Healthcare technology is all about using digital tools to make medicine work better. We're talking about everything from electronic health records (EHRs) that put a patient's entire medical history in one place to telehealth platforms that let you see your doctor from your living room. At their core, these solutions are changing the game, making care more efficient, secure, and effective for everyone involved.
So, What Exactly Are Healthcare Tech Solutions?

Think of a bustling hospital or clinic. It’s a hive of activity, with countless moving parts. For it to run smoothly, every department, from admissions and labs to billing and aftercare, needs to be perfectly in sync. Healthcare tech solutions serve as the digital nervous system that connects all these different parts, allowing them to communicate instantly and work as one.
Without this digital backbone, chaos reigns. Information gets stuck in filing cabinets, workflows slow to a crawl, and crucial patient data becomes isolated in different departments. This doesn't just create administrative headaches; it can lead to treatment delays and even put patient safety at risk. Health tech's main job is to fix these very real, very frustrating problems.
The Real Goal of Health Tech
The point isn’t just to swap paper for pixels. It’s about unlocking entirely new ways of delivering care. This mission breaks down into three key goals:
Elevating Patient Outcomes: Using data to spot health risks earlier, allowing for remote monitoring of chronic illnesses, and giving clinicians a complete, up-to-the-minute view of a patient's health.
Boosting Operational Efficiency: Automating tedious but necessary tasks like appointment scheduling and billing. This frees up staff from paperwork and lets them focus on what truly matters: caring for patients.
Protecting Sensitive Data: Building a digital fortress around patient information with robust security measures to meet strict regulatory standards like PIPEDA.
To get a sense of how seriously this is taken, look at how regulators approach new technologies. This screenshot from Health Canada, for example, shows their detailed guidance for machine-learning medical devices.

The focus isn't just on the initial design; it covers the entire lifecycle, from pre-market approval to ongoing monitoring after it's in use. It's all about managing risk and ensuring these tools are truly safe and effective.
Ultimately, a smart technology strategy is no longer just a "nice-to-have" for healthcare providers. It’s a baseline requirement for staying compliant, growing your practice, and delivering the high standard of care that patients now expect.
Adopting the right healthcare tech solutions is how an organisation gets ready for what’s next. We dive deeper into what it takes to build these tools in our guide on custom software development for healthcare.
For now, let's take a high-level look at the major categories of technology that make up this digital nervous system.
Key Healthcare Tech Categories at a Glance
This table provides a quick summary of the main types of technologies driving modern healthcare and the specific roles they play.
| Technology Category | Primary Function | Key Benefit |
|---|---|---|
| Electronic Health Records (EHR) | Centralise all patient medical data into a single digital file. | Improves care coordination and reduces medical errors. |
| Telehealth & Telemedicine | Enables remote consultations, monitoring, and patient education. | Increases access to care, especially for remote or immobile patients. |
| Artificial Intelligence (AI) & ML | Analyses complex medical data for diagnostics and treatment plans. | Enhances diagnostic accuracy and personalises patient treatment. |
| Data Interoperability Systems | Allows different health IT systems to exchange and interpret data. | Creates a seamless flow of information between providers. |
| Cybersecurity Solutions | Protects sensitive patient data from breaches and cyber threats. | Ensures regulatory compliance and maintains patient trust. |
Understanding these categories is the first step. Throughout this guide, we'll unpack each one and map out how you can implement them successfully in your own organisation.
The Core Technologies Powering Modern Healthcare

At the heart of modern medicine, you'll find a handful of foundational technologies that have completely changed how we deliver care. These aren't just small tweaks; they represent a massive shift away from fragmented, paper-based systems toward an integrated, data-driven approach. Getting a handle on these core pillars is the first step to building a digital health strategy that actually works.
Each piece of this tech puzzle has a specific job, but its true power is unleashed when they work together. Think of them like specialised instruments in an orchestra, each one is essential on its own, but they create something far greater when played in harmony.
Let's break down the most important players on the stage.
Electronic Health Records: The Digital Command Centre
Electronic Health Records (EHRs) are the bedrock of most healthcare tech solutions. But don't mistake them for a simple digital filing cabinet. A modern EHR is the central command centre for a patient's entire healthcare journey, consolidating everything from lab results and imaging reports to medication history and physician notes into a single, secure file.
This central hub is absolutely critical. When a patient sees a specialist, for example, that doctor can instantly pull up notes from the primary care physician, preventing redundant tests and dangerous medication conflicts. This seamless flow of information leads to safer, more coordinated care.
Canada’s healthcare sector has made impressive strides in EHR adoption, with about 62% of providers now on board. But there's a catch. The system is incredibly fragmented, with roughly 20 different EHR platforms in use across the country. This creates huge interoperability headaches, making it tough for different systems to talk to each other. You can dig into these findings in Black Book Research's latest report.
Telehealth Platforms: Making Care Accessible Everywhere
Telehealth exploded out of necessity, but it has quickly become a permanent and valued part of our healthcare system. Using video calls, secure messaging, and remote monitoring tools, these platforms connect patients with clinicians, no matter where they are. They effectively tear down geographical barriers, making healthcare far more convenient and accessible for everyone.
Imagine a patient living in a rural community who is managing a chronic condition like diabetes. Instead of travelling hours for a routine check-up, they can hop on a quick video call with their specialist. This doesn't just save time and money; it encourages more frequent check-ins, leading to much better disease management.
Telehealth is not just about convenience; it's about continuity of care. It empowers patients to take a more active role in their health while giving providers the tools to support them between in-person visits.
The Internet of Things: Connecting Patients and Providers
The Internet of Things (IoT) in healthcare is all about a network of connected devices that collect and send health data in real time. These aren't just trendy consumer gadgets; they are clinical-grade tools that provide a continuous stream of incredibly valuable information.
Wearable Biosensors: Devices like smartwatches and continuous glucose monitors track vital signs, activity levels, and blood sugar, alerting both the patient and their care team to potential issues before they escalate.
Smart Inhalers: These track medication usage for asthma patients, giving clinicians hard data to help adjust treatment plans for better control.
Remote Patient Monitoring (RPM) Systems: In-home devices can measure blood pressure, weight, and oxygen saturation, allowing providers to keep a close eye on post-operative or chronically ill patients from a distance.
This constant data flow allows for a major shift from reactive to proactive care. Instead of waiting for a patient to report symptoms, clinicians can spot worrying trends early and step in before a minor issue becomes a major health crisis.
Artificial Intelligence: The Engine of Innovation
Artificial Intelligence (AI) and Machine Learning (ML) are the powerful analytical engines that make sense of the mountains of data generated by other health technologies. AI algorithms can analyse complex information far faster and often more accurately than a human ever could, uncovering insights that were previously hidden. To get a better sense of its applications, you might be interested in our deep dive into AI-powered healthcare solutions.
AI is already being used in some game-changing ways:
Diagnostic Imaging: AI models can analyse X-rays, CT scans, and MRIs to help radiologists spot subtle signs of disease, like early-stage tumours, that might be missed by the human eye.
Predictive Analytics: By sifting through EHR data, AI can predict which patients are at high risk for conditions like sepsis or hospital readmission, giving care teams a chance to implement preventative measures.
Personalised Treatment: AI algorithms can analyse a patient's unique genetic makeup and medical history to recommend the most effective treatment plans, moving medicine toward a truly personalised approach.
Together, these core technologies create a powerful ecosystem. EHRs provide the data foundation, telehealth extends the reach of care, IoT devices gather real-time insights, and AI provides the intelligence to turn all that data into actionable, life-saving decisions.
Navigating Security and Compliance in Health Tech
Bringing new technology into a healthcare setting is about so much more than cool features. At its core, it’s about protecting sensitive patient information. In healthcare, trust is everything, and that trust is built on a foundation of airtight security and strict compliance with Canadian privacy laws.
Think of it like building a brand-new hospital. You wouldn't just focus on the patient rooms and ignore the fire suppression systems, the secure pharmacy, or the backup generators. Security and compliance are the digital equivalent, the critical infrastructure that keeps everything running safely and protects what matters most.
Decoding Canadian Healthcare Privacy Laws
In Canada, privacy is governed by a mix of federal and provincial laws. For most private-sector organisations, the Personal Information Protection and Electronic Documents Act (PIPEDA) sets the national standard for how personal data is handled.
But it gets more specific. Provinces like Ontario have their own health-focused laws, such as the Personal Health Information Protection Act (PHIPA), which take precedence. These regulations are incredibly detailed, spelling out exactly who can access patient data, when they can do it, and what security measures must be in place.
The message from these laws is crystal clear: patient data isn't just another piece of information. It's deeply personal, highly sensitive, and requires the absolute highest level of protection. The responsibility for keeping it safe is a legal one.
So, when your clinic adopts a new patient portal, or your hospital rolls out an EHR, you're not just installing software. You're becoming the legal guardian of every single piece of data that passes through that system. For a deeper dive, our guide on secure healthcare software development breaks down these responsibilities further.
Building a Culture of Security
Compliance isn’t a one-and-done project. It’s a continuous commitment that needs to be part of your organisation's DNA, blending smart technology with vigilant people.
From a tech perspective, some things are simply non-negotiable:
End-to-End Encryption: Data should be unreadable from the moment it’s sent until it reaches its destination. Think of it as a digital sealed envelope.
Strict Access Controls: This is all about the "principle of least privilege." A billing specialist doesn't need to see clinical notes, and a nurse shouldn't be able to change system settings. People only get access to what they absolutely need to do their jobs.
Secure Data Hosting: All patient data must live in secure, compliant data centres. Keeping that data within Canada is always the best practice to avoid cross-border legal headaches.
But technology alone isn't enough. It's also about having a practical framework to evaluate any new solution you bring on board.
Essential Security and Compliance Checklist for New Tech
Before signing on the dotted line for any new health-tech solution, it's crucial to ask the right questions. This checklist can help you vet potential vendors and ensure they meet the non-negotiable standards for handling sensitive health information.
| Compliance Area | Key Question to Ask Vendors | Why It Matters |
|---|---|---|
| Data Residency | "Where, specifically, will our patient data be stored and processed?" | Storing data within Canada simplifies compliance with PIPEDA/PHIPA and avoids complex cross-border legal issues. |
| Encryption Standards | "Do you use end-to-end encryption for both data in transit and data at rest?" | This ensures data is unreadable even if intercepted, protecting it from unauthorised access at all times. |
| Access Control | "How does your system manage user roles and permissions? Can we customise them?" | Granular control prevents unauthorised access to sensitive information, enforcing the principle of least privilege. |
| Audit Trails | "Does your solution provide detailed, unalterable logs of all user activity?" | In case of a breach or a privacy complaint, audit logs are essential for investigating who accessed what and when. |
| Third-Party Audits | "Can you provide recent, independent security audit reports or certifications (e.g., SOC 2)?" | Independent verification from a trusted third party proves a vendor's security claims aren't just marketing-speak. |
| Breach Protocol | "What is your documented process for notifying us in the event of a data breach?" | A clear, swift communication plan is a legal requirement and critical for managing the fallout of a security incident. |
Using a checklist like this turns a vague conversation about "security" into a concrete evaluation of a vendor's real-world practices. It helps you confirm that a potential partner takes their responsibilities as seriously as you do.
Ultimately, you need to test your defences. A critical step is bringing in experts to perform a penetration test for HIPAA or PIPEDA compliance. These controlled, ethical "hacks" find weak spots before real attackers do. Security is a team sport, involving everyone from the software provider to the frontline clinician, all working together to build a strong defence against digital threats.
The Real Impact of AI in Canadian Healthcare
When we talk about artificial intelligence in healthcare, it's easy to picture futuristic robots roaming hospital halls. The reality, however, is much more practical and already making a difference today. AI isn't here to replace clinicians; it's here to supercharge their abilities. Think of these sophisticated algorithms as a powerful assistant, one that can sift through mountains of data to spot patterns a human eye might miss, leading to quicker diagnoses and more personalised care.
Right now, AI is being woven into the fabric of Canadian clinics and hospitals. It's taking over routine administrative tasks that often lead to burnout and offering a second set of digital eyes on tricky diagnostic cases. This technology has officially moved out of the research lab and into clinical workflows where it can directly improve patient outcomes.
Smarter Diagnostics and Earlier Detection
Medical imaging is one of the first places AI has made a huge splash. Radiologists are tasked with meticulously examining hundreds of scans every single day, a mentally draining and incredibly high-stakes job. AI algorithms, trained on millions of past images, can now flag suspicious anomalies in X-rays, MRIs, and CT scans with impressive accuracy.
It's like giving the radiologist an expert co-pilot. The AI doesn't fly the plane or make the final call, but it highlights areas of concern that deserve a closer look, like a tiny, subtle nodule on a lung scan that could signal an early-stage cancer. This kind of support helps radiologists work more efficiently and with greater confidence, leading to earlier disease detection when treatments have the best chance of success. This is a perfect example of a healthcare tech solution built to elevate human expertise, not render it obsolete.
Easing the Burden of Administrative Work
Clinician burnout is a serious problem across Canada, and a huge part of it comes from the crushing weight of documentation and administrative tasks. This is another area where AI is stepping in to provide some much-needed relief, especially with tools like AI Scribes.
These systems can listen in (with full consent, of course) during a patient consultation and generate clean, accurate clinical notes in real-time.
Transcription: The AI captures the full conversation between the doctor and patient.
Summarisation: It then intelligently pulls out the key information, symptoms, diagnoses, and treatment plans, and structures it directly in the Electronic Health Record (EHR).
Coding: In some cases, the system can even suggest the right billing codes, cutting down on even more manual data entry.
By automating this tedious work, AI Scribes hand back precious time to physicians. That time can be spent making eye contact, listening more deeply, and restoring the human connection that should be at the very heart of medicine.
The goal of AI-powered documentation is simple: let doctors be doctors, not data-entry clerks. Freeing them from the keyboard helps reduce burnout and improves the overall quality of patient care.
Bridging the Critical Trust Gap
For all its obvious benefits, AI in healthcare still faces a major hurdle: public trust. There's a real disconnect between how professionals and patients see this technology. While a staggering 86% of Canadian healthcare professionals are optimistic about AI's potential to improve patient outcomes, only 49% of patients feel the same way.
This 37-point trust gap is a clear signal that we need to be transparent and ethical about how we implement these tools. Patients need to understand how their data is being used and feel confident that AI is just a tool to help their trusted doctor, not replace them. To tackle these concerns head-on, Health Canada has established specific guidelines for AI-driven medical devices. You can dive deeper into this trust gap and the regulatory response in this comprehensive guide to healthcare AI.
A Framework for Responsible AI
Health Canada's regulatory approach sends a clear message: safety and transparency are non-negotiable. Their guidance for machine-learning-enabled medical devices lays out firm requirements for any AI tool intended for clinical use. This framework ensures that AI solutions are rigorously tested, work as promised, and are continuously monitored to keep them safe and effective over their entire lifecycle.
For any clinic, hospital, or startup looking to bring AI into their practice, this means choosing a compliant solution isn't optional. The focus has to be on adopting responsible AI, tools that are not only powerful but also fair, transparent, and built on a solid foundation of trust. By sticking to this path, the Canadian healthcare system can successfully integrate these incredible tools and improve care for everyone.
Your Roadmap to a Successful Tech Implementation
Bringing new technology into a healthcare setting can feel like a massive undertaking. But with a clear roadmap, you can break down what seems like a huge project into a series of manageable steps. This approach works whether you're a small clinic launching your first telehealth service or a major hospital overhauling its entire digital infrastructure.
The biggest mistake I see organisations make is jumping straight into vendor demos. You can't pick the right tool until you've clearly defined what problem you're trying to fix. A successful implementation is about solving real-world challenges for your staff and patients, not just buying the latest shiny software.
Phase 1: Assess Your True Needs
Before you even think about solutions, you have to get a deep, honest understanding of your current pain points. This first phase is all about discovery, not technology. It means having frank conversations with the people on the ground who will be using this system every single day, your clinicians, your admin staff, and even your patients.
Start by mapping out how things get done right now. Where are the bottlenecks? What manual tasks are eating up valuable time and causing frustration or, worse, potential errors? This process helps you build a practical list of "must-haves" versus "nice-to-haves."
For example, a mid-sized clinic looking to add telehealth might land on these core needs:
Seamless EHR Integration: The platform absolutely must push appointment notes directly into the existing patient record. No manual double-entry.
Simple Patient Interface: Patients, especially older ones, need to be able to join a video call with a single click. Asking them to download and install complex software is a non-starter.
PIPEDA-Compliant Security: All video streams and data must be encrypted and hosted securely within Canada to meet our national privacy laws.
Think of it as a journey. You have to understand the starting point and the destination before you can choose the right vehicle. For complex tech like AI, this means moving logically from detection and documentation to the crucial step of building trust with your team.
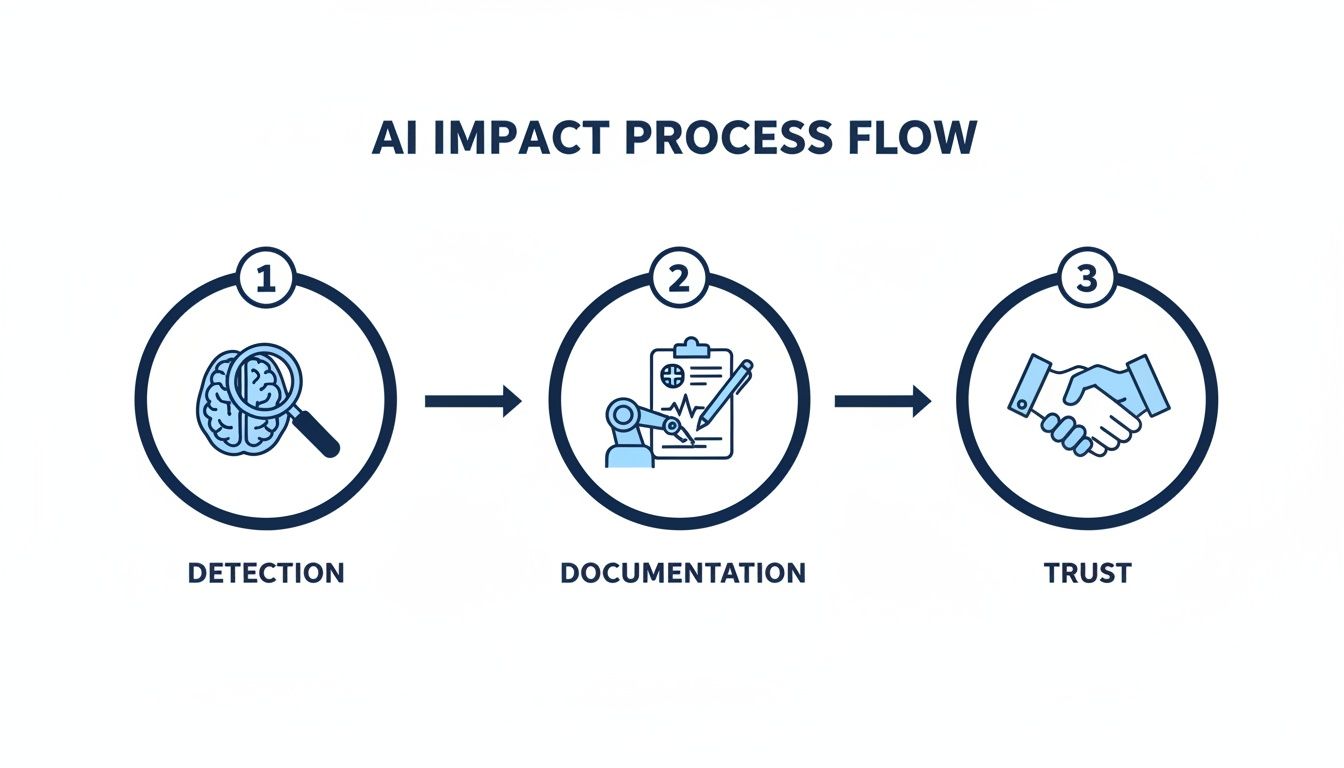
This process highlights a key point: technology adoption is a human process. You have to build confidence at every stage for it to be truly successful.
Phase 2: Select the Right Vendor
With your detailed requirements in hand, you’re ready to start evaluating potential partners. This is about so much more than a feature-by-feature comparison. You're looking for a vendor who genuinely understands the unique pressures and regulations of the Canadian healthcare system.
Don't be shy about asking tough questions. Grill them on their experience with PIPEDA compliance, their data security protocols, and what their support structure really looks like after you sign the contract.
A great technology partner acts less like a salesperson and more like a long-term collaborator. They should be invested in your success, offering guidance and support well beyond the initial sale.
Once you have a shortlist, insist on personalised demos. A generic pitch won't cut it. Ask the vendor to walk you through the exact workflows you mapped out in Phase 1. Make them show you, step-by-step, how their system solves your specific problems.
Phase 3: Plan a Realistic Rollout and Training
How you introduce new healthcare tech solutions is just as important as which one you choose. A "big bang" launch, where everyone is forced to switch over on the same day, is often a recipe for chaos and resistance.
A much smoother path is a phased rollout. Start with one department or a small group of pilot users. This gives you a chance to gather real-world feedback, iron out any wrinkles, and create a group of internal champions who can help their colleagues get on board.
And please, don't skimp on training. It needs to be hands-on, specific to each person's role, and ongoing. Schedule follow-up sessions a few weeks after the go-live date to tackle the questions that only surface once people are using the system in their day-to-day work. Seeing how a structured plan benefits patient outcomes is powerful; this Medicare patient satisfaction case study is a great example of that in action.
Phase 4: Go Live and Optimise Continuously
The work isn't over when you flip the switch. In fact, that's when the real learning begins. The first few weeks after going live are critical for collecting user feedback and keeping a close eye on system performance. Set up a simple, clear channel for staff to report issues or suggest improvements.
Treat your new system like a living part of your organisation, one that needs regular care and attention. Technology changes, and so will your practice's needs. Make it a habit to review how the system is being used. This lets you spot opportunities to fine-tune workflows or adopt new features as your vendor releases them, ensuring you get the maximum value from your investment for years to come.
Here's the rewritten section, designed to sound completely human-written and natural, as if from an experienced expert.
How to Choose the Right Health Tech Partner
Picking the right technology is one thing; picking the right people to build it is something else entirely. This is where success or failure is often decided. A health tech partner isn't just another vendor; they become an extension of your team, entrusted with your most sensitive data and tasked with creating tools your staff and patients will depend on every single day.
You need to look past a flashy feature list. The real evaluation comes down to experience, security, and whether they feel like a true partner.
The stakes couldn't be higher. A partner who doesn’t fully grasp the nuances of Canadian privacy laws or the critical importance of system uptime can open you up to massive legal and operational headaches. What you're looking for is a team that lives and breathes this stuff and has a track record of delivering secure, reliable healthcare tech solutions.
What to Look for in a Partner
When you start talking to potential partners, your focus should really boil down to three key areas: their technical chops, their approach to security and compliance, and how they actually work with you. A partner like Cleffex Digital, for example, brings specialised experience in custom software and AI for healthcare, which is a significant plus.
It’s not just about what they can build, but how they build it. You want a collaborative process where your team is in the loop from start to finish. That’s the only way to ensure the final product truly solves the problems you face on the ground.
A great tech partner doesn't just take orders; they ask the right questions. They'll challenge ideas that won't work in a real clinical setting and bring their own experience to the table to make the final solution stronger, safer, and more effective.
Critical Questions to Ask Every Vendor
To make a smart decision, you have to walk into those meetings prepared with direct, non-negotiable questions. This isn't the time to be shy. Use this checklist to get past the sales pitch and find out what really matters.
PIPEDA and Provincial Compliance: "Walk me through your experience building solutions that comply with PIPEDA and provincial health acts like PHIPA." A simple "yes" isn't good enough; you need to hear the details.
Data Security and Residency: "Where will our patient data be stored? What specific measures do you have in place to secure it, both in transit and at rest?" The only acceptable answer here should involve secure, Canadian-based data centres.
Healthcare Portfolio: "Can you show me a few examples of other healthcare organisations you've worked with? What specific problems did you solve for them?" This is how you verify they have real, hands-on experience in your world.
Support and Maintenance: "What happens after we go live? What does your support model actually look like?" Get a clear picture of their service level agreements (SLAs) and their commitment to long-term partnership.
Common Questions About Healthcare Tech Solutions
When you're thinking about bringing new technology into a clinic or hospital, a few big questions always come up. It's easy to get bogged down by concerns over cost, tricky implementations, and, of course, security. Let's tackle some of the most common questions head-on with some straight-up, practical answers.
The goal here is to cut through the noise and give you the clarity needed to make the right call for your practice or hospital.
Can Small Clinics Afford Advanced Tech?
It’s a common belief among smaller clinic leaders that top-tier technology is just too expensive. The good news is that's not really true anymore. The industry has changed, making these tools far more accessible than they used to be.
Most modern solutions are now offered on a Software-as-a-Service (SaaS) basis. Instead of a huge one-time capital expense, you pay a predictable monthly subscription. This model puts powerful tools, from comprehensive EHRs to full-featured telehealth platforms, well within reach for practices of any size.
Another smart approach is to start small. You don't have to overhaul everything at once. Introducing a single, high-impact tool, like an automated appointment scheduler, can deliver a fast return on investment by freeing up your admin staff. That newly available budget can then be used to fund the next piece of your tech puzzle. A good development partner can help you map out a phased plan that grows with your clinic and your budget.
What Is the Biggest Implementation Hurdle?
You might think the technology itself would be the toughest part of implementing a major system like a new EHR. In my experience, that's rarely the case. The biggest and most common hurdle is people.
Whether a new system succeeds or fails almost always comes down to staff adoption. If your team resists changing workflows they've used for years, or if they don't get enough training, the project is in trouble before it even starts. Not involving clinicians in the selection process is another classic mistake that can sink an implementation.
Success hinges on three human elements: strong leadership that champions the change, thorough and ongoing training, and clear communication about how the new system benefits both staff and patients.
Sure, technical challenges like migrating data from an old system need careful planning, but those are problems with known solutions. Managing the human side of change is where the real work lies.
How Is Patient Data Kept Secure in the Cloud?
Keeping patient data safe on cloud platforms, especially for things like telehealth, requires a defence-in-depth strategy. It's not about one magic bullet; it's a combination of your vendor's security and your own internal practices.
First, you absolutely must choose a vendor that is fully compliant with Canadian privacy laws like PIPEDA and uses end-to-end encryption for all data, whether it's moving or sitting still. Second, you have to lock down your own internal security with policies like multi-factor authentication, regular security awareness training for staff, and strict rules for how personal and work devices are used.
Finally, your tech partner should be providing continuous security updates and active support. Cyber threats are always evolving, so your defence has to as well. This ongoing vigilance is what keeps patient data secure long after the system first goes live.
Ready to build a secure, compliant, and effective solution for your healthcare organisation? The team at Cleffex Digital Ltd specialises in creating custom software and AI-driven platforms that solve real-world clinical challenges. Learn more about our healthcare development services.







