When people talk about healthcare digital transformation, they're talking about weaving technology into the very fabric of a healthcare organisation. This isn't just about buying new software or putting old files on a computer. It's a fundamental culture change that completely rethinks how you operate and deliver care to your patients.
What Is Healthcare Digital Transformation Anyway?

Let’s cut through the jargon. Think of it like swapping a paper road atlas for Google Maps. The point isn't just to have a digital version of the map; it’s about getting real-time traffic updates, finding the quickest route, and discovering points of interest you never knew existed. Digital transformation in healthcare works the same way; it’s not about digitising paper forms for the sake of it, but about reimagining the entire care journey.
This strategic shift forces you to look at how your clinic or hospital uses technology, people, and processes to build entirely new ways of working. The goal is to create a connected, intelligent, and patient-first ecosystem where information flows securely and effortlessly between providers, departments, and the patients themselves.
Moving from Analogue to Integrated Systems
At its heart, this transformation is about tearing down data silos. For decades, patient information has been locked away in filing cabinets or trapped in separate software systems that don't talk to each other. This kind of fragmentation leads to frustrating delays, repeated tests, and critical gaps in a patient's care history.
A digitally-forward organisation connects those dots. A patient's visit to a specialist instantly appears in their family doctor's records. New lab results automatically trigger an alert for the right clinician. This is what comprehensive healthcare IT modernisation looks like in practice, moving past clunky, outdated systems to build a smarter, more responsive foundation for care.
Comparing Traditional vs Digital Healthcare Models
To truly grasp the scale of this shift, it helps to see the old and new models side-by-side. The table below breaks down the core differences in how healthcare is managed and delivered.
| Core Pillar | Traditional Approach | Digital Transformation Approach |
|---|---|---|
| Patient Data | Stored in paper files or siloed digital systems. | Centralised in secure, accessible Electronic Health Records (EHRs). |
| Care Delivery | Primarily in-person visits during office hours. | A mix of in-person, telehealth, and remote monitoring. |
| Patient Engagement | Passive; patients receive information from providers. | Active; patients access their own data via portals and apps. |
| Decision-Making | Based on clinician experience and limited data sets. | Augmented by AI, predictive analytics, and real-time data. |
| Operations | Manual, paper-based administrative tasks (scheduling, billing). | Automated workflows, digital intake, and streamlined processes. |
This comparison highlights that digital transformation isn't just an upgrade; it's a complete re-engineering of the healthcare model to be more proactive, connected, and efficient.
The True Impact on Care Delivery
Ultimately, this whole evolution is driven by the need to improve three critical pillars:
The Patient Experience: Making healthcare easier to access, more convenient, and tailored to the individual. Think online appointment booking, virtual consults, and patient portals that put health records at their fingertips.
Clinical Outcomes: Using data and analytics to support sharper diagnoses, develop more effective treatment plans, and shift the focus from reactive treatment to proactive, preventative care.
Operational Efficiency: Automating tedious administrative work, smoothing out clinical workflows, and cutting unnecessary costs. This gives your staff more time to focus on what truly matters: caring for patients.
By zeroing in on these areas, healthcare digital transformation stops being a simple IT project and becomes a core business strategy. It aligns technology directly with the mission of providing better, safer, and more efficient care for everyone. The result is a healthcare system that's more resilient, adaptable, and ready to meet the expectations of modern patients.
Why Is This Transformation Happening Now?
The push for digital in healthcare isn't some fleeting trend. It's a direct answer to a perfect storm of converging pressures. For decades, the industry has relied on established, often paper-based, systems. But now, a mix of evolving patient expectations, serious operational strains, and major tech breakthroughs has turned digital adoption from a nice-to-have into a necessity.
This is about more than just swapping old tech for new. It’s a fundamental response to a world where people, used to the instant, seamless service they get from banking or retail, are starting to expect that same level of convenience and control from their healthcare.
The Rise of the Empowered Patient
Patients today see themselves less as passive recipients and more as active consumers of healthcare. They want on-demand access to their health records, easy ways to talk to their doctors, and simple digital tools to manage their own care. This consumer-driven mindset is a huge catalyst for change.
Just look at the numbers in Canada. In 2023, 39% of Canadians went online to check their health information, a big jump from 32% in 2021. But here's the disconnect: only 29% of physicians say they can electronically share clinical summaries with providers outside their own practice. That gap signals an urgent need for healthcare organisations to catch up with patient expectations. You can read more about how the Canadian system is adapting in our guide on digital healthcare transformation in Canada.
Escalating Operational and Financial Pressures
While patients are pushing from the outside, healthcare organisations are also dealing with immense internal pressures that make digital solutions essential. These challenges build a powerful business case for ditching inefficient, manual workflows.
Here are the big operational drivers:
Rising Costs: The price of delivering care just keeps going up. Digital tools help create efficiencies by automating administrative work, making better use of resources, and cutting down on preventable errors, all of which lead to real cost savings.
Staff Shortages and Burnout: Clinician burnout is a crisis. By automating repetitive tasks like charting and scheduling, digital systems can lighten the administrative load, freeing up skilled staff to focus on what matters most: patient care.
The Push for Value-Based Care: The industry is slowly moving away from paying for every service toward a model that rewards better patient outcomes. This value-based approach depends entirely on having strong data analytics and connected systems to track progress, coordinate care, and prove that treatments are working.
Simply put, the old ways of working are no longer sustainable. Digital transformation provides the tools to build a more efficient, resilient, and financially viable healthcare system that can withstand these mounting pressures.
A New Wave of Technological Maturity
Finally, the technology itself is no longer just a concept; it's mature, accessible, and secure enough for widespread use. What was once experimental is now proven and ready to be deployed at scale.
Cloud computing now offers a secure and flexible foundation for managing massive amounts of health data. Artificial intelligence (AI) and machine learning (ML) have become sophisticated enough to help with diagnostics and predict patient risks. And, of course, high-speed internet and smartphones in every pocket have made telehealth a practical and often preferred choice for millions.
These aren't just gadgets and software. They are the core enablers, the infrastructure needed to build the connected, patient-focused, and efficient healthcare ecosystem that today's world demands.
The Core Technologies Driving Modern Healthcare

The real engine behind healthcare’s digital shift is a handful of interconnected technologies. These aren't just buzzwords or futuristic concepts; they are practical tools being put to work right now to solve some of the oldest problems in healthcare, from clunky data management to gaps in patient care.
To really get a feel for how a modern clinic or hospital operates, it helps to see these technologies not as separate gadgets but as layers of a new digital foundation. Each one supports the next, creating a system that’s far more responsive and powerful than any single part. Let's look at the essential pieces making this happen.
Modernising Electronic Health Records
It all starts with upgrading the humble Electronic Health Record (EHR). For years, most EHRs were little more than digital filing cabinets. They were clunky, hard to search, and locked away inside a single hospital’s network, creating frustrating silos where a complete picture of a patient's health was nearly impossible to see.
Today’s EHRs are built differently. The keyword is interoperability, designing systems to speak a common language so data can flow securely between them. This is where standards like Fast Healthcare Interoperability Resources (FHIR) are game-changers. Think of FHIR as a universal translator that lets a specialist's system instantly and securely share notes with a family doctor's EHR.
Real-World Example: Imagine a patient ends up in the emergency department. Using a FHIR-enabled system, the ER doctor can immediately pull the patient's allergy list and current medications from their primary care physician's records. This simple data exchange can prevent a dangerous drug interaction and ensure care continues without a hitch.
The Power of Cloud Computing
Making this seamless flow of data possible is the cloud. Moving health records from ageing on-site servers to secure, compliant cloud platforms brings massive gains in scale, security, and access. Essentially, the cloud provides the heavy-duty infrastructure needed to handle the sheer volume of data modern healthcare generates.
Scalability: Cloud platforms can expand or shrink resources on demand, whether that means storing millions of patient files or processing huge, high-resolution medical images.
Security: Major cloud providers invest billions in security, offering advanced encryption and threat detection that often far exceeds what a single hospital could manage alone.
Accessibility: It lets authorised clinicians securely access patient information from anywhere, on any device, a must-have for supporting telehealth and remote teams.
This move to the cloud is what truly breaks down the physical walls around health information, making a connected care system a reality.
AI and Machine Learning in Diagnostics
Once data is accessible and organised, we can bring in the next layer: Artificial Intelligence (AI) and Machine Learning (ML). These aren't here to replace doctors but to give them superpowers. As a vital component of today's health tech, the integration of solutions like AI in healthcare is becoming standard.
Intelligent algorithms can sift through enormous datasets to spot patterns that would be invisible to the human eye. An AI, for instance, can be trained on thousands of medical scans to flag early signs of disease with incredible accuracy, pointing a radiologist exactly where to look. It’s about augmenting clinical expertise with powerful analytical tools.
Real-World Example: A dermatology clinic uses an AI tool to analyse pictures of skin lesions. The system instantly compares the image to a database of thousands of confirmed cases and gives the dermatologist a probability score for malignancy, helping them make faster, more confident decisions.
Expanding Telehealth and Remote Monitoring
Finally, all these foundational pieces come together to enable a more proactive and patient-centred model of care through telehealth and the Internet of Things (IoT). Telehealth is now much more than a video call. It includes everything from secure messaging and remote specialist consultations to continuous health monitoring.
IoT devices, like smartwatches, connected glucose monitors, or blood pressure cuffs, let clinicians gather real-time health data from patients right in their own homes. This constant stream of information is crucial for managing chronic conditions, catching problems before they escalate, and ultimately keeping people healthier and out of the hospital.
This is where you see the full circle. IoT devices collect data, the cloud stores and secures it, EHRs organise it, and AI analyses it. This gives providers the insights they need to deliver truly personalised and proactive care, regardless of where their patients are. This is the promise of digital transformation in healthcare, delivered.
Translating Technology Into Tangible Clinic Benefits
Jumping into new technology can feel like a massive undertaking, but the real value of digital transformation in healthcare shows up in measurable, real-world results. This isn't just about swapping old systems for new ones; it’s about building a smarter, more efficient, and patient-first practice.
The return on investment (ROI) really shines in three key areas: the patient’s experience, the quality of clinical outcomes, and the efficiency of your daily operations. When you put the right digital tools in place, you don't just digitise old processes; you open up entirely new ways to deliver and manage care.
Enhancing The Patient Experience
Today's patients expect the same convenience from their healthcare provider that they get everywhere else. A smart digital shift puts them right at the centre of their care, replacing frustrating paperwork and long waits with smooth, intuitive experiences that build trust.
Here’s how that actually looks in practice:
Reduced Wait Times: Think about online scheduling and digital intake forms. Patients can handle all the paperwork from home, which means no more front-desk bottlenecks and less time spent in the waiting room.
Personalised Communication: Automated reminders for appointments and follow-ups keep patients in the loop. Secure patient portals give them a direct line to ask questions, check lab results, and review their care plans whenever they want.
Greater Access to Care: Telehealth platforms break down geographical barriers. This is a game-changer for patients in remote areas or those with mobility challenges who need timely consultations.
Improving Clinical Outcomes
Beyond making things convenient, the core mission is always to deliver the best possible health outcomes. Digital tools give clinicians what they need to make sharper decisions, intervene earlier, and cut down on preventable medical errors.
When your systems can talk to each other, you get a complete picture of a patient's health history. This ensures diagnoses are based on comprehensive data, not just bits and pieces of information. For instance, a centralised EHR can prevent duplicate tests or flag potential drug allergies that might otherwise be missed. Better yet, IoT devices for remote patient monitoring enable proactive care, alerting clinicians to worrying trends in a patient's vitals long before a crisis hits.
By connecting disparate data points and providing powerful analytical tools, digital systems empower clinicians to shift from reactive treatment to proactive health management. This leads to safer care, better management of chronic conditions, and ultimately, healthier patients.
Gaining Greater Operational Efficiency
Perhaps the most immediate ROI you'll see is in streamlining the administrative and clinical tasks that eat up so much of your team's time. Automation and smarter digital workflows let your staff focus less on paperwork and more on patients. This is a huge factor in Canada’s booming digital health market.
In fact, Canada's digital health sector is on track to generate US$13.49 billion in 2024 and is expected to soar to US$53.92 billion by 2030. This incredible growth signals a massive push for efficiency and innovation across Canadian healthcare, and streamlined operations are a major driver.
Optimising workflows with the right tools is key. A well-designed system can automate billing, simplify insurance claims, and manage inventory, which reduces overhead and minimises costly mistakes. To see how this applies directly to your practice, check out our guide on the benefits of modern clinic management software development. This kind of operational excellence doesn’t just help your bottom line; it also helps prevent staff burnout by easing the administrative load.
Your Step-By-Step Digital Implementation Roadmap
Successfully navigating a digital shift in healthcare is about so much more than just buying new software. It demands a well-thought-out plan that considers every part of your organisation, from the technology you choose to the people who will be using it every single day. The most effective framework I've seen in my experience is built on three core pillars: People, Process, and Technology.
Think of these pillars as interconnected gears. If one is out of sync or gets ignored, the entire machine can grind to a halt. A solid roadmap addresses each one deliberately, building momentum and ensuring new systems actually deliver on their promise without throwing patient care into chaos. The secret is to start with a clear vision, solve a high-impact problem first to demonstrate early value, and then scale up your efforts from there.
This journey shows how investing in the right digital tools can directly elevate the patient experience, leading to better clinical outcomes and, ultimately, a more efficient clinic.
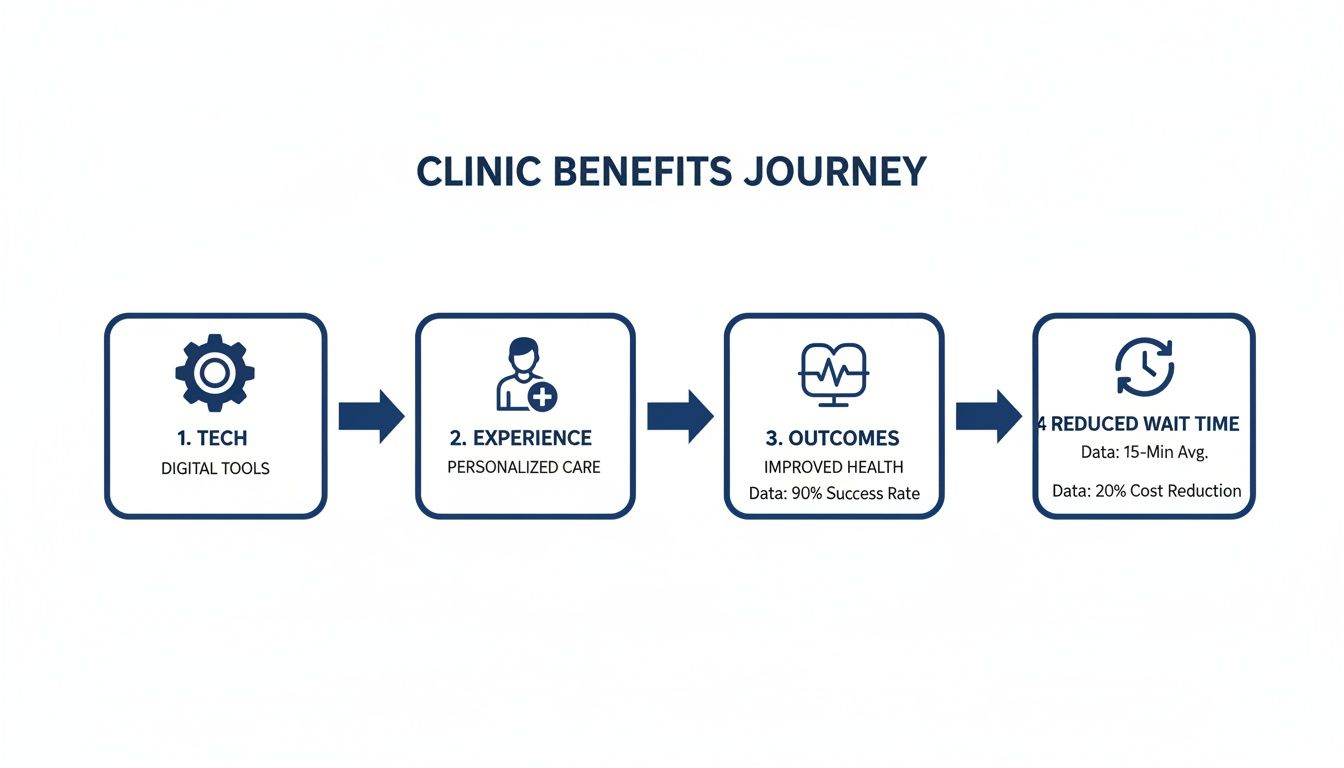
As you can see, technology is the catalyst, not the final destination. It’s what powers the human-centric benefits that truly define a successful transformation.
Phase 1: People First
Any new technology is only as good as the team using it. This is why your people have to be at the very centre of your plan from day one. Resistance to change is completely natural, especially in high-stakes clinical settings where established routines are there for safety and precision. Getting past this hurdle is all about communication and empowerment, not just top-down enforcement.
Start by creating a coalition of champions, respected clinicians and admin staff who genuinely see the potential and can advocate for the change among their peers. Their buy-in is absolutely critical for earning trust across the organisation.
From there, it’s all about clear and consistent communication.
Explain the 'Why': People are far more likely to get on board when they understand the problems you’re trying to solve. Frame the initiative around tangible benefits, like cutting down on tedious paperwork or making patient care safer.
Provide Robust Training: A one-size-fits-all training seminar rarely works. You need to offer role-specific, hands-on guidance that shows each person exactly how the new tools will make their specific daily tasks easier.
Create Feedback Channels: Set up open forums where staff can voice concerns and ask questions without judgment. When you actually act on that feedback, it shows you value their expertise and are committed to making the transition as smooth as possible for them.
A well-managed "people" strategy turns potential resistance into active engagement. When your team understands the vision and feels supported through the transition, they become the driving force behind a successful implementation.
Phase 2: Rethinking Your Processes
Once your team is on board, the next step is to take a hard look at your existing workflows. A classic mistake is simply layering shiny new technology on top of broken or inefficient processes. This is a surefire way to limit your ROI and create a lot of frustration. The goal here is to redesign how work gets done to take full advantage of your new digital capabilities.
Start by mapping out your current patient journey and key internal workflows. Pinpoint the bottlenecks, redundant steps, and manual tasks that eat up valuable time. Where do communication breakdowns happen? Where is the same data being entered over and over again?
With a clear picture of the current state, you can start redesigning those pathways. For instance, a clunky appointment scheduling process full of phone tag and paper calendars can be reimagined as a fluid digital workflow. Patients could book online, get automated reminders, and fill out intake forms from home, drastically cutting down the front-desk workload and patient wait times. This kind of process redesign is a core part of any meaningful healthcare digital transformation.
Phase 3: Selecting The Right Technology
The final pillar is, of course, choosing and implementing the technology itself. This phase should only start after you have a deep understanding of your people’s needs and your process improvement goals. A common pitfall is getting wowed by a long list of features without first considering how a solution will actually fit into your redesigned workflows.
To guide you, we've put together a high-level checklist that breaks down the key stages of implementation.
Digital Transformation Implementation Checklist
This checklist provides a framework for healthcare organisations to follow, ensuring a structured approach from initial planning to long-term success.
| Phase | Key Action Items | Primary Focus |
|---|---|---|
| 1. Discovery & Strategy | – Define clear objectives (e.g., reduce wait times by 15%). – Form a cross-functional leadership team. – Secure budget approval. | Aligning the project with organisational goals and establishing leadership. |
| 2. People & Process | – Identify and engage clinical champions. – Map current-state workflows. – Redesign future-state processes. | Gaining buy-in from staff and optimising workflows before tech selection. |
| 3. Technology Vetting | – Define technical requirements. – Research vendors with healthcare expertise. – Conduct demos and check references. | Choosing a solution and partner that fits the redesigned processes and culture. |
| 4. Implementation & Go-Live | – Develop a phased rollout plan. – Configure and test the system. – Execute role-based training programs. | Deploying the technology with minimal disruption to patient care. |
| 5. Post-Live Optimisation | – Gather user feedback. – Monitor key performance indicators (KPIs). – Plan for continuous improvement and updates. | Ensuring long-term adoption, measuring ROI, and evolving the system. |
By following a structured path like this, you move from a vague idea to a concrete plan. Your technology assessment should break down into a few key steps:
Assess Your Current Infrastructure: Take stock of your existing IT systems, from network capacity to data security protocols. This helps you spot any foundational upgrades you'll need before bringing in new platforms.
Define Your Requirements: Using your process analysis as a guide, create a detailed list of what you need the technology to do. What specific problems must it solve?
Select the Right Partner: Look for technology partners who have a proven track record in healthcare and truly understand compliance requirements like PIPEDA. A real partner offers more than just software; they provide implementation support, training, and ongoing service.
By approaching your implementation in this order, People, Process, then Technology, you ensure your investment is tied directly to your organisation's goals and is truly set up for success from the start.
Navigating Security, Compliance, and Staff Adoption
Getting new technology up and running is really just the start. In healthcare, even the best-laid plans can hit a wall if you don't tackle two critical challenges head-on: maintaining rock-solid security and compliance, and getting your team to actually use and like the new tools.
Bringing technology into the fold introduces incredible efficiencies, but it also dials up the responsibility. Protecting sensitive patient information isn't just a best practice; it's a legal and ethical cornerstone of modern healthcare. In Canada, that means every system you build has to be fully compliant with regulations like the Personal Information Protection and Electronic Documents Act (PIPEDA).
This is about much more than just installing the latest security software. It demands a security-first mindset woven into every layer of your digital strategy.
Data Encryption: All patient data, whether it's sitting on a server or moving between systems, must be encrypted. Think of it as an unbreakable code that makes information completely unreadable to anyone without the right key.
Secure Cloud Architecture: Working with cloud providers who live and breathe healthcare security is non-negotiable. This ensures your data is stored in environments with world-class physical and digital safeguards.
Strict Access Controls: Not everyone needs to see everything. By implementing role-based access, you ensure team members can only view the specific information required for their jobs, drastically cutting the risk of internal data leaks.
If you're looking to go deeper on this, we've put together a comprehensive guide on secure healthcare software development.
Overcoming Staff Resistance to Change
Here’s the thing: the most brilliant system in the world is useless if your team won't use it. Resistance isn't a sign of stubbornness; it's a natural human response, especially in a field where established routines are built for safety and precision. The trick is to manage this change with empathy, not force.
A classic misstep is focusing only on what's changing while forgetting to explain why. People are much more likely to get on board when they see how new tools make their jobs better and improve patient outcomes. Frame the change around less paperwork, fewer errors, and more time for what really matters: caring for patients.
A study found that while 75% of U.S. hospitals use EHR systems, many clinicians report serious burnout and frustration due to poor training. This is a powerful reminder: new technology without proper support can easily create more problems than it solves.
To get genuine buy-in, you need to cultivate a culture that champions support and innovation from the ground up.
Identify and Empower Champions: Find those respected clinicians and administrators who are genuinely excited about the new technology. Their enthusiasm and endorsement will be far more convincing to their colleagues than any memo from management.
Provide Role-Specific Training: One-size-fits-all training doesn't work. A nurse interacts with the system differently from someone in billing, and your training needs to reflect those real-world workflows.
Establish Open Feedback Loops: Create channels where staff can safely share their frustrations, ask questions, and offer suggestions. When you actively listen and respond to their feedback, it shows you respect their expertise and helps build trust in the entire process.
Common Questions About Digital Transformation Answered
Stepping into a digital transformation project is a big move, and it’s natural for leaders to have questions. To help clear things up, we’ve put together some straightforward answers to the most common concerns we hear from clinics and hospitals.
How Do We Start With A Limited Budget?
The trick is to start small and think in phases. You don’t need to find a massive budget to get the ball rolling. Instead, look for a high-impact project that won’t break the bank but will solve a real, nagging problem, like setting up a secure patient portal to cut down on phone tag and administrative busywork.
A solid needs assessment is your best friend here. It’ll help you zero in on the one thing that causes the most headaches for your team or your patients. By tackling that one problem first, you get a quick win and a clear return on your investment. That early success builds momentum and makes it much easier to get buy-in for the next phase.
What Is The Biggest Mistake To Avoid?
Without a doubt, the most common pitfall is getting completely wrapped up in the technology and forgetting about the people who have to use it every day. Just buying a new piece of software and dropping it into an old, clunky workflow is a surefire way to fail. The tech is just a tool; its real power comes from how people use it.
A successful strategy looks at the whole picture. It has to consider the human side, how this new system actually makes a nurse's shift less stressful, and the process side, making sure the technology fits into a genuinely smarter workflow, not just different. If you ignore these parts, you're just not going to see the results.
How Does This Affect Patient Data Security?
This is a big one, and it’s a valid concern. But here’s the thing: modern digital systems, when set up properly, are often a huge step up in security. A lot of older, on-site systems are surprisingly vulnerable. In contrast, today’s top platforms are designed from the ground up with security baked in.
Think of things like end-to-end encryption for every piece of data, strict access controls that ensure only the right people see sensitive information, and secure cloud infrastructure managed by experts who live and breathe healthcare compliance. The key is to partner with someone who has a proven track record of protecting health information.
Ready to start your clinic’s transformation journey with confidence? Cleffex Digital Ltd builds secure, compliant, and user-friendly software solutions that align with your budget and goals. Learn how we can help you take the first step.







