-changer.
When you bake analytics capabilities into your software, it stops being a digital filing cabinet and becomes a dynamic tool. Suddenly, you can:
Build predictive models: Flag patients at high risk for conditions like sepsis or hospital readmission, giving clinical teams a chance to intervene early.
Manage population health: Analyse community-wide health data to spot disease outbreaks before they spiral, track vaccination rates, or manage chronic diseases more effectively across a region.
Boost operational efficiency: Optimise hospital bed allocation, forecast staffing needs for busy shifts, and find bottlenecks in the revenue cycle.
The demand for this is exploding. The healthcare analytics market was valued at USD 2,776.6 million and is on track to hit USD 11,639 million by 2033. This massive growth tells you one thing: analytics are no longer a "nice-to-have." They are critical.
Building Your Analytics Engine
You’ve got a couple of options here. You can build custom analytics modules from scratch or integrate with specialised third-party platforms. Whichever route you take, the end goal is the same: create a system that can chew through massive datasets securely and present the findings in a clear, actionable way for clinicians and administrators.
Think about a real-world scenario. A hospital wants to slash wait times in its emergency department. An integrated analytics module could analyse years of admission data to find patterns, linking wait times to the time of day, day of the week, and even the types of symptoms people arrive with. The system could then predict peak hours and suggest better staffing levels, directly improving patient care. Our team has deep experience building these kinds of powerful healthcare data analytics solutions that turn raw information into tangible results.
Getting Integration and Quality Assurance Right
This is where the rubber meets the road. All the planning and coding in the world don't mean much until your software proves it can handle the pressure of a real clinical setting. This final stretch: testing and integration is all about making sure your system isn't just functional, but genuinely reliable and intuitive for the healthcare professionals who will depend on it every day.
If you cut corners here, you're setting yourself up for failure. A buggy system or one that doesn't play well with existing tools can cause serious workflow headaches, frustrate users, and completely erode trust from day one. In healthcare, that's a risk you just can't take.
A QA Strategy Grounded in Clinical Reality
Quality assurance in healthcare software is more than just squashing bugs. It's about stress-testing your system against the chaos of a busy hospital or clinic. Your QA plan has to be built around real-world scenarios to ensure your software actually helps, not hinders, patient care.
It's not enough to see if a button works. You have to validate the entire clinical workflow it supports. Does it make sense? Is it efficient? Most importantly, is it safe? That means layering different types of testing to catch problems from every angle.
Here’s how we typically break it down:
Unit Testing: This is the foundational level where developers check their own code, making sure each tiny component works perfectly on its own.
Integration Testing: Now we start connecting the pieces. Does the patient registration module talk to the billing service correctly? This is where you find out.
End-to-End (E2E) Testing: Think of this as a full dress rehearsal. We simulate an entire patient journey, from scheduling an appointment and documenting the visit to sending the final bill, to make sure the whole system hangs together seamlessly.
User Acceptance Testing (UAT): This is the moment of truth. We put the software in the hands of actual clinicians: doctors, nurses, admin staff, and ask them to do their jobs with it. Their feedback is pure gold for spotting usability flaws that no automated test could ever find.
A piece of hard-won advice: Get your clinical users involved in writing the UAT scripts. A developer might think a three-click process to pull up lab results is fine, but a nurse in the middle of an emergency knows it's two clicks too many. Only your end-users can give you that kind of critical insight.
The EHR Integration Gauntlet
Integrating with a facility's existing Electronic Health Record (EHR) system is often the single biggest technical challenge you'll face. The EHR is the heart of a modern clinic or hospital; if your software can't communicate with it, it's practically useless.
Don't expect this to be a simple plug-and-play exercise. Connecting to major platforms like Epic, Cerner, or Allscripts is a complex dance. You'll need to navigate their developer programs, get familiar with their specific APIs, and often go through a rigorous certification process.
On the technical side, this usually means working with interoperability standards like FHIR or the older HL7 to get data flowing between systems. It’s a painstaking process of mapping data fields, handling different formats, and building rock-solid error handling to deal with inevitable connection hiccups.
Rolling It Out: A Smooth Deployment and Beyond
Once testing is complete and the integrations are solid, it's go-time. But a "big bang" launch where everyone flips the switch at once is a recipe for disaster in a healthcare environment. The stakes are too high. A phased rollout is always the smarter, safer path.
Here are a couple of proven strategies:
Run a Pilot Program: Start with a single, controlled group, maybe one forward-thinking department or a smaller clinic. This gives you a final real-world shakedown, letting you iron out any last-minute kinks with a limited number of users before the full launch.
Roll Out by Feature: Instead of unleashing the entire platform at once, introduce new modules incrementally. This gives users time to adapt and massively reduces the initial training burden.
And remember, the work isn't over once you go live. Solid post-launch support is non-negotiable. Having a dedicated team on standby to answer questions, troubleshoot issues, and push out quick fixes is absolutely essential for building user confidence and driving long-term adoption.
Common Questions We Hear About Healthcare Software Development
When you're diving into a healthtech project, a lot of questions pop up right away. It's a unique field – you're dealing with incredibly sensitive data, navigating a maze of regulations, and trying to build something that clinicians will actually use. It’s a tough nut to crack, but incredibly rewarding when you get it right. Let's tackle some of the most common questions we get asked.
What’s the Single Biggest Hurdle to Overcome?
Hands down, the biggest challenge is security and compliance. We're talking about an unwavering commitment to regulations like PIPEDA, HIPAA, and GDPR. In most industries, a data breach is a major headache. In healthcare, it can ruin lives and expose an organisation to crippling legal and financial blowback.
You simply can't treat security as a feature you add on later. It has to be baked in from day one; what we call a "security-by-design" approach. Things like end-to-end encryption and granular, role-based access aren't just nice-to-haves; they are foundational pillars that need to be part of the initial architecture conversations.
How Long Will This Actually Take to Build?
The timeline for developing custom healthcare software is all over the map because it completely depends on what you're trying to build.
If you’re aiming for a Minimum Viable Product (MVP) that solves one or two specific problems really well, you could be looking at a launch in 6 to 9 months.
But if your vision is a sprawling, enterprise-level platform with multiple EHR integrations, sophisticated analytics, and complex clinical workflows, you should budget for 18 to 24 months, and sometimes even longer. This is where an agile development process becomes non-negotiable. It allows you to build, get feedback from real clinicians, and adjust your course in short cycles, which is critical to making sure the end product actually works in a busy hospital or clinic.
If there's one piece of advice I can give, it's to phase your project. Launch a focused MVP to get value into the hands of users quickly. From there, you can build out more features based on what people are actually doing with the software, not just what you think they need.
Why Does Everyone Keep Talking About Interoperability?
Interoperability is the glue that holds modern healthcare together. Think about it: a single patient's data might be scattered across a dozen different systems that don't speak to each other: the hospital's EHR, a specialist's private system, a lab's LIMS, the pharmacy's database, the billing platform… it's a mess.
This is where standards like HL7 and the newer, more flexible FHIR (Fast Healthcare Interoperability Resources) come in. They create a shared language so these separate systems can securely exchange critical information. Without that common ground, you can't build a single, unified view of a patient's journey, which severely limits how useful your software can be. Lack of interoperability is a deal-breaker for adoption.
What Kind of Team Do I Need to Pull This Off?
Building great healthcare software isn't just a job for coders. You need a specialised crew that brings together technical chops with a real understanding of how healthcare works.
A solid team will almost always include:
A Project Manager who keeps the train on the tracks.
A Business Analyst who lives and breathes healthcare and can translate a doctor's needs into technical specs.
UX/UI Designers who get that clinicians are working under immense pressure and need interfaces that are simple and foolproof.
Backend and Frontend Developers to build the actual application.
QA Engineers who are relentless in hunting down bugs and ensuring the software is intuitive.
A DevOps Engineer to handle the infrastructure and deployment pipeline.
A Compliance or Security Specialist whose entire job is to make sure every line of code and every process meets strict regulatory standards.
At Cleffex Digital Ltd, we build these expert teams, combining top-tier technical talent with deep healthcare industry experience to create software that is secure, compliant, and genuinely useful. Explore our custom development services to see how we can help bring your vision to life.







