Canada's healthcare system is undergoing a massive overhaul, finally transitioning from its paper-based roots to a more connected, digital future. This digital healthcare transformation in Canada is much more than just adopting new gadgets; it's about rebuilding the very foundation of how we deliver care to be more efficient, accessible, and focused on the patient. Think of it as swapping out an old, creased paper map for a live, province-wide GPS that reroutes care in real-time.
The Next Chapter for Canadian Healthcare

For years, Canadians have taken pride in their healthcare model, but let's be honest, it has been creaking under the weight of administrative overload and siloed information. The move to a digital-first mindset is a direct response to these long-standing frustrations, sparked by a perfect storm of evolving patient expectations and the urgent need for a smarter system.
Today’s patients simply expect more. They're used to managing their banking, shopping, and travel online, and they want that same level of convenience from their healthcare. This means easy access to their own health records, online appointment booking, and the choice of virtual visits. This consumer-driven demand is a powerful force pushing the entire industry forward.
Key Drivers Accelerating the Shift
At the same time, there's a serious national conversation happening about boosting efficiency and achieving better health outcomes for everyone. The current system, which still leans heavily on fax machines and manila folders, creates frustrating information gaps that get in the way of seamless, coordinated care. Digital tools are finally giving us a way to tear down those walls.
The table below breaks down the key factors pushing Canada’s digital health adoption into high gear.
Key Drivers of Canada's Digital Health Boom
| Driving Factor | Impact on the Healthcare System |
|---|---|
| Rising Patient Expectations | People want control over their health journey, demanding seamless access to records and virtual care. |
| Need for System Efficiency | Automation and digital workflows reduce administrative burdens, freeing up clinicians to focus on patients. |
| Improved Health Outcomes | Connected data enables better care coordination, proactive health management, and smarter clinical decisions. |
| Economic Momentum | Major investment in health-tech is fostering a dynamic ecosystem of innovation and new solutions. |
These drivers aren't just theoretical; they represent a fundamental change in how healthcare is valued and delivered.
The numbers back this up. In 2023, Canada’s digital health market was already valued at USD 19.5 billion, and it's on track to hit an incredible USD 53.92 billion by 2030. This kind of growth is a direct result of widespread smartphone use, reliable internet access, and the mounting pressure to get healthcare spending under control.
Understanding the Foundational Tools
At the centre of this change are a few core technologies that are becoming the new building blocks of patient care. Things like Electronic Health Records (EHRs) and telehealth aren't just buzzwords; they are the practical tools making this whole shift possible.
An EHR is best understood as a patient's single, secure digital chart – a living document that can be shared instantly and securely among their entire care team, from the family doctor to a hospital specialist.
This simple idea of a shared digital file is a game-changer, replacing stacks of scattered paper with one reliable source of information. In the same way, telehealth is essentially the modern-day house call, bringing expert medical advice to remote communities and fitting conveniently into the busy schedules of city dwellers. As these tools become standard, we're seeing how artificial intelligence in Canadian healthcare can build on them to find new ways to analyse data and support clinicians.
By getting a handle on why this digital shift is happening now, we can better prepare for the opportunities and challenges on the horizon. To see how these trends fit into the bigger picture, a guide to digital transformation in the healthcare industry offers a broader look at how technology is reshaping patient care globally.
Core Technologies Modernising Patient Care

To really understand the digital healthcare transformation in Canada, we need to peek under the hood and see what’s actually driving the change. These aren't just futuristic ideas; they are real tools being put to work today, tackling long-standing problems in how we manage data, communicate, and care for patients.
Think of these technologies as a team of specialists. Each one has a distinct job, but they all work together toward one goal: a more connected and intelligent healthcare system. From creating a single, reliable source for a patient's medical history to delivering expert care across vast distances, these tools are building the digital backbone of modern Canadian healthcare.
Electronic Health Records: The Digital Foundation
The heart of it all is the Electronic Health Record (EHR). An EHR is so much more than a digital filing cabinet. It’s a living, breathing story of a patient's health, accessible in real-time to everyone on their authorised care team.
Picture a patient from rural Saskatchewan needing to see a specialist in Saskatoon. In the old days, this would kick off a mad dash for paper files, faxed documents, and a very real risk of missing crucial information. With a solid EHR system, that specialist can securely pull up the patient's complete history: notes from their family doctor, recent blood work, allergies, all with just a few clicks.
This instant access to a single, unified record demolishes the information silos that have historically made healthcare delivery so fragmented. It means clinical decisions are based on the full picture, which is a massive leap forward for patient safety and coordinated care.
The core idea behind EHRs is simple but powerful: "one patient, one record." This principle cuts down on redundant tests, prevents medical errors, and gives every clinician the context they need to provide the best care possible.
Telehealth: Expanding Access to Care
If EHRs give the system its memory, telehealth gives it reach. Using everyday communication technology, telehealth delivers healthcare remotely, effectively shrinking the massive distances that are a reality for so many Canadians. It’s the modern-day house call, brought to you by secure video, phone, and patient portals.
The impact is felt everywhere:
Rural and Remote Communities: Patients can connect with specialists hundreds of kilometres away without the burden of travel time and costs.
Urban Convenience: A professional in a big city can have a follow-up appointment on their lunch break, making it easier to stick with their care plan.
Chronic Disease Management: Individuals with ongoing conditions can have regular check-ins from home, allowing for proactive, continuous care.
Telehealth isn't meant to replace in-person visits entirely, but to complement them. It ensures that where you live or your ability to travel no longer dictates your access to high-quality medical advice. It’s a fundamental shift toward a more accessible, patient-first model of care.
Artificial Intelligence and Machine Learning
Think of Artificial Intelligence (AI) and Machine Learning (ML) as expert assistants for clinicians. These systems can sift through enormous volumes of health data, spotting patterns that would be nearly impossible for the human eye to catch. The goal isn't to replace doctors but to amplify their expertise, leading to faster and more precise decisions. You can get a deeper look into how organisations are using AI-powered healthcare solutions to achieve real-world results.
Across Canada, AI is already making a tangible difference:
Medical Imaging: AI algorithms can analyse MRIs and CT scans with incredible accuracy, flagging potential issues for a radiologist to review.
Predictive Analytics: By analysing patient data, ML models can identify who is at a higher risk for things like sepsis or hospital readmission, giving care teams a chance to intervene early.
Reducing Admin Work: AI-powered scribes are now being used by thousands of Canadian primary care doctors to automatically turn patient conversations into clinical notes, fighting the burnout that comes from endless paperwork.
The Internet of Medical Things
Finally, the Internet of Medical Things (IoMT) is a growing web of connected devices that monitor patients’ health outside of a clinic or hospital. We’re not just talking about fitness trackers; these are clinical-grade tools that send a continuous stream of valuable health data back to the care team.
Consider smart glucose monitors for people with diabetes, wearable ECGs for cardiac patients, or smart inhalers that track usage for those with asthma. This information flows right into the patient's EHR, giving doctors a real-world look at their health between appointments. The IoMT is what helps shift care from being reactive to proactive, letting providers catch a worrying trend before it becomes a crisis.
Getting to Grips with Canadian Policy and Regulations
Jumping into Canada’s digital health scene isn’t just about having the latest tech. It’s about knowing the rules of the road. The country's regulatory landscape is designed with one core purpose: to protect incredibly sensitive personal health information. For any clinic, hospital, or tech company in this space, getting this right is the absolute foundation of patient trust.
Canada’s system is a mix of federal and provincial laws. Nationally, you have the Personal Information Protection and Electronic Documents Act (PIPEDA). This law sets the ground rules for how private organisations handle personal information in their business dealings. It's built on core ideas like consent, accountability, and keeping data secure.
But because healthcare is managed province by province, things get a bit more specific from there.
Diving into Provincial Privacy Laws
Most provinces have their own health-specific privacy laws. These are often considered "substantially similar" to PIPEDA, but they go deeper. In Ontario, for example, the big one is the Personal Health Information Protection Act (PHIPA). This is the rulebook for how "health information custodians" – think doctors, hospitals, and labs – must handle personal health data.
Knowing the specific act for your province isn't optional; it's essential. These laws spell out everything from how you get patient consent to what you must do if there’s a data breach. If you're curious about how this plays out with new tech, you can dig into the complexities of AI in healthcare data privacy in Canada to see how these regulations are being applied today.
Why Data Sovereignty is a Big Deal
A huge piece of this puzzle is data sovereignty. At its heart, this is a simple but powerful idea: the personal health information of Canadians should be stored and handled on servers physically located within Canada. This isn't just a technical preference; it's often a legal requirement to keep Canadian data under the protection of Canadian law.
For anyone choosing a tech partner, this is a make-or-break question. One of the first things you have to ask a cloud provider or software vendor is, "Where are your servers?" Partnering with a company that stores data outside of Canada could put you in serious violation of privacy laws.
This requirement acts as a shield, protecting patient information from foreign laws and access requests, which is crucial for maintaining trust in the system.
The Push for Interoperability and Shared Standards
Beyond privacy, the other major regulatory focus is interoperability. It sounds complex, but it's really about getting different digital health systems to speak the same language. Think about the banking system: you can use a Scotiabank card at a BMO machine because they all follow a shared standard. That's what we're aiming for in healthcare.
Canada is actively working to establish these kinds of standards for health information. The goal is to tear down the digital walls that stop a family doctor from seeing a patient's recent emergency room results. Organisations like Canada Health Infoway are at the forefront, working with governments to champion these common frameworks.
For any new technology, fitting into these standards is becoming non-negotiable. It’s what allows a new tool to become part of a larger, connected ecosystem instead of just another silo of isolated patient data.
Real-World Impact and Success Stories
The push for digital health in Canada isn't just about theory anymore; we're seeing real, measurable results on the ground. Across the country, what were once small pilot projects are now becoming standard practice, delivering clear wins for both patients and the healthcare system. These aren't just abstract ideas; they're concrete improvements that are changing lives and making healthcare delivery more efficient.
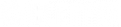
Looking at specific success stories shows us exactly how valuable these technologies are. The true impact is found in faster healing, fewer hospital visits, and a better quality of life for patients. These examples aren't just feel-good stories; they highlight the powerful return on investment when digital tools are integrated thoughtfully into how we provide care.
Accelerating Healing with Digital Wound Care
One of the most striking examples is in highly specialised care, like wound management. Traditionally, tracking a wound's healing process was a pretty subjective task, relying on manual measurements and handwritten notes. This often led to inconsistent assessments and, worse, delayed changes in treatment.
Now, digital wound care platforms are flipping that script. Clinicians can use something as simple as a smartphone camera, paired with advanced imaging software, to capture precise, 3D measurements of a wound. This creates a consistent and objective record, allowing the care team to track progress with incredible accuracy over time. Best of all, that data is instantly shared with everyone on the team, whether they’re in a hospital or out in the community.
This isn't just about better record-keeping. It's about better outcomes. When clinicians have accurate, real-time data at their fingertips, they can make smarter, faster decisions about treatment plans, which can lead to significantly quicker recovery times for patients.
By providing a clear, data-driven view of a wound's progress, digital tools empower clinicians to intervene earlier and more effectively, turning a subjective art into a precise science. This shift is a perfect example of how technology supports, rather than replaces, clinical expertise.
Slashing Readmissions with Digital Care Pathways
Another area seeing huge gains is in how we guide patients through surgery, both before and after. Digital care pathways are essentially interactive roadmaps that support patients through every single step. They send timely reminders, deliver educational content, and provide a direct line to the care team, all through a simple app.
The results have been nothing short of remarkable. These pathways help make sure patients show up properly prepared for their procedure and can recover safely at home afterwards. This dramatically reduces the chances of complications that might otherwise land them back in the hospital. It’s a win for the patient, who gets a smoother experience, and a win for the system, which sees less strain on overburdened emergency departments.
The public appetite for this is undeniable, with over 80% of Canadians wanting their health information shared electronically between providers. The clinical data backs this up. For instance, Swift Medical's wound care technology has been shown to speed up wound healing by up to 35%. In a similar vein, digital care pathways from SeamlessMD have delivered impressive results. Sault Area Hospital, for example, reported 72% fewer emergency room visits and 64% fewer readmissions for its urology patients. You can discover more insights about how digital tools are delivering real-world results and transforming Canadian healthcare.
The Human Impact of Digital Health
Beyond the impressive stats, these stories point to a much bigger shift: a move toward a more proactive, patient-centred model of care. Digital tools are finally giving patients the resources they need to be active partners in their own health journey. At the same time, they're empowering clinicians with the data to provide more personalised and effective care.
These real-world examples prove that Canada's digital health transformation isn't just about adopting technology for technology's sake. It’s about achieving meaningful, measurable improvements in health that benefit everyone, from individual patients to the system as a whole.
Your Practical Roadmap to Digital Adoption
Jumping into the digital healthcare transformation in Canada isn't just about buying new software. It’s a deliberate journey that needs a clear plan, whether you're a small private clinic or a sprawling regional health network. The real key to success lies in a thoughtful approach that lines up technology with how you actually work and what your patients truly need.
This roadmap isn't a rigid, one-size-fits-all checklist. Think of it more as a framework to help you ask the right questions, build support within your team, and make sure new digital tools become a core part of your daily operations, not just another piece of software that gathers dust.
Stage 1: Assess Your Needs and Identify Pain Points
Before you can find the right solution, you have to get to the root of the problem. The first step is to take a good, hard look at your own organisation and pinpoint the most critical challenges you're facing. Is endless paperwork drowning your clinicians? Are communication gaps between your team and patients causing missed appointments or frustrating follow-ups?
Start by mapping out your current processes. More importantly, talk to your staff and your patients. This is how you move past vague complaints and uncover specific, actionable insights that will guide your decisions.
Common pain points that digital tools are great at solving include:
Administrative Overload: Manual scheduling, billing, and record-keeping that create errors and burn out your team.
Inefficient Communication: Still relying heavily on phone calls and fax machines for everything from patient reminders to referrals.
Fragmented Patient Data: Information stuck in different systems, making it impossible to see a complete picture of a patient's health history.
Limited Patient Access: Obstacles that make it a chore for patients to book an appointment, check their results, or ask a simple question.
By clearly defining these issues first, you can focus your search on technology that solves your biggest problems instead of getting dazzled by fancy features you'll never use.
Stage 2: Build the Business Case and Secure Buy-In
Once you know what needs fixing, your next move is to build a convincing case to get everyone on board. This is about more than just crunching numbers; it’s about telling a compelling story of how this change will make life better for everyone, from the front-desk staff to senior clinicians and, of course, your patients.
Your business case should lay out the expected return on investment, which includes both hard numbers and softer benefits. Think in terms of real-world outcomes like lower administrative costs, the ability to see more patients, and higher patient satisfaction scores. Getting key stakeholders on your side, especially the clinical leaders who will be using and championing the new tools, is absolutely crucial for building momentum.
A strong business case connects the dots between the technology investment and tangible improvements in care quality, operational efficiency, and patient outcomes. It answers the fundamental question: "How will this make us better?"
Stage 3: Choose the Right Technology Partners
Picking a vendor is one of the most important decisions you'll make. In Canada, this means looking far beyond a slick software demo. You need to dig deep into compliance, support, and whether a partner truly understands the local healthcare scene. To successfully navigate this complex journey, a comprehensive digital transformation roadmap guide is essential for organisations in Canadian healthcare, providing a clear pathway from strategy to implementation.
When you're evaluating potential partners, ask sharp, specific questions:
Compliance: How does your solution guarantee compliance with provincial privacy laws like PHIPA and federal rules like PIPEDA?
Data Sovereignty: Are your data centres located exclusively within Canada? This is a non-negotiable for many.
Interoperability: How well does your system play with existing hospital information systems or provincial health records?
Support and Training: What does your onboarding process actually look like? What kind of ongoing support can we expect when things go wrong?
Choosing a partner who gets the nuances of the Canadian healthcare system will save you a world of trouble down the line.
This graphic drives home the point that the right digital tools deliver real clinical benefits. It’s a clear line from technology adoption to better patient outcomes, reinforcing that this isn't just about efficiency; it's about faster healing and reduced strain on our hospitals.
Stage 4: Focus on Implementation and Change Management
This is where the rubber meets the road. A successful rollout is just as much about people as it is about technology. Change management isn't an afterthought; it needs to be woven into every single step. That means communicating transparently with your team, providing excellent training, and redesigning workflows with them, not for them.
Consider starting with a pilot program. Test the new system in one department or with a small group of users to iron out the kinks before a full-scale launch. And don't forget to celebrate the small wins along the way; it builds enthusiasm and shows everyone the real-world value of the new tools. Ultimately, the goal is to make the technology feel like a natural, indispensable part of how you deliver excellent care.
Frequently Asked Questions
As Canada's healthcare system continues its digital shift, a lot of questions pop up. From the practicalities of getting different systems to work together to the big-picture concerns about patient privacy, getting to grips with the details is essential. Here are some straightforward answers to the most common questions we hear.
What's the Biggest Challenge Holding Back Canada's Digital Healthcare Transformation?
Hands down, the single biggest hurdle is interoperability.
Imagine if your Rogers phone couldn't text a friend on Bell. Sounds ridiculous, right? That’s essentially the problem we have in healthcare. Hospitals, clinics, labs, and pharmacies often use different digital systems that were never designed to talk to each other.
This creates a mess of disconnected information silos. A family doctor might not be able to see a patient’s latest hospital discharge summary, or a specialist could be missing crucial lab results from another facility. This disconnect prevents seamless, coordinated care and often forces patients to become the human couriers of their own medical history, which is inefficient and can even be risky.
While Canadians are more eager than ever for digital health services, solving this complex technical puzzle is the most critical challenge we need to tackle.
How Is Patient Data Kept Private in These New Digital Systems?
Patient privacy isn't an afterthought; it's built into the very foundation of Canadian digital health, protected by a layered system of federal and provincial laws. At the national level, we have the Personal Information Protection and Electronic Documents Act (PIPEDA), which sets the ground rules for how all organisations handle personal data.
But because healthcare is managed provincially, each province has its own specific, often stricter, legislation. Ontario’s Personal Health Information Protection Act (PHIPA) is a perfect example. These laws dictate exactly how personal health information can be collected, used, and shared by everyone in the circle of care.
In the real world, this means any digital health tool must have iron-clad security features, including:
End-to-end encryption to shield data while it's in transit.
Strict access controls to make sure only authorised people can view patient files.
Clear consent processes so patients always know how their information is being used.
At its core, the principle is simple: patients own their health data. For technology developers, this means building solutions that are "private by design" and adhere to Canadian data sovereignty laws, which typically require that all patient data be stored on servers physically located within Canada.
What's the Federal Government's Role Versus the Provinces?
In Canada's decentralised health system, the federal and provincial governments play distinct but connected roles. Think of the federal government, through groups like Health Canada and Canada Health Infoway, as the guide and a key source of funding. It helps set national standards, pushes for interoperability, and provides money for digital health initiatives.
The provinces and territories, however, are on the front lines, responsible for actually delivering healthcare. This means each one decides how to build out and manage its own digital health infrastructure.
How Can Smaller Clinics Possibly Afford to Go Digital?
That’s a very real concern for many smaller practices, but the good news is that modern digital tools are no longer just for large hospitals. Several trends are making it much easier for small clinics to get on board without a massive budget.
First off, many provincial health authorities offer grants and incentive programs specifically to help smaller practices adopt certified Electronic Medical Record (EMR) systems. These programs can take a huge bite out of the initial setup costs.
Second, the move to cloud-based Software-as-a-Service (SaaS) has been a total game-changer. Instead of a huge upfront investment in servers and software licences, clinics can pay a manageable monthly subscription fee. This fee often includes maintenance, security, and support, making costs predictable and much lower over time.
Finally, tech companies are now offering solutions that can grow with a clinic. A small practice can start with the basics, like online booking and billing, and add features like telehealth or a patient portal when they're ready. For a small clinic, the key is to look at the clear return on investment that comes from running more efficiently, cutting down on paperwork, and giving patients a better experience.
At Cleffex Digital Ltd, we specialise in building secure, compliant, and scalable digital solutions that empower Canadian healthcare providers to thrive. We understand the unique regulatory and operational challenges you face and partner with you to implement technology that delivers real, measurable results.
Ready to start your digital transformation journey? Contact us today to learn how we can help.