The future of healthcare is not about treating sickness anymore; it's about proactively keeping people well. AI-powered healthcare apps are at the very heart of this change, shifting the entire model from reaction to prevention. This is not some far-off concept; it's happening right now, as AI begins to monitor our health in real-time, predict problems before they spiral, and make clinical work far more efficient.
The New Reality of AI in Digital Health
Think about this: what if your health were not just something you discussed at your yearly check-up? What if it were continuously monitored, with potential red flags raised long before you even felt a symptom? This is not a scene from a film; it's the tangible reality we're building today. The discussion around artificial intelligence in healthcare has finally moved past the buzzwords and into real, practical applications that are changing diagnostics and reshaping the patient journey.
This leap forward is powered by two main forces: the massive amount of health data we can now access and the incredible computing power needed to make sense of it all. When you put them together, you get a perfect environment for AI to drive real improvements in both patient outcomes and the day-to-day operations of healthcare.

Unlocking Market Potential
The momentum is hard to ignore, especially here in Canada, which has become a serious global player in health-tech innovation. The Canadian digital health market is expected to hit $13.49 billion in 2024 and is on track to balloon to $53.92 billion by 2030. This incredible growth creates the perfect conditions for AI-driven apps to flourish. We're already seeing this with platforms like PocketHealth, which now helps over two million patients get direct access to their own health records and imaging.
The growth is undeniable. You can get a deeper look into the details of Canada's digital health market and see just how profoundly it's shaping the industry.
This guide is your map for navigating this fast-moving space. We're going to walk through how your organisation can take these big ideas and turn them into real-world solutions, transforming today's challenges into tomorrow's opportunities.
By getting a firm grip on AI's core capabilities and what's driving the market, healthcare organisations can position themselves at the forefront of this new era. This is a future where AI is not just a nice-to-have feature but the very foundation of modern care.
Here’s a breakdown of what we'll cover:
Real-world AI use cases that are gaining traction.
The critical technical and regulatory hurdles you'll need to clear.
How to measure the real impact on both clinicians and patients.
A practical roadmap to get your implementation right.
To set the stage, it's helpful to understand the core technologies that are making all of this possible. These AI capabilities are the building blocks for the next generation of healthcare applications.
Key AI Capabilities Transforming Healthcare Apps
| AI Capability | Primary Function in Healthcare Apps | Example Application |
|---|---|---|
| Machine Learning (ML) | Analyses large datasets to identify patterns and predict outcomes without being explicitly programmed. | Predicting patient readmission risks based on their electronic health records. |
| Natural Language Processing (NLP) | Enables computers to understand, interpret, and generate human language from text and speech. | Transcribing doctor-patient conversations into structured clinical notes automatically. |
| Computer Vision | Trains algorithms to interpret and understand information from digital images and videos. | Assisting radiologists by highlighting potential anomalies in medical scans like X-rays or MRIs. |
| Generative AI | Creates new, original content, from text to images, based on the data it was trained on. | Generating personalised patient education materials or summarising complex medical reports. |
Each of these technologies plays a unique role, but their true power emerges when they work together, creating sophisticated tools that support clinicians and empower patients in new ways.
Emerging AI Use Cases in Modern Healthcare
The conversation around AI in healthcare has officially moved from "what if" to "what's next." We're seeing practical, life-altering applications roll out that do more than just speed up old processes. AI is becoming a genuine partner for clinicians, opening up entirely new ways to diagnose, treat, and manage health.
We're talking about everything from predicting the next flu season to designing a cancer treatment based on someone's unique genetic code. Each new application is driven by the same core goals: to achieve better patient outcomes, ease the incredible burden on medical staff, and make quality healthcare more accessible to everyone.

Predictive Analytics for Population Health
One of the biggest game-changers is the shift from reactive to proactive care. Instead of just responding to crises, AI algorithms can sift through massive public health datasets, think about environmental data, social media chatter, and hospital admission rates, to forecast disease outbreaks with startling accuracy. This gives public health officials a crucial head start to allocate resources, launch targeted prevention campaigns, and stop a potential crisis in its tracks.
It’s like having an advanced weather forecast, but for illnesses like COVID-19 or influenza. By pinpointing hotspots and predicting how a virus might spread, health systems can get staff and supplies ready, ultimately saving lives and building a far more resilient healthcare infrastructure.
The market certainly reflects this potential. Canada's AI healthcare sector, valued at $1.1 billion in 2023, is expected to explode to $10.8 billion by 2030. But there's a catch: only 21% of Canadian doctors feel confident about AI's handling of patient confidentiality, according to research on AI project statistics in Canadian healthcare from launchable.ai. This trust gap is a major hurdle we need to clear.
AI-Powered Medical Imaging and Diagnostics
In the world of diagnostics, AI is quickly becoming the most reliable second opinion a radiologist could ask for. Computer vision algorithms, trained on millions of medical images, can spot subtle patterns in X-rays, CT scans, and MRIs that the human eye might overlook. This does not replace the expert; it supercharges their ability to make faster, more accurate diagnoses.
Think of it as a specialist consultant who has seen every similar case in history, all at once. The AI can flag a tiny anomaly on a scan, help prioritise the most urgent cases, and significantly cut down on diagnostic errors that can have devastating consequences.
By handling the initial review of countless images, AI gives highly skilled radiologists their time back. They can then focus their expertise on the most complex and nuanced cases, which directly fights burnout and elevates the quality of patient care.
This powerful combination of human experience and machine precision is reshaping modern diagnostics. It’s a fascinating field, and you can dive deeper into the technical side in our guide to AI for medical imaging and diagnostics.
Hyper-Personalised Treatment Plans
The days of one-size-fits-all medicine are numbered. AI is ushering in an era of hyper-personalisation, where it can analyse a patient's genetic makeup, lifestyle, and medical history to develop a treatment plan that is truly theirs and theirs alone.
This is having a massive impact in areas like oncology. AI models can now predict how a specific tumour might respond to different chemotherapies or immunotherapies. By matching the right treatment to the right person, clinicians can boost success rates and drastically reduce harmful side effects. The advantages are clear:
Increased Treatment Efficacy: Pinpointing the most effective drug or therapy right from the start.
Reduced Adverse Reactions: Steering clear of treatments likely to cause problems for a specific patient.
Optimised Dosing: Fine-tuning the exact dosage for maximum impact with minimal risk.
This is not just an improvement; it's a fundamental change, moving medicine from a practice of averages to a science of individuals.
Intelligent Virtual Health Assistants
Finally, let's not forget the patient's daily experience. AI-driven virtual assistants are completely changing how people engage with their own health. These are not your average chatbots; they are sophisticated tools available 24/7 to answer questions, send medication reminders, and help manage chronic conditions right from a patient's home.
Using advanced Natural Language Processing (NLP), these assistants can understand context, offer empathetic responses, and deliver clear health information. For clinics and hospitals, this means fewer routine phone calls, better patient adherence, and a new way to monitor patients remotely. It all adds up to a more connected and efficient healthcare experience for everyone involved.
Navigating Technical and Regulatory Hurdles
Taking a great idea for an AI healthcare app and turning it into a real-world tool is about much more than just clever code. It's about successfully navigating a maze of technical and regulatory demands. For anyone stepping into this space, getting a handle on these challenges is the first, most critical step towards building something that’s not just effective, but also secure, compliant, and trustworthy.
You really have to get both sides of this equation right. The technology itself needs to be rock-solid, reliable, and built on a foundation of excellent data. At the same time, it has to meet strict regulations designed to protect patient safety and privacy, especially here in Canada.
The Technical Foundations of Trustworthy AI
Before any AI algorithm can even think about making a prediction, it needs a solid technical framework. This really comes down to three things: the quality of your data, how well your systems talk to each other, and how rigorously you train your models. Nail these, and you're on the right track.
It all starts with high-quality data. Think of an AI model like a medical student. Its performance is a direct reflection of the textbooks and case studies it learns from. If that training data is biased, incomplete, or just plain wrong, the AI's "diagnoses" will be flawed, and that can have serious consequences. Sourcing clean, diverse, and representative datasets is probably the single most important technical step you'll take.
Next up is interoperability, a fancy word for making sure different digital systems can actually communicate. Imagine a family doctor's notes from Toronto being instantly and perfectly understood by a specialist's system in Vancouver. That’s the dream, and it's what standards like FHIR (Fast Healthcare Interoperability Resources) are designed to do. They ensure data flows smoothly and securely between different apps and electronic health records.
Without strong interoperability, even the most advanced AI app becomes a silo, unable to access the comprehensive data it needs to function effectively. This makes adherence to standards like FHIR essential for building a connected healthcare ecosystem.
Finally, the training and validation process for the model has to be painstaking. This is not just about showing the AI how to spot patterns. It's about constantly testing it against new, unseen data to prove its predictions are accurate and reliable when it matters most, in a real clinical setting.
The Canadian Regulatory Maze
Beyond the technical hurdles, the regulatory environment is its own beast. In Canada, healthcare is a tightly controlled field. Any AI app that's classified as a medical device falls under the watchful eye of Health Canada. Whether your app fits that description depends on what it's meant to do and the level of risk it poses to patients.
On top of that, every AI healthcare app must follow strict data privacy laws. The federal Personal Information Protection and Electronic Documents Act (PIPEDA) sets the rules for how private-sector organisations collect, use, and share personal information. For anyone handling patient data, this means treating every single piece of information with the highest level of security and transparency.
Figuring all this out is not simple. Successfully navigating the complex regulatory landscape for AI healthcare apps requires a deep understanding of AI security and compliance in medical technology and healthcare. It's an area where a misstep can lead to serious legal and financial trouble.
For a deeper dive into the specifics, check out our guide on AI in healthcare and data privacy in Canada, where we break down what developers and healthcare organisations need to know.
Ultimately, getting these technical and regulatory details right is what will determine the future of AI healthcare apps. It really highlights why it’s so important to work with a development partner who not only gets the tech but also has the experience to build solutions that are secure, compliant, and truly ready for the demands of the industry. This dual focus is what ensures innovation can actually do what it’s supposed to: improve patient care, safely and effectively.
Measuring the Real-World Impact on Providers and Patients
Investing in new technology is one thing, but how does that investment actually translate into genuine, measurable value for your clinic or hospital? When it comes to the future of AI healthcare apps, the real test is whether they deliver tangible benefits, not just for the bottom line, but for the clinicians on the front lines and the patients they serve. This is not about adding fancy features; it's about solving core challenges.
For healthcare providers, the impact really splits into two key areas. On the clinical side, we're seeing AI tools make a real difference in diagnostic accuracy, helping doctors create treatment plans that are genuinely personalised. Then, on the business side of things, the gains are just as compelling, from sorting out back-office headaches to making patients feel more supported and likely to stick with your practice.
Enhancing Clinical Precision and Outcomes
One of the most powerful ways AI helps in a clinical setting is by acting as an expert assistant, which naturally reduces the chance of human error. Think about it: AI-powered diagnostic tools can scan medical images or lab results, flagging tiny abnormalities that a busy doctor might miss at the end of a long shift. This kind of support leads to faster, more accurate diagnoses, and that directly improves patient outcomes.
Beyond that, AI is unlocking a level of personalised care that was simply impossible to deliver at scale before. By analysing a patient's entire health profile, everything from their genetics to their lifestyle, algorithms can help clinicians predict which treatments are most likely to work. We're moving away from a one-size-fits-all model towards a much more precise, individualised approach that boosts effectiveness and minimises side effects.
The ultimate goal here is to augment, not replace, the expertise of healthcare professionals. AI is brilliant at handling the heavy lifting of data analysis, which frees up clinicians to focus on complex decision-making, patient communication, and the empathetic side of care that a machine simply can't replicate.
This support system is absolutely vital in high-pressure environments, helping to reduce staff burnout by taking on some of the more repetitive analytical work.
Driving Operational and Financial Health
Once you step outside the examination room, AI becomes a powerful engine for making the whole operation run more smoothly. So many administrative tasks, from patient scheduling and billing to managing electronic health records, are perfect for automation. AI-driven apps can manage these workflows intelligently, taking a huge administrative weight off your staff's shoulders.
These efficiencies add up to some serious cost reductions. One study found that AI applications could lead to annual savings of £120 billion for the UK's health and social care system if they were widely adopted. When you automate routine processes, you do not just cut costs; you also minimise errors and free up your team to focus on more patient-facing roles. This creates a much better patient experience, which in turn improves engagement and retention rates, a critical metric for any healthcare organisation.
A Comparative Look at AI Adoption
The benefits of AI are not one-size-fits-all; they show up differently depending on the size and needs of the organisation. A small local clinic has very different challenges from a large hospital network, but AI offers smart solutions for both. Understanding these differences is the key to making a strategic investment that pays off.
To illustrate this, the table below provides a comparative look at how AI healthcare apps benefit different segments of the healthcare industry.
AI Impact Analysis for Healthcare Organisations
| Benefit Area | Impact on Small Clinics (<£5M) | Impact on Medium Enterprises (£5M–£500M) |
|---|---|---|
| Operational Efficiency | Automated appointment scheduling and billing reduce the need for dedicated admin staff, freeing up clinicians' time. | Intelligent workflow automation optimises bed management, staff rostering, and supply chain logistics for significant cost savings. |
| Clinical Support | AI-powered diagnostic aids provide a "second opinion" for general practitioners, improving diagnostic confidence without needing in-house specialists. | Advanced AI imaging analysis across departments (e.g., radiology, pathology) helps prioritise urgent cases and standardises diagnostic quality. |
| Patient Engagement | AI chatbots handle routine patient queries 24/7 and send automated reminders, improving communication and adherence to care plans. | Personalised patient portals with AI-driven health insights and remote monitoring improve chronic disease management and reduce readmissions. |
| Cost Reduction | Lower overheads from automated administrative tasks and optimised resource use lead to better financial stability and growth potential. | Predictive analytics for resource allocation and reduced length of stay through better care coordination deliver substantial financial returns. |
As you can see, the future of AI healthcare apps is not just for the big players. By homing in on specific operational and clinical pain points, organisations of any size can find AI-powered solutions that deliver a clear, measurable, and meaningful return on their investment.
A Practical Roadmap for AI Implementation
Bringing artificial intelligence into a healthcare setting can feel like a massive undertaking. But with a structured, step-by-step approach, what seems like a complex challenge becomes a series of manageable goals. The secret for any healthcare organisation is to move with purpose, starting with a clear problem you need to solve and building out from there. This way, you ensure the final solution actually addresses a real-world need and delivers tangible value.
The most important first step has nothing to do with technology. It's all about the problem. I've seen too many organisations get swept up in the hype and adopt AI just for the sake of it. A successful project always starts by identifying a genuine pain point in your daily operations. Are your staff buried under administrative tasks? Are diagnostic wait times too long? Or is patient follow-up falling through the cracks? Pinpointing a specific, well-defined problem is the bedrock of any solid implementation.
Charting Your Course to AI Integration
Once you know exactly what you're trying to fix, the journey can be broken down into clear, logical stages. For leaders looking to develop AI-powered healthcare apps, following a practical AI implementation roadmap is a great way to guide strategic planning and execution. It ensures each phase builds on the one before it.
This kind of structured process helps take the risk out of the project, giving you room to make adjustments and learn as you go. The main stages usually look something like this:
Assess Your Data Readiness: AI runs on data. Simple as that. You have to take a hard look at the quality, quantity, and accessibility of your existing data. Is it clean, structured, and compliant with privacy laws? A thorough data audit will show you where the gaps are, and you'll need to fix those before you can even think about building a model.
Decide on a 'Build vs. Buy' Strategy: You don’t always have to reinvent the wheel. Your organisation will come to a fork in the road: do you build a custom AI solution from the ground up, buy an off-the-shelf product, or partner with a firm that specialises in this? The right choice really depends on your budget, timeline, in-house skills, and just how unique your problem is.
Launch a Small-Scale Pilot Project: Before you go all-in, run a pilot. This is your chance to test the AI solution in a controlled environment, get real feedback from users, and prove its value without a huge upfront investment. A successful pilot creates momentum and gives you the hard data needed to justify a full-scale rollout.
Placing People at the Centre of Technology
A classic mistake when developing new tech is forgetting about the people who have to use it every day. The most brilliant AI tool is a failure if it's clunky or confusing for clinicians and patients. That's why a user-centred design approach is not just a nice-to-have, it's absolutely essential for getting people on board.
The goal is to create a solution that integrates seamlessly into existing clinical workflows, not one that disrupts them. By involving doctors, nurses, and patients in the design process, you ensure the final product is intuitive, helpful, and genuinely improves their experience.
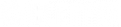
This infographic gives a great visual of how a well-thought-out AI strategy flows from technical improvements to real, human-centric benefits.
You can see the clear progression: reducing errors is the first domino to fall. That, in turn, allows for more personalised care, which ultimately leads to major cost savings down the line.
This whole journey, from spotting the initial problem to the final launch, is undeniably complex. Working with a skilled development partner can be the difference between a project that stalls and one that succeeds. A good partner brings more than just technical skill; they offer strategic guidance that can turn the intimidating task of AI implementation into a smooth and successful project. To learn more about this process, explore our complete guide to healthcare app development.
So, What’s Next on Your AI Journey?
We've covered a lot of ground, and it’s clear that AI in healthcare is not some far-off concept; it’s happening right now. The opportunity to sharpen diagnostics, tailor patient treatments, and make daily operations run smoother is here. But getting from knowing this to doing something about it requires a bit of strategic thinking. You need a clear-eyed view of where your organisation stands and what the most logical next step is.
It’s time to shift from watching on the sidelines to taking action. Whether you're running a small local clinic or leading a mid-sized healthcare enterprise, the moves you make today will shape your future. The trick is to start small and smart, with a focused goal that solves a real-world problem you're facing.
Finding Your Starting Line
To make this tangible, let's figure out which of these descriptions fits you best. Each one points to a practical, actionable step you can take, based on your organisation's size and readiness.
For the Small Clinic Owner: Your best bet is to start with a single, high-impact tool. Think about your biggest administrative headache. Is it patient scheduling? Or maybe billing? Find an AI-powered solution for that one thing. It's a low-risk way to test the waters and see an immediate benefit.
For the Medium Enterprise Leader: You're in a position to think bigger. It's time to build a proper automation strategy. Start with an internal audit to pinpoint two or three key workflows, either clinical or operational, that are ripe for an AI upgrade. Areas like patient data analysis or managing staff resources are often great places to find major efficiency gains.
The real secret is to stop thinking of AI as a one-off project. Instead, see it as a fundamental part of your long-term growth. That mindset is what will give you a lasting edge and ultimately lead to better patient care.
No matter where you begin, the most important thing is simply to begin. The lessons you learn from a small pilot project or a strategic audit will become the bedrock for your more ambitious AI initiatives down the road.
Ready to figure out what that first or next step looks like? Our team at Cleffex is here to help you cut through the noise. Let’s talk about your goals and map out a practical plan to put AI to work for you.
Frequently Asked Questions
Stepping into the world of AI in healthcare naturally brings up a lot of questions, especially for organisations trying to figure out where to start. We’ve gathered some of the most common ones we hear to give you clear, straightforward answers as you think about your next move.
How Can Smaller Clinics Afford AI Solutions?
The idea of custom AI development can definitely feel intimidating, but the good news is you do not need a massive budget to get started. Many of the best tools are now available as Software-as-a-Service (SaaS), which flips the model from a huge upfront investment to a predictable monthly fee.
A smart way to begin is by picking one specific problem and finding an AI tool that solves it well. Think automated appointment scheduling or smarter billing software. This way, you can see a clear return on investment right away before deciding to scale up to more complex systems.
What’s the Biggest Hurdle to AI Adoption in Healthcare?
Interestingly, the biggest roadblock is not the technology. It’s a mix of data security concerns, navigating the maze of regulations, and, most importantly, earning the trust of the clinicians who will use these tools every day. Healthcare data is incredibly sensitive, so rock-solid privacy and security are not optional. Getting regulations like PIPEDA right also requires expertise that many do not have in-house.
Beyond that, doctors and nurses need to feel confident that an AI tool is reliable and genuinely helpful, not just another piece of tech that gets in the way. Real adoption happens when systems are easy to use, fit neatly into existing workflows, and prove they can make a positive difference in real-world care.
The core challenge really boils down to building trust. AI needs to be seen as a dependable co-pilot that supports healthcare professionals, enhancing their skills rather than trying to replace their judgment.
Will AI Replace Doctors and Nurses?
Absolutely not. The real goal here is augmentation, not replacement. AI is fantastic at churning through massive amounts of data, finding subtle patterns, and taking over repetitive administrative tasks that drain clinicians' time.
This frees up doctors, nurses, and other specialists to focus on what they do best: making complex decisions, connecting with patients, and delivering the kind of empathetic care a machine simply can't. Think of AI as a powerful assistant that makes your team better, leading to less burnout, more efficiency, and ultimately, better outcomes for patients. It's all about creating a stronger partnership between human expertise and smart technology.
Ready to explore how AI can solve your specific challenges and open up new possibilities? The team at Cleffex is here to guide you through it. Contact us today to map out a practical plan that puts AI to work for your organisation.