Patient engagement technology isn't just another set of digital tools; it's what builds a bridge between patients and healthcare providers, transforming the relationship from a series of occasional office visits into an ongoing partnership. Think of it as giving patients a dedicated health co-pilot, empowering them to take an active role in their own care journey.
What Is Patient Engagement Technology

Traditionally, the patient's role was often passive. You'd get a diagnosis, follow the instructions, and have very little contact with your doctor between appointments. Patient engagement technology flips that entire model on its head. It’s a collection of platforms and apps built to open up communication, share educational resources, and give patients direct, secure access to their own health information.
This transforms healthcare from a series of disconnected events into a continuous, collaborative dialogue. Instead of saving up questions for a yearly check-up, patients can now message their doctor securely, see lab results as soon as they’re ready, or get automatic reminders to take their medication.
From Passive Recipient to Active Partner
At its heart, this technology is about turning patients into active partners in managing their health. When people have the right tools to understand their condition and see their progress, they're far more likely to stick to treatment plans and adopt healthier habits. This isn't just a feel-good idea; it's a proven way to get better clinical results.
Take, for instance, a person managing diabetes. They might use a mobile app that syncs with their glucose monitor. The app doesn’t just log their blood sugar levels; it can also send that data straight to their care team. This allows for quick, proactive tweaks to their treatment, a level of connected care that was simply out of reach a decade ago. It’s also worth exploring other ways tech is improving healthcare in our guide to AI-powered healthcare solutions.
This approach shifts healthcare from a model of periodic intervention to one of continuous support. It gives patients the information and tools they need to take control of their well-being, building a stronger, more trusting relationship with their providers.
To give you a clearer picture, here’s a breakdown of what these technologies actually do.
The Core Functions of Patient Engagement Technology
| Function | Description | Example Tool |
|---|---|---|
| Information Access | Provides patients with secure, on-demand access to their personal health records (PHRs), including lab results, diagnoses, and medication lists. | Patient Portals |
| Communication | Facilitates direct, secure messaging between patients and their care teams, enabling quick questions and follow-ups without a phone call. | Secure Messaging Apps |
| Education | Delivers targeted educational materials, such as articles and videos, relevant to a patient's specific condition or treatment plan. | Health & Wellness Libraries |
| Self-Monitoring | Allows patients to track vital signs, symptoms, or lifestyle data (e.g., blood pressure, glucose levels, diet) and share it with their provider. | Remote Patient Monitoring (RPM) |
| Administrative Tasks | Simplifies tasks like appointment scheduling, prescription refills, and bill payments, reducing administrative workload for clinic staff. | Online Schedulers & Bill Pay |
These functions work together to create a more transparent, convenient, and collaborative healthcare experience for everyone involved.
Why It Matters for Modern Clinics
For small and mid-sized clinics across Canada, adopting patient engagement technology is no longer an optional extra; it's a core part of providing modern care. It helps streamline daily operations, cuts down on administrative headaches, and significantly boosts patient satisfaction and loyalty.
The evidence speaks for itself. A major review of information technology platforms for patient engagement found that 88.8% of studies showed positive impacts on patient behaviour, with most reporting high levels of improvement. You can read the comprehensive research on these positive patient engagement outcomes. This data confirms that these digital tools are successfully helping patients become more involved and invested in their own healthcare journey.
Exploring the Types of Patient Engagement Tools

Patient engagement technology isn't just one single piece of software. It’s more like a digital toolkit, with different solutions designed to smooth out specific parts of the patient journey, from accessing records to managing a chronic condition from the comfort of home. Getting to know these different tools is the first real step in building a strategy that actually helps patients and supports your clinical staff.
These tools are at their best when they work together, creating a seamless, connected experience. Let's unpack the six main categories that form the backbone of any modern patient engagement strategy and look at how they function in the real world.
Patient Portals: The Digital Front Door
Patient portals are probably the most familiar piece of patient engagement technology out there. Think of a portal as your clinic’s secure, always-on digital front door. It’s a central hub where patients can log in to check their lab results, see upcoming appointments, review their medication lists, and send secure messages to their care team.
For instance, after a routine check-up, a patient might get an email saying their blood test results are ready. Instead of playing phone tag or waiting for a follow-up call, they can just log into the portal, see the results along with their doctor's notes, and message back with any questions. It’s a simple process that saves a ton of administrative time and puts health data directly into the patient's hands.
Among the different tools available, dedicated medical appointment scheduling software is a cornerstone for boosting access and convenience, and it’s often built right into these portals.
Mobile Health Apps: Health in Your Pocket
Mobile health (or mHealth) apps take all the power of a patient portal and stick it right in a patient’s pocket. These apps are built for on-the-go access and often come packed with features designed for specific health needs, like diabetes management, heart monitoring, or mental wellness tracking.
Imagine a patient who was just diagnosed with hypertension. Their doctor could recommend an mHealth app where they log daily blood pressure readings, get reminders to take their medication, and find helpful articles on lifestyle changes. The app could even be set up to send that data right back to the clinic's EHR, letting the care team keep an eye on things without needing constant in-person visits.
Telehealth Platforms: Erasing Distance
Telehealth platforms use video conferencing and other digital tools to connect patients and providers from a distance. This tech became a household name during the pandemic, but its value goes far beyond public health crises. It effectively tears down geographical barriers, making healthcare far more accessible for people in rural areas or for those who have trouble getting around.
A simple follow-up for a stable, chronic condition can easily happen over a video call. This saves the patient a trip, gas money, and time off work, which in turn makes it much more likely they'll actually attend those crucial check-ins they might have otherwise skipped.
Telehealth is more than just a video call; it represents a fundamental shift in how care is delivered. It prioritises patient convenience and ensures continuity of care, regardless of physical location.
Automated Communication and Reminders
Appointment no-shows are a huge drain on any clinic's resources. Automated communication systems tackle this problem head-on by sending timely reminders via text, email, or a quick automated call. But they can do so much more than that.
These systems can also be programmed for:
Preventive Care Nudges: Letting patients know they're due for a flu shot or an annual screening.
Post-Visit Follow-ups: Sending a quick summary of care instructions or a link to a patient feedback survey.
Billing Notifications: Alerting patients when a new statement is available to view in their portal.
This level of automation frees up your admin staff from making hundreds of manual phone calls, letting them focus on the more complex, human-to-human parts of their job. To see how much automation is changing the game, it's worth reading about the role of a virtual assistant in healthcare.
Remote Patient Monitoring: Virtual Check-Ins
Remote Patient Monitoring (RPM) is all about using digital devices to collect health data from patients while they're at home. These devices, like connected blood pressure cuffs, glucometers, or smart scales, send data directly to the healthcare provider for review.
RPM is a game-changer for managing chronic diseases like congestive heart failure or COPD. A single care manager can monitor the daily vitals of dozens of patients, getting an alert if any reading falls outside a safe range. This allows the clinical team to step in early, often preventing a costly trip to the emergency department or a hospital readmission.
AI-Driven Personalisation
The most sophisticated patient engagement tools now use Artificial Intelligence (AI) to make the experience deeply personal. AI algorithms can analyse a patient's health records, preferences, and even their behaviour to deliver relevant educational articles, customised care plan reminders, and proactive health tips. This ensures every patient gets information and support that’s truly tailored to their unique health journey.
Here is the rewritten section, crafted to sound natural and human-written by an experienced expert.
The Real-World Benefits for Clinics and Patients
Bringing patient engagement technology into your practice is about much more than just a tech upgrade. It fundamentally changes the dynamic between appointments, creating a healthcare environment that’s more connected, efficient, and genuinely collaborative. When done right, it’s a win-win for everyone involved.
For patients, the impact is immediate and personal. Giving people the tools to take an active role in their own care journey provides a sense of ownership and clarity that’s often missing in traditional healthcare. This feeling of empowerment naturally leads to better decisions and, ultimately, better health.
For Patients: Taking Control and Improving Health
Think about someone managing a chronic condition like diabetes. Instead of just seeing their doctor every few months, they can now use a mobile app to log their blood sugar, get automatic medication reminders, and pull up articles on diet and exercise anytime. This creates a constant feedback loop that keeps them on track with their treatment plan day in and day out.
This is especially critical when you consider how many people live with long-term health issues. The demand for these tools in Canada has skyrocketed, largely driven by the need for better chronic disease management. For example, about 1 in 12 adults in Canada, that's 2.6 million people over 20, are diagnosed with some form of heart disease each year. These aren't one-off illnesses; they require ongoing communication and support, which is exactly what this technology provides. You can dig deeper into the drivers behind the Canadian patient engagement market to see the full picture.
Here’s what this looks like for the patient:
Actually Sticking to the Plan: Simple, automated reminders and easy-to-find care plans make following a doctor's advice far less of a chore.
Understanding Their Own Health: Having trusted educational resources at their fingertips helps patients make sense of their condition.
Convenience That Matters: Booking appointments, renewing prescriptions, or checking lab results online eliminates phone tag and waiting room frustration.
A Stronger Connection to Their Doctor: Secure messaging and video calls build a real sense of partnership and trust with the care team.
For Clinics: Boosting Efficiency and the Bottom Line
The perks for clinics are just as powerful, hitting everything from daily workflows to financial stability. Adopting patient engagement technology isn't just an IT project; it's a smart business move that tackles some of the most stubborn operational headaches in healthcare.
It really boils down to an investment in efficiency. Every automated reminder is a phone call your staff doesn't have to make. Every question handled through a secure message frees up your front desk for the person standing right in front of them.
One of the first things clinics notice is a sharp drop in no-shows. Missed appointments are a direct hit to revenue, and automated reminders are incredibly effective at getting that money back in the door.
Beyond that, these tools help your practice scale. Telehealth, for instance, lets you see patients who live hours away, opening up entirely new communities without the cost of a new physical location.
By automating all those routine tasks, scheduling, refill requests, and intake forms, you lighten the load on your administrative team. This doesn't just cut down on operational costs; it also improves morale by letting your staff focus on what they do best: interacting with and caring for patients. The result is a practice that runs smoother, is more profitable, and puts patients first.
Navigating Critical Integration and Compliance Challenges
Bringing powerful new tools into your clinic is about more than just picking shiny new features. Before you can truly benefit from patient engagement technology, you have to clear two major hurdles: making sure it works seamlessly with your existing systems and following data privacy laws to the letter.
Getting these two things right isn't optional. It’s essential for protecting patient data and making sure your new tech is a help, not a hindrance.
Think of it like adding a specialised app to your smartphone. If it can't sync with your contacts or calendar, its usefulness plummets. In the same way, your patient engagement platform has to "talk" to your Electronic Health Record (EHR) system. This connection is called interoperability, and it’s what lets information flow freely and accurately between your systems. It prevents data from getting trapped in separate silos and saves your staff from the soul-crushing task of manual double-entry.
Ensuring Seamless System Integration
When your systems are properly integrated, a patient booking an appointment online automatically populates in your EHR schedule. When lab results are in, they can be pushed straight to the patient portal without a staff member needing to manually upload anything. That kind of fluid connection is the foundation of an efficient, modern practice.
The good news is that Canada's healthcare infrastructure has already done much of the heavy lifting. The digital groundwork is already there. A staggering 96% of hospitals have adopted EHR systems, and 78% of office-based physicians are on board as well. This widespread adoption means the digital framework needed to support patient engagement solutions is largely in place. You can read more about the surge in patient-centric health IT to see how far we've come.
Demystifying Healthcare Compliance
Beyond the technical nuts and bolts, you have to navigate the legal side of patient privacy. In Canada, the main piece of legislation is the Personal Information Protection and Electronic Documents Act (PIPEDA), although some provinces have their own very similar health privacy laws.
These aren't just bureaucratic hoops to jump through; they are crucial rules designed to protect sensitive patient information from falling into the wrong hands. It’s your responsibility to choose a patient engagement vendor that is fully compliant. This means verifying they have rock-solid security measures, including:
End-to-End Encryption: This protects data whether it's sitting on a server or moving between systems.
Access Controls: This ensures only authorised staff can see specific patient information.
Regular Security Audits: These proactively find and fix potential weak spots.
Following privacy laws like PIPEDA isn't just about avoiding hefty fines. It’s about upholding the trust your patients have in you. A single data breach can do permanent damage to your clinic's reputation.
A huge part of this process involves carefully vetting any third-party tools. For example, if you wanted to use a survey tool to gather patient feedback, you'd need to ask serious questions like "Is SurveyMonkey HIPAA Compliant?" This level of scrutiny is necessary for any software that touches patient data.
When you're talking to potential vendors, always ask for their compliance documentation and security protocols. A partner you can trust will be open and transparent about how they protect patient information, which lets you focus on what you do best: providing excellent care. For a deeper dive into this, our guide on clinic management software development can help.
Your Step-By-Step Implementation Roadmap
Bringing new patient engagement technology into your practice can feel like a massive undertaking, but a solid plan makes all the difference. This roadmap breaks the process down into clear, manageable steps to guide you from the initial idea all the way to a successful launch and beyond. Think of it as a blueprint for implementing a solution that actually meets the needs of your patients and your team.
This whole process is about creating a bridge. Data needs to flow from your core systems, through the engagement platform, and into the hands of your patients to truly empower them.
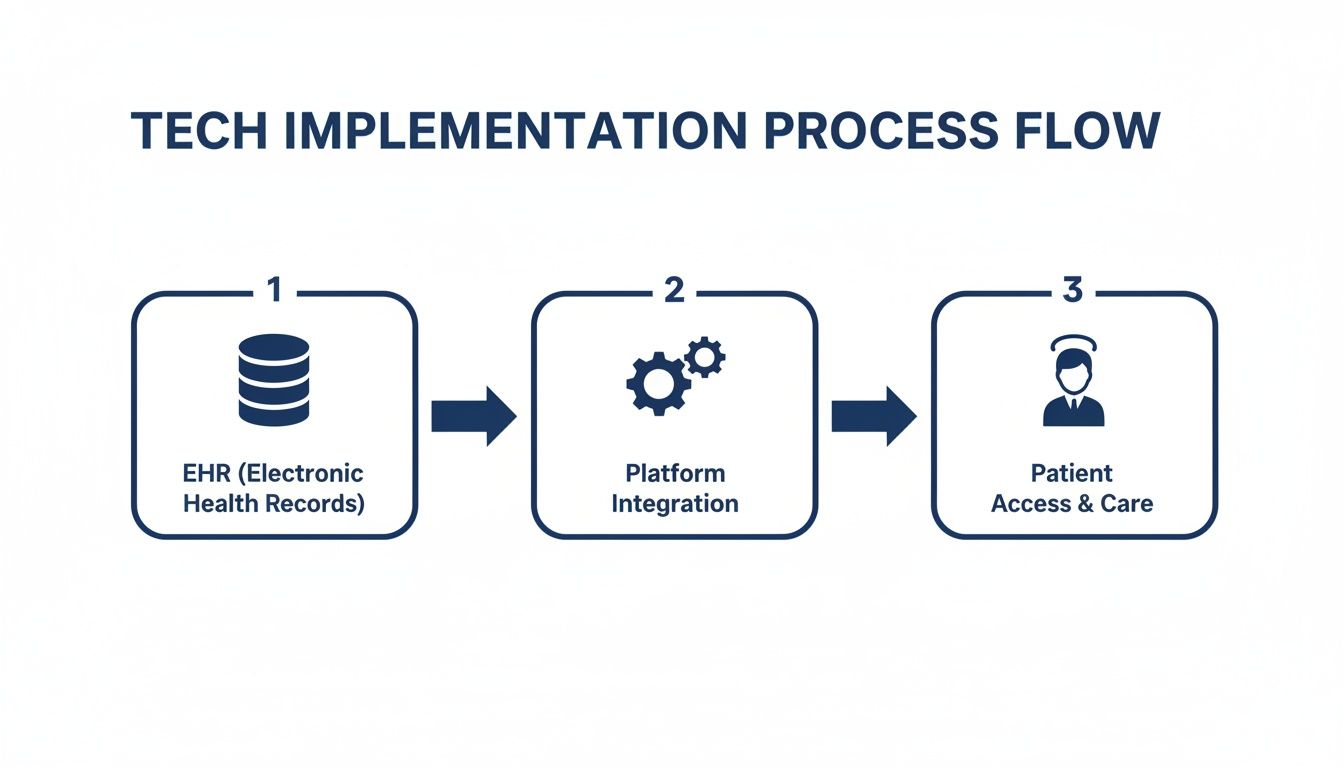
As you can see, a successful rollout hinges on seamless integration. The platform you choose has to work in harmony with your internal records to create a great end-user experience for patients.
Step 1: Assess Your Clinic and Set Goals
Before you even think about looking at software, you need to look inward. Where are the biggest communication bottlenecks in your practice right now? Are your phone lines constantly jammed with appointment requests? Do you struggle with a high no-show rate that hurts your bottom line?
Start by identifying your top three to five pain points. Then, turn those problems into real, measurable goals. A vague goal like "improve communication" isn't helpful. Instead, aim for something specific, like "reduce administrative phone calls by 20%" or "decrease our no-show rate by 15% within six months." These concrete targets will be your north star through this entire process and make it easy to measure success later on.
Step 2: Choose the Right Technology Partner
With your goals clearly defined, you can start evaluating vendors. It's easy to get distracted by flashy features you'll never use, so stay focused. You're looking for a partner whose solution directly solves the problems you identified in step one.
Most importantly, you must confirm that any platform you're considering can integrate smoothly with your existing Electronic Health Record (EHR) system. You also have to verify their compliance with Canadian privacy laws like PIPEDA. A trustworthy vendor will be completely transparent about their security protocols and how their system connects with yours.
"A successful implementation is less about the technology itself and more about finding a true partner. Choose a vendor who understands your clinical workflows and is committed to supporting your staff and patients through the transition."
Step 3: Plan Your New Workflows
New technology always changes how work gets done; that’s the point. Take the time to map out exactly how your current processes will be affected. For instance, who will be responsible for responding to secure patient messages? How will your front desk staff manage online appointment bookings alongside the usual phone calls?
Get your team involved in this planning stage. They're on the front lines every day and will have invaluable insights into what will actually work in practice. This kind of collaboration builds buy-in from the start and makes for a much smoother transition when the technology finally goes live.
Step 4: Train Your Staff to Be Advocates
Your staff will be the champions of this new technology. Proper training isn’t just about showing them which buttons to click; it’s about helping them understand the "why" behind the change. Take the time to explain how the new tools will make their jobs easier and, ultimately, improve patient care.
When your staff is well-trained, they can confidently guide patients through using a new portal or app. If they believe in the system, their enthusiasm is contagious and plays a huge role in getting patients on board.
Step 5: Educate and Onboard Your Patients
Your patients won't use technology they don't know about or don't understand. You need a simple, clear communication plan to introduce them to the new tools.
Here are a few ideas that work well:
In-Clinic Promotion: Put up posters and flyers in your waiting room.
Staff Introductions: Have your front desk team briefly explain the benefits when patients check in.
Email Campaigns: Send out a straightforward, step-by-step guide on how to register and start using the platform.
Make the benefits crystal clear to them, always focusing on convenience. Frame it as "you can now book appointments anytime" or "get your lab results without ever making a phone call."
Step 6: Launch, Gather Feedback, and Improve
Launch day is just the beginning, not the finish line. Once the system is live, pay close attention to adoption rates and user feedback. Are patients actually signing up for the portal? Are they using the secure messaging feature?
Check in regularly with both your staff and your patients to find out what's working and what isn't. Use that feedback to make continuous improvements. A great patient engagement technology strategy isn't a "set it and forget it" project; it's an ongoing process of refinement to better serve your clinic and your community.
The Future of Patient Engagement
Where is patient engagement heading next? The tools we're using today are impressive, but they’re really just the first chapter. The future is all about making healthcare more proactive, deeply personal, and woven into the fabric of our daily lives.
These aren't far-off, sci-fi concepts; they're the natural next steps in giving patients more control over their health. The goal is to build a system where care is continuous and data-driven, creating a true partnership between patients and their care teams. For any practice that wants to lead the pack, keeping an eye on these trends is non-negotiable.
The Rise of AI and Hyper-Personalisation
Artificial Intelligence (AI) is quickly becoming the brain behind the next wave of patient engagement. Today's systems are great at sending reminders or educational articles, but AI is about to take that to a completely different level. It can look at a patient's entire health record, combine it with real-time data from their smartwatch, and even learn their communication style to offer support that feels truly individual.
Picture this: instead of just a generic "take your meds" alert, a system notices a dip in a patient's activity levels and suggests a short walk at the time of day they're most energetic. That's the difference between reactive and proactive care. We're talking about using data to get ahead of problems before they even start.
The Internet of Medical Things (IoMT)
The Internet of Medical Things (IoMT) is all about the growing ecosystem of connected health gadgets, smart glucose monitors, blood pressure cuffs, fitness trackers, and even smart scales. These devices collect a constant stream of health data from a patient's real life, not just from the few minutes they spend in an exam room.
This firehose of data gives clinicians a completely new perspective. Instead of seeing a single snapshot of a patient's health during a visit, they get the whole movie. This allows for incredibly precise monitoring of chronic conditions, spotting red flags much earlier, and tweaking treatment plans based on what's actually happening day-to-day.
The IoMT turns health monitoring from an active chore into something that just happens in the background. It becomes a seamless part of life, all while feeding richer, more accurate information back to the care team.
Digital Therapeutics: Software as Medicine
One of the most groundbreaking shifts on the horizon is the rise of digital therapeutics (DTx). Think of these as prescription-strength apps, clinically validated software programs designed to prevent, manage, or treat a specific medical condition.
For instance, a doctor could prescribe a DTx app to help a patient manage their anxiety through guided cognitive behavioural therapy. These aren't just wellness apps; they deliver evidence-based care right to a patient's phone, making treatment more accessible and consistent. DTx is an entirely new class of medicine where the software is the treatment, and it's a key piece of the puzzle in preparing your practice for the future of connected care.
Frequently Asked Questions
Thinking about bringing new patient engagement technology into your practice? You're not alone, and it's normal to have questions. For most clinic leaders I talk to, the big concerns usually circle back to three things: the price tag, whether patients will actually use it, and how it’ll play nice with the software you already have.
Let's cut through the noise and get you some straight answers to these common questions.
How Much Does Patient Engagement Technology Cost?
Honestly, the cost can be all over the map. It's a bit like buying a car, you can get a reliable, basic model or a fully-loaded luxury version. For a smaller practice, a simple patient portal or an automated reminder service might run you anywhere from a few hundred to a couple of thousand dollars a month. On the other end, a large-scale, custom-built platform with deep EHR integration and a branded mobile app is a much bigger investment.
The key is to reframe this from a "cost" to an "investment." You can actually calculate the return on this investment. Think about the concrete savings from fewer hours spent on administrative tasks, a real drop in expensive no-shows, and better patient loyalty that keeps people coming back.
Will My Patients Actually Use This Technology?
This is a big one, but patient adoption boils down to two things: simplicity and value. Is the tool easy to use? Does it solve a real problem for them? If a patient can check their latest lab results online instead of sitting on hold, they'll use it. If the digital way is genuinely more convenient than the old way, people will naturally gravitate towards it.
But you can't just set it and forget it. A successful launch depends on your team actively showing patients the ropes.
Your staff needs to be the biggest cheerleaders for these new tools. When they can confidently walk a patient through the setup and explain the benefits, that excitement is infectious and goes a long way in building trust.
Can This Technology Integrate With My Current EHR?
It absolutely should; this is a deal-breaker. Any patient engagement platform worth its salt must integrate smoothly with your current Electronic Health Record (EHR) system. If it doesn't, you're just creating more work, risking data entry errors, and building frustrating information silos.
Good vendors use well-established industry standards to make sure data flows securely and automatically between the systems. This keeps everything in sync, ensuring patient information is consistent everywhere. Before you sign anything, always get confirmation that the solution has a proven history of working with your specific EHR.
At Cleffex Digital Ltd, we specialise in building secure, user-friendly software that solves real-world problems for healthcare providers. If you're ready to see better patient outcomes and a more efficient clinic, take a look at our custom healthcare software development services.







