Imagine having a consultant by your side who has reviewed millions of patient charts, spotting patterns no human could ever detect. That's the essence of AI-powered healthcare solutions. They act as a powerful assistant for clinicians, not a replacement, by analysing massive datasets to sharpen diagnostics, personalise treatments, and make operations run more smoothly.
The New Era of AI-Powered Healthcare
Artificial intelligence is quickly shifting from a buzzword to a practical tool in the modern medical toolkit. It’s less about futuristic robots and more about a smart layer of software that enhances human expertise. At its heart, AI processes volumes of health data far beyond human capacity, uncovering insights that lead to better, faster, and more efficient patient care.
This isn't just a minor tech upgrade; it's a fundamental change in how we deliver healthcare. We're moving away from a one-size-fits-all approach and towards a model that's more predictive and precisely tailored to each individual. The real power here is that these tools tackle both clinical and operational hurdles, becoming a key part of daily workflows that help manage resources and give medical professionals data-driven support.

Why This Matters for Healthcare Providers
For any hospital or clinic, bringing AI into the fold is about more than just staying current. It’s a direct response to real-world pressures like rising operational costs, heavy administrative loads, and the constant drive to improve patient outcomes.
By automating repetitive tasks and offering deeper analytical power, AI frees up clinicians to do what they do best: focus on their patients and make complex decisions. As we move forward, the integration of new tools like AI-driven diagnostics in physical therapy is setting a new standard for patient care and operational excellence.
The goal is never to replace the human touch in medicine, but to amplify it. AI handles the data so doctors and nurses can dedicate more of their energy to the patient.
This guide cuts through the noise to give you a clear, business-focused look at how AI is actively changing medicine. We’ll lay the groundwork for understanding how to implement these tools and measure their impact, always focusing on tangible results. For a deeper dive, check out our article on the benefits of AI in the healthcare industry.
Core Promises of AI in a Medical Context
While the applications are incredibly diverse, they tend to deliver value in a few key areas that make a real difference for both patients and providers.
Improved Diagnostic Accuracy: AI algorithms can review medical images like X-rays and MRIs with incredible precision, often catching subtle signs of disease that the human eye might overlook.
Personalised Treatment Pathways: By looking at a patient's genetics, lifestyle, and medical history all at once, AI helps clinicians craft highly customised treatment plans with a better chance of success.
Streamlined Hospital Operations: From optimising patient scheduling and managing bed availability to automating billing, AI helps healthcare facilities operate more efficiently and reduce costs.
In the end, all these systems are designed to work together, building a smarter and more connected healthcare ecosystem for everyone.
Understanding the Core AI Technologies in Medicine
To really get a handle on AI-powered healthcare solutions, you have to look under the bonnet and see what makes them run. These technologies aren't just abstract ideas; they are practical tools built to solve real-world problems in hospitals and clinics. Knowing how they work is the first step to using them effectively.
The foundation of most modern AI is Machine Learning (ML). The best way to think of it is like a junior doctor learning on the job. We feed an ML model thousands of anonymised patient cases, each with its own data and a known outcome. Over time, it starts to spot incredibly complex patterns that help it predict what might happen next, allowing it to forecast disease risk or suggest treatment options with growing confidence.
Then there's Natural Language Processing (NLP). So much of healthcare is built on text, from clinicians' notes and patient records to dense research papers. NLP acts like a super-efficient medical scribe that can read and make sense of all this human language. It can pull out key details like symptoms or medication dosages from a doctor's free-form notes and turn them into structured data that a computer can actually analyse.

Making Sense of Medical Images with Computer Vision
Perhaps the most striking application of AI in medicine is Computer Vision. This field trains algorithms to interpret visual information, much like our own eyes and brain do. In medicine, this has massive implications, especially for specialists in radiology and pathology.
A computer vision model can be trained on millions of medical images: X-rays, CT scans, MRIs, you name it. In doing so, it learns to recognise the subtle textures, shapes, and anomalies that might point to a health problem. It essentially becomes a radiologist's second set of eyes, tirelessly highlighting areas of concern that might be too faint or small for a person to notice right away. The goal isn't replacement; it's augmentation. It’s about making sure nothing gets missed.
You can dive deeper into this in our guide on AI for medical imaging and diagnostics. This technology helps speed up diagnoses, lower error rates, and get urgent cases in front of an expert faster, which can make all the difference for a patient.
To see how these technologies translate into practice, this table breaks down their core functions and gives a concrete example for each.
Key AI Technologies and Their Healthcare Applications
| AI Technology | Core Function | Primary Healthcare Application Example |
|---|---|---|
| Machine Learning (ML) | Learns from data to identify patterns and make predictions without being explicitly programmed. | Predicting which patients are at high risk for hospital readmission based on their health records and demographic data. |
| Natural Language Processing (NLP) | Enables computers to understand, interpret, and generate human language from text and speech. | Automatically extracting patient symptoms, medications, and diagnoses from unstructured clinical notes in an EHR. |
| Computer Vision | Trains computers to interpret and understand information from digital images and videos. | Identifying and highlighting potential cancerous nodules on a chest CT scan to assist a radiologist's review. |
Each of these technologies is powerful on its own, but the real breakthroughs happen when they're combined.
How These Technologies Work Together
In practice, these core AI tools rarely work in isolation. The most sophisticated AI-powered healthcare solutions emerge when they are woven together to build a comprehensive view of a patient's health.
Consider a modern diagnostic platform. It might use:
NLP to pull relevant symptoms and family history from a patient's electronic health record.
Computer Vision to analyse a recent MRI for any potential abnormalities.
Machine Learning to bring all that textual and visual data together, comparing it against a massive database to calculate the probability of a specific condition.
This integrated approach mirrors how a human clinician thinks, but it operates at a scale and speed that's simply impossible to achieve manually.
By integrating different AI capabilities, healthcare systems can move from reacting to health events to proactively predicting them. This shift is fundamental to improving patient outcomes and managing population health more effectively.
At the end of the day, these tools are all designed to do one thing: turn incredibly complex data into clear, actionable insights. Whether it's making sense of language, interpreting an image, or predicting an outcome, each technology exists to give healthcare professionals the information they need to provide the best possible care.
Putting AI to Work in Clinical and Operational Settings
The real test of any new technology is how it performs on the ground. For AI-powered healthcare solutions, this means moving beyond the buzz and delivering tangible benefits that clinicians and administrators can see and feel every day. These tools aren't some far-off concept; they’re actively reshaping how hospitals and clinics work, solving stubborn problems in both patient care and back-office operations.
On one side, you have AI augmenting clinical decisions with insights that were previously out of reach. On the other hand, it’s chipping away at the mountain of administrative work that often slows the entire system down, freeing up people to focus on what matters most.
The pace of adoption is picking up quickly. Recent data shows a sharp increase in the use of AI tools among both physicians and health plans. The American Medical Association found that roughly two-thirds of doctors (about 66%) are now using health AI – a 78% jump from previous years. This surge has even prompted large purchasers like CalPERS to start cataloguing the AI tools being used across their health plans. You can dig into the specifics in the full report on AI adoption in healthcare.
Enhancing Clinical Precision and Outcomes
In the consulting room and the operating theatre, AI is becoming an indispensable partner for diagnosis and treatment planning. It’s making a direct, positive impact on patient outcomes simply by being able to analyse complex data at a scale humans can't.
Medical imaging is a perfect example. AI algorithms, especially those built on computer vision, can review radiological scans like MRIs and CTs with incredible accuracy. They’re trained to spot the tiniest, earliest signs of conditions like cancer or neurological disorders – anomalies that a radiologist might miss at the end of a long shift. The AI doesn’t replace the expert; it acts as a tireless second set of eyes, ensuring nothing critical gets overlooked.
But it’s not just about diagnostics. AI is also making patient care far more personal.
Predictive Analytics in ICUs: In intensive care, machine learning models can track a patient's vitals in real-time to predict a sudden decline hours before it happens. This gives the care team a crucial head start to intervene and prevent serious complications.
Personalised Treatment Plans: For complex diseases like cancer, AI can sift through a patient's genetic profile and clinical history to suggest the most effective therapies. It’s a shift away from one-size-fits-all protocols towards precision medicine truly built for the individual.
The real clinical value of AI isn't about letting a machine take over. It’s about giving clinicians a more complete, data-backed picture of their patient. The technology connects dots that were previously invisible, empowering providers to make better, more confident decisions when it counts.
Optimising Healthcare Operations
While the clinical applications get most of the attention, the impact of AI-powered healthcare solutions on the operational side is just as profound. AI is ironing out long-standing inefficiencies, helping healthcare organisations run more smoothly and become more financially stable.
Take the headache of administrative tasks. Things like prior authorisation, which used to burn hours of staff time on paperwork and phone calls, can now be handled by intelligent automation. These systems can gather the necessary documents and submit requests automatically, cutting down delays and letting staff focus on patients instead of fax machines.
This drive for efficiency is also changing how patients and resources move through the entire facility.
Streamlining Workflows and Financial Health
Making a hospital run well is key to its survival. AI provides the tools to manage everything from bed availability to operating theatre schedules with far more intelligence.
Patient flow optimisation is a great example. By analysing historical admission data and real-time information, predictive models can forecast when the accident and emergency department will be busiest. This allows hospitals to staff up accordingly, manage bed assignments proactively, and cut down on those frustrating wait times for patients.
At the same time, AI is also shoring up the financial health of these organisations through better Revenue Cycle Management (RCM). AI-powered platforms can automate medical coding and billing, catching errors and reducing the number of denied claims. By using Natural Language Processing (NLP) to read clinical notes, these systems assign the right codes from the start. This not only gets payments processed faster but also secures the financial footing needed to keep delivering excellent care.
Navigating the Challenges of AI Implementation
Getting an AI-powered healthcare solution up and running is about much more than just installing new software. It’s a major strategic shift that demands careful planning around data integration, regulatory compliance, and airtight security. If you don't get these pieces right from the start, even the most promising AI tool can fail to deliver, or worse, create significant risk.
Getting AI to Talk to Your Existing Systems
One of the first and most significant hurdles is making a new AI platform work with your existing Electronic Health Record (EHR) system. These systems are the heart of any healthcare organisation, holding all the critical patient data. The new AI tool has to be able to pull data from and push insights back to the EHR seamlessly.
This is all about achieving true interoperability. The goal is a smooth, two-way flow of information that prevents data from getting trapped in separate systems. When done right, clinicians get a complete, unified view of their patients, and the AI’s insights appear directly within the workflows they already know. It feels like a natural extension of their tools, not another screen to check.
This diagram shows the general workflow for how AI turns raw data into useful insights for both clinical and operational teams.
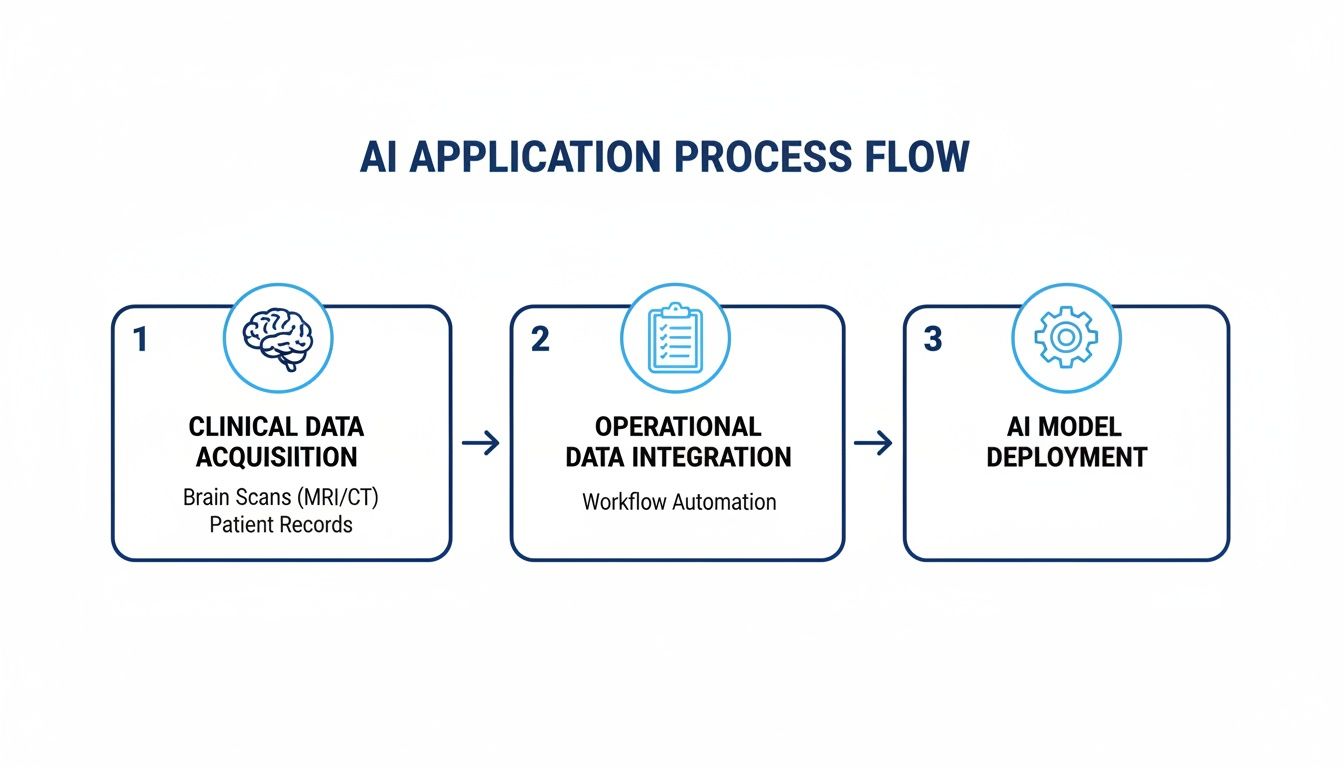
As you can see, it all starts with good data. From there, the AI models analyse it and deliver actionable information that can improve patient care and make operations more efficient.
Mastering the Regulatory and Compliance Maze
Once you solve the technical puzzle, you face a complex web of regulations designed to protect sensitive patient information. For any healthcare organisation adopting AI, navigating this landscape is simply non-negotiable.
And it’s not just about national laws. In Canada, for example, each province has its own specific health information legislation on top of the federal PIPEDA. This means a one-size-fits-all approach to compliance just won’t cut it. You have to be on top of the rules at every level.
A significant hurdle in deploying AI, particularly in healthcare, is ensuring full compliance with data protection regulations such as GDPR. For a more detailed look, consult a comprehensive practical AI GDPR compliance guide.
Staying vigilant isn't just about avoiding hefty fines; it’s about earning and keeping patient trust. When people are confident their data is being handled responsibly, they are far more likely to embrace the new technologies you're introducing.
Fortifying Cybersecurity for Sensitive Health Data
Health data is incredibly valuable, which, unfortunately, makes it a prime target for cyberattacks. As AI becomes more deeply embedded in hospital operations, it can introduce new security vulnerabilities that need to be managed from day one. This requires a proactive, multi-layered cybersecurity strategy.
At a minimum, best practices for securing AI-powered healthcare solutions should include:
End-to-End Encryption: Data must be encrypted whether it's sitting on a server (at rest) or moving between systems (in transit). No exceptions.
Strict Access Controls: Role-based access is key. People should only be able to see the specific data they need to do their jobs, which drastically reduces the risk of exposure.
Regular Security Audits: You have to proactively look for weaknesses. Penetration testing and vulnerability assessments help you find and fix security gaps before criminals can exploit them.
A deep understanding of regional data privacy laws is also essential. For organisations operating in Canada, this means adhering to a specific set of regulations governing patient information. We cover this topic in more detail in our guide on AI in healthcare and data privacy in Canada.
Ultimately, strong security isn't a one-and-done project. It’s an ongoing commitment that involves constant monitoring, regular staff training, and a clear plan for what to do if a breach occurs. By building security into every step of your AI implementation, you protect your patients, your data, and your organisation's reputation.
How to Choose the Right AI Partner and Measure Success
Picking an AI-powered healthcare solution isn’t just about buying a piece of software; it’s about starting a long-term strategic relationship. The right partner can help you hit your targets faster, but the wrong one can burn through your budget and leave you with nothing but stalled projects. You have to be tough in your evaluation, looking past the polished demos to see what really makes a solution tick.
Start by asking the hard questions. Does the vendor have any peer-reviewed clinical studies that actually back up their claims? What about their security credentials – can they prove they follow regional privacy laws like Canada's PIPEDA to the letter? A vendor's answers here will tell you everything you need to know about how seriously they take both results and patient safety.
Vetting Potential AI Vendors: A Practical Checklist
To make the right call, you need to look at everything: technical performance, clinical proof, and the support they offer. Think of it as a comprehensive inspection to make sure the solution isn't just powerful on paper, but also practical and secure enough to work in the real world of healthcare.
Before you even think about signing a contract, make sure your team has dug into these key areas:
Clinical Validation and Evidence: Forget the marketing brochures. Ask for published, peer-reviewed research that proves the tool works accurately in a clinical setting that looks a lot like yours.
Security and Compliance Certifications: The vendor needs to show you clear proof of their compliance with all relevant healthcare regulations. This means providing certifications and third-party audit reports that confirm their data protection is up to snuff.
Integration Capabilities and Support: A fantastic AI tool is worthless if it can't talk to your existing EHR. Make sure the vendor has a solid history of successful integrations and offers real, hands-on technical support during and after the rollout.
Post-Implementation Partnership: What happens after you go live? A good partner sticks around. They should offer ongoing support, proper training for your staff, and have a clear plan for future updates and improvements.
Choosing a vendor is a long-term commitment. Look for partners who are honest about their technology's limitations and are genuinely interested in working with you to achieve real, measurable improvements for your clinic and your patients.
Defining and Measuring Your Return on Investment
Once you’ve found your partner, it’s time to prove the investment was worth it. Success isn’t about how fancy the algorithm is; it’s about the real, tangible impact it has on your organisation. That means setting clear Key Performance Indicators (KPIs) that tie directly back to your biggest goals. Ditch the vanity metrics and focus on outcomes that actually matter to your clinicians, administrators, and patients.
The trick is to get a solid baseline before you flip the switch. If you don't know where you started, you'll never be able to prove how far you've come.
Key KPIs for AI in Healthcare
To get a true sense of the impact your AI-powered healthcare solutions are having, concentrate on metrics that show improvements in care quality, operational flow, and your bottom line.
Clinical Outcome Metrics: These are the big ones. Track changes in diagnostic error rates, see if you can reduce the time it takes to start treatment for critical conditions, and monitor for a drop in hospital readmission rates.
Operational Efficiency Metrics: How is the AI making your daily workflows smoother? Look for better patient throughput, less time spent by staff on administrative tasks, and more efficient operating theatre scheduling.
Financial Impact Metrics: You need to see a clear return. This often shows up as lower administrative costs, fewer denied insurance claims, and a more efficient revenue cycle overall.
Patient and Staff Satisfaction Scores: Technology should make people's lives easier, not more complicated. Keep a close eye on patient satisfaction surveys and check in regularly with your clinical staff to see how they feel about using the new tools.
By zeroing in on these concrete metrics, you can move past just saying the AI works and build a solid business case that shows everyone, from the boardroom to the break room, the real value it's delivering.
Frequently Asked Questions About AI in Healthcare
When organisations start looking into AI-powered healthcare solutions, it's natural for a lot of practical questions to pop up. Let's walk through some of the most common ones to clear up how this technology actually works in the real world.
Will AI Replace Doctors and Other Healthcare Professionals?
Absolutely not. Think of AI in a clinical setting as a powerful assistant, not a replacement. Its main job is to augment the incredible skills of healthcare professionals.
These systems are brilliant at sifting through massive amounts of data, catching subtle patterns humans might miss, and handling the repetitive admin work that bogs everyone down. This frees up doctors, nurses, and specialists to focus on what truly matters: making complex clinical judgements, connecting with patients, and delivering compassionate, human-centred care. It's less of a takeover and more of a collaboration – like a co-pilot supporting the pilot.
How Is Patient Data Kept Secure With AI Solutions?
Protecting patient data isn't just a feature; it's the absolute foundation of any trustworthy AI solution. Security is designed in from the very beginning, with strict compliance to regulations like Canada's Personal Information Protection and Electronic Documents Act (PIPEDA) or GDPR in Europe.
Here are a few core security measures that are non-negotiable:
Data Encryption: All patient information is encrypted, both when it's being stored (at rest) and when it's being moved between systems (in transit).
Anonymisation: Wherever possible, personally identifiable information is stripped out or masked to ensure patient privacy is the top priority.
Access Controls: Rigid, role-based access rules mean that people can only see the specific data they absolutely need to do their job – nothing more.
On top of that, regular security audits and penetration testing are standard practice to stay ahead of cyber threats and safeguard patient confidentiality.
What Is the Best First Step for Adopting AI?
The smartest way to start is by picking one specific, high-impact problem you want to solve. Instead of adopting AI just for the sake of it, find a genuine pain point in your operations. Maybe it’s frustrating diagnostic delays, a chaotic patient scheduling system, or stubbornly high readmission rates.
Start with a focused pilot project that has clear, measurable goals. This approach lets you prove the value of the technology quickly, get your key stakeholders on board, and learn valuable lessons before you commit to a larger rollout. It also aligns with what the public expects; recent research shows people are open to AI in healthcare, but they insist on transparency and human oversight. You can learn more about public opinions on AI in healthcare.
At Cleffex Digital Ltd, we focus on building secure, compliant, and genuinely effective AI-powered healthcare solutions that address your specific challenges. We have deep expertise in navigating the complexities of data privacy and system integration, making sure your AI initiative is a success right from the start.
Partner with us to build your next-generation healthcare solution







