What was once a distant idea is now our daily reality; the future of digital healthcare in Canada is here. The shift is being driven by a perfect storm of new patient expectations, incredible leaps in technology, and hard-won lessons from recent global health crises. At its core, this change is all about making healthcare more accessible and putting the patient first, using everything from virtual care to artificial intelligence.
The New Era of Canadian Digital Healthcare

Canada's healthcare system is in the middle of a massive overhaul. The old model of relying almost exclusively on in-person visits and stacks of paper records is giving way to a smarter, digital-first approach. This isn't just about adding a few new tools for convenience; it’s a fundamental rethinking of the relationship between patients and their care providers.
To really get a handle on this evolution, we need to look at three key pillars. Each one brings its own set of opportunities and, of course, a few challenges for everyone involved: patients, clinicians, and policymakers alike.
The Rise of Virtual Care: Telehealth is no longer a niche service. It's quickly becoming a standard way to deliver care, knocking down geographical barriers and making it easier for people in remote communities to get the help they need.
The Challenge of Connected Health Data: Getting patient information to flow seamlessly between different clinics, hospitals, and specialists is the holy grail of coordinated care. It’s a complex puzzle, but one we absolutely have to solve.
The Impact of Artificial Intelligence: AI is starting to play a fascinating role in supporting clinical decisions. It's helping to analyse medical scans with incredible accuracy and even predict health trends, paving the way for more proactive and personalised medicine.
Why This Matters Now
The push for digital health has some serious momentum behind it. The pandemic forced our hand, rapidly accelerating the adoption of virtual consultations and proving they could work on a national scale. At the same time, Canadians have got used to managing their banking, shopping, and social lives online; they now have the same expectation of accessibility from healthcare.
The market growth tells a similar story. The digital health market in Canada is on track to hit US$3.69 billion in revenue by 2025, and it’s expected to keep growing at a healthy 6.44% each year through 2030. This isn't happening in a vacuum; it's supported by near-universal smartphone use, better internet across the country, and government initiatives aimed at dragging our healthcare system into the 21st century.
The integration of digital health is essential for preparing a workforce capable of using new technologies to enhance care delivery and patient outcomes. It addresses the need for greater efficiency, improved accessibility, and a more sustainable healthcare system for all Canadians.
The Path Forward
Making sense of this new landscape means looking beyond the tech itself to the entire ecosystem that supports it. Innovation is happening everywhere, from large-scale provincial platforms to niche applications, like the recent expansion of digital brain health initiatives across Canada. As we forge ahead, the goal isn't just to build a system that's technologically advanced, but one that is also equitable, secure, and truly centred on the patient.
If you're interested in the specific tools making this all possible, you can get more details in our guide to patient care technology.
How Virtual Care Is Redefining Patient Access
What was once a nice-to-have feature in Canadian healthcare has quickly become a fundamental part of the system. Virtual care is no longer a stopgap measure; it’s now a permanent and expected way for patients and doctors to connect, completely changing the game for accessing care.
Think about someone living in a rural or remote community. In the past, seeing a specialist often meant taking days off work, travelling long distances, and all the stress that comes with it. Now, that same expert consultation can happen over a video call from their own living room. It turns a logistical nightmare into a simple appointment.
This isn't just about making life easier; it’s about creating a more equitable system. Through telehealth and remote monitoring, we're finally extending quality healthcare to populations that have been historically underserved. Your postcode is becoming less of a barrier to getting the care you need.
From Policy to Practice
While the pandemic kicked virtual care adoption into high gear, it’s the solid backing from provincial governments that’s given it staying power. New frameworks and billing codes have been rolled out across the country, officially recognising and paying for virtual visits. This has given clinics and hospitals the confidence to truly integrate these services into their daily operations.
This government support has fuelled incredible progress, especially in a couple of key areas:
Family Medicine: Things like routine check-ups, prescription refills, and follow-up chats are now routinely handled online. This frees up precious in-clinic time and space for more complex issues that require a hands-on approach.
Mental Health Services: Offering therapy and counselling virtually has dramatically lowered the barrier for people seeking help. It provides a level of privacy and convenience that encourages more Canadians to take that first step in looking after their mental well-being.
Thanks to this policy push, virtual appointments are now a standard option. By 2025, virtual care for family medicine and mental health became commonplace across all provinces, driven by new reimbursement models and quality standards. This has been a massive win for remote communities where in-person options are few and far between. Today, about 80% of Canadian doctors are regularly using telemedicine, a huge jump made possible by supportive provincial policies. Learn more about how AI and wearables are shaping Canadian digital health.
Tracing the Modern Patient Journey
Let's walk through what a patient's experience looks like today. It often doesn't start with a phone call to a clinic anymore. Instead, it might begin with an AI-powered symptom checker that helps assess the issue and guides them to the right type of care.
From there, the next step could be a secure video chat with their family doctor. If a specialist is needed, the referral can happen digitally, leading to another virtual consultation. The patient gets the care they need, often without ever having to leave home. It’s a far more efficient and patient-friendly process.
This digital-first approach does more than just connect patients and doctors; it creates a more responsive and proactive healthcare system. By managing straightforward issues remotely, it allows clinicians to focus their in-person time on patients with the most urgent and complex needs.
Navigating the Remaining Hurdles
As promising as all this is, the road to a fully integrated virtual care system still has a few bumps. There are two big challenges that we need to tackle head-on.
First, there's the digital divide. Not everyone in Canada has reliable internet or feels comfortable using the technology needed for a virtual visit. To make sure virtual care is truly for everyone, we have to close these gaps in infrastructure and digital literacy. No one should be left behind.
Second is the critical issue of patient privacy. With more sensitive health data moving online, the need for rock-solid security is non-negotiable. We have to protect patient information from cyber threats to maintain the trust that our entire healthcare system is built on. Solving these challenges is the key to unlocking the full promise of virtual care in Canada's health future.
Solving the EHR Interoperability Puzzle
One of the biggest roadblocks to a truly modern digital health system in Canada is getting different systems to talk to each other. This is the challenge of Electronic Health Record (EHR) interoperability.
Think about it like this: you can send an email from a Gmail account to someone using Outlook without a second thought. The systems just work together. But in healthcare, it’s often like trying to send a text message from your phone to a friend, only to discover your mobile networks are completely incompatible. The message never arrives.
That’s what’s happening across much of our healthcare system. A patient's vital health information: allergies, lab results, and medical history, is frequently locked inside one hospital or clinic's specific EHR system. When that patient needs care somewhere else, the new provider is flying blind, unable to see the full picture.
This creates what we call data silos. Each system holds a piece of the patient's story, but nobody can read the whole book. This isn’t just an IT headache; it creates real-world inefficiencies and puts patient safety at risk.
The Real-World Impact of Disconnected Data
When EHRs can't share data, the consequences are felt throughout the entire care journey. The lack of a single, unified patient record means clinicians have to work with incomplete information, often pieced together from a patient's memory or a stack of faxes. This is more than just inefficient; it's a direct obstacle to providing quality care.
Here are a few common problems that pop up:
Duplicate Medical Tests: A patient might get the same blood test or MRI twice, simply because a new specialist can't get the results from another facility. This wastes money and the patient's time.
Incomplete Patient Histories: An emergency room doctor might not know about a critical allergy or a pre-existing condition because that data is trapped in another provider’s system. This can lead to dangerous, even life-threatening, treatment decisions.
Delayed Care: Precious time is lost chasing down records from other clinics. This can stall diagnoses and slow down treatment, turning coordinated care into a frustrating logistical exercise.
Ideally, a connected virtual care journey should flow seamlessly, moving from the first point of contact right through to specialist care without losing any information along the way.
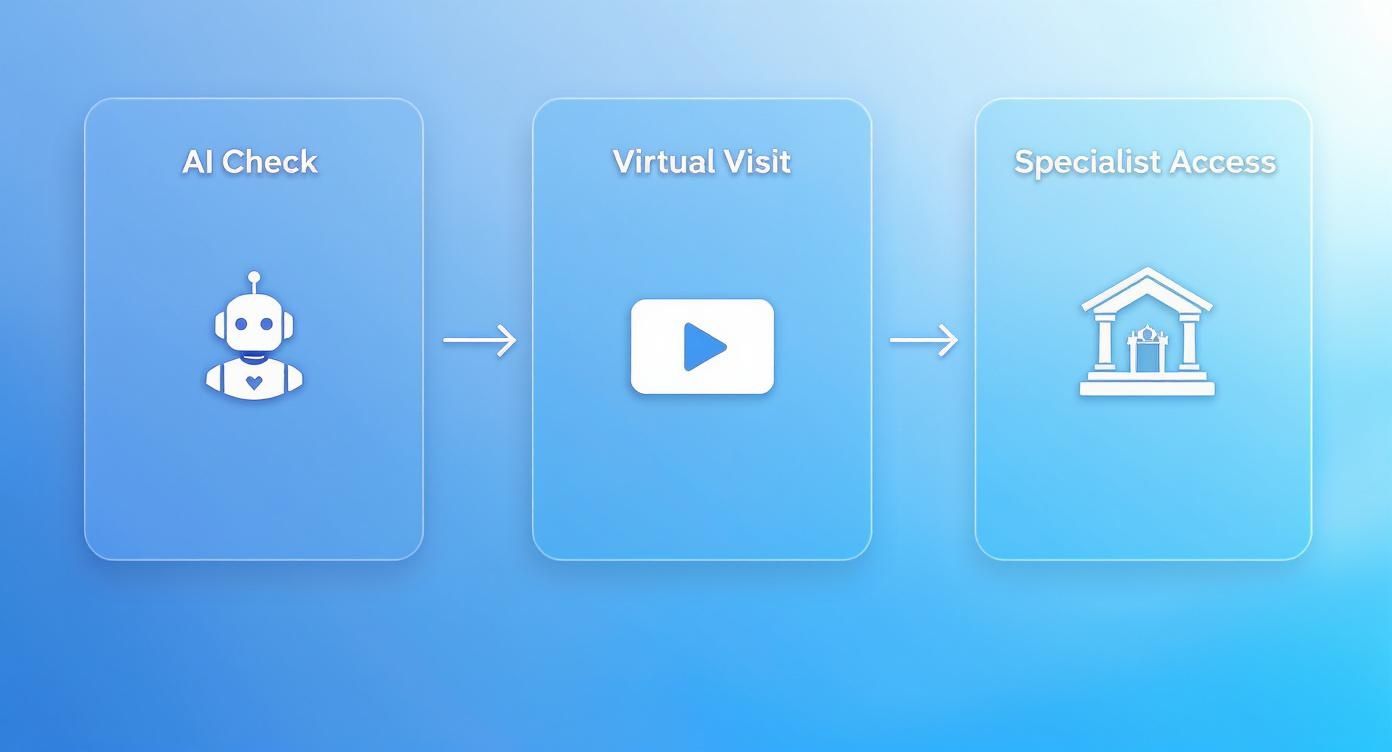
This workflow, moving smoothly from an AI-powered check-in to a virtual visit and specialist follow-up, is only possible if the underlying systems can communicate effortlessly. True interoperability is the backbone of this vision.
Progress and Persistent Challenges
Canada has certainly made progress in getting digital records into the hands of clinicians. But just because a clinic has an EHR doesn't mean it’s connected to anything.
By the second quarter of 2025, an estimated 62% of Canadian healthcare providers have adopted EHR systems, a modest but steady climb from 59% in 2024. While this shows a clear commitment to going digital, the reality on the ground is a patchwork of incompatible platforms. There are over 20 different EHR platforms being used across the country, and many vendors run multiple, non-compatible versions of their own software, making the interoperability puzzle even harder to solve. You can explore more EHR adoption trends here.
"The ultimate goal is to create a digital ecosystem where a patient's health data follows them securely, no matter where they are in Canada. Achieving this requires not just technology, but a collaborative effort to establish and enforce national data standards."
To get there, national bodies are working with provincial and territorial governments to build a set of unified standards. This means setting common rules for how health data is formatted, shared, and protected. It's a slow, complex process, but it's the essential groundwork needed to finally break down those data silos.
By building this connected infrastructure, we can move toward a truly seamless digital health system where a patient's complete story is available whenever and wherever it's needed most.
The Growing Role of AI in Canadian Healthcare

Artificial Intelligence (AI) and Machine Learning (ML) are no longer concepts from a science fiction movie; they're becoming practical tools in Canadian clinics and hospitals. The whole point isn't to replace doctors, but to give them a powerful assistant that can work with incredible speed and precision.
Think of it this way: an AI diagnostic model is like a specialist who has painstakingly reviewed millions of medical cases. This digital partner can look at a complex MRI or X-ray and spot tiny patterns the human eye might miss, flagging areas for a radiologist to take a closer look at.
This completely changes the diagnostic workflow. Instead of spending hours on manual image reviews, a clinician can bring their expertise to bear on the critical findings the AI has already pinpointed. It’s this partnership between human intuition and machine accuracy that’s really shaping the future of care in Canada.
From Theory to Practical Application
Across the country, AI is already being put to the test in ways that directly impact patients. These aren't just abstract ideas; they're real tools designed to make our healthcare system more proactive, efficient, and tailored to the individual. The aim is to get ahead of health problems, not just react to them.
For instance, AI algorithms are learning to sift through huge public health datasets to predict where a disease outbreak might happen next. This gives authorities a vital head start on mobilising resources. Other systems are helping to craft highly personalised treatment plans for tough conditions, matching therapies to a patient's specific genetic code and lifestyle.
Some of the most exciting areas right now include:
Predictive Analytics: AI can identify patients at high risk for serious issues like sepsis or heart failure, which allows for early intervention before things get critical.
Medical Imaging Analysis: These systems are being trained to spot early signs of cancer or diabetic retinopathy in scans with amazing accuracy, often much faster than we could before.
Personalised Medicine: By analysing genomic data, AI can help figure out which drug therapies are most likely to work for a specific person, cutting down on the frustrating trial-and-error process.
By processing enormous volumes of data, AI can uncover insights that lead to earlier diagnoses and more effective treatments. This data-driven approach supports clinicians in making better-informed decisions, ultimately enhancing the quality and safety of patient care.
These are just the first steps. To see how these ideas are already taking shape, our deep dive into AI healthcare solutions in Canada gives you a closer look at current projects and what’s on the horizon.
Navigating the Ethical Maze
As we start using these powerful tools, we also have to face some serious ethical questions. For AI to be effective and fair, we have to get this part right. It all comes down to trust, and that can only be built with total transparency and clear accountability.
The first big hurdle is data privacy. AI models need a massive amount of health data to learn from, and protecting that sensitive information is non-negotiable. This means strict adherence to Canadian privacy laws like PIPEDA is an absolute must, ensuring patient data is kept anonymous and secure at every stage.
Another major issue is algorithmic bias. If an AI is trained on data that mostly comes from one group of people, its insights and predictions might not be accurate for others. This could actually make existing health inequalities worse. Development teams have to work intentionally to make sure their training data is diverse and truly represents Canada's population.
Finally, there’s the question of accountability. When an AI-assisted diagnosis leads to a poor outcome, who is responsible? We need clear rules that define the roles of the tech company, the hospital, and the doctor. Getting the fundamentals right, like proper medical annotation for healthcare AI, is a key first step toward building systems we can all rely on.
By tackling these ethical challenges head-on, we can make sure AI becomes a fair and dependable tool in building a better, more equitable healthcare system for every Canadian.
Here's the rewritten section, designed to sound like it was written by a human expert.
How Policy Is Shaping Digital Health Innovation
You can have the best technology in the world, but without the right policies to support it, it’s not going anywhere. In Canada, building a thriving digital health ecosystem is as much about policy as it is about tech. The real challenge? It involves a delicate dance between federal, provincial, and territorial health authorities.
This isn’t a simple setup. The federal government might set the broad vision and open the chequebook, but it’s the provinces and territories that are on the ground, actually delivering healthcare. This division of power often creates a messy patchwork of standards and regulations across the country. For innovators, that can mean trying to build a national solution that has to navigate thirteen different rulebooks. Getting these different bodies to work in concert isn't just a nice-to-have; it's the only way forward.
Without that coordination, progress stalls. We end up slowing down the very technologies that could benefit everyone, simply because the path to market is too complicated.
Crafting the Rules of the Road
If we're going to build a digital health system people can trust, it all starts with a rock-solid legal framework for protecting patient data. The cornerstone in Canada is the Personal Information Protection and Electronic Documents Act (PIPEDA). This is the federal law that sets the ground rules for how private-sector organisations handle personal information.
But PIPEDA is just the starting line. Provinces often have their own "substantially similar" legislation, which means anyone building a health solution needs to be fluent in both federal and provincial privacy rules. These laws aren't just red tape; they are the bedrock of patient trust.
Building a secure "digital front door" for healthcare is non-negotiable. Patients must have absolute confidence that their most sensitive information is locked down with strong security and clear privacy laws. In digital health, trust is everything.
Beyond privacy, a few other policy areas are absolutely critical to get right:
Data Security Protocols: We need clear mandates for cybersecurity measures. Think strong encryption and regular security audits to defend our health systems against the constant threat of cyberattacks.
Technology Adoption Incentives: Governments can accelerate modernisation by offering funding and programmes that help clinics and hospitals adopt modern EHRs and virtual care platforms. It greases the wheels of progress.
Interoperability Standards: It’s crucial that policies require new digital health tools to speak the same language. This prevents us from simply trading our old paper silos for new digital ones.
Closing the Digital Divide
One of the biggest policy hurdles is making sure digital health benefits everyone, not just those in urban centres with a fast internet connection. The "digital divide" – that gap between people who have reliable internet and digital skills and those who don't, is a massive barrier to equitable healthcare.
Bridging this gap has to be a central part of the policy conversation. That means investing in broadband for rural and remote communities, funding digital literacy programmes for seniors, and pushing for technology that’s accessible for people with disabilities. The goal is simple: build a system that leaves no one behind.
Ultimately, good policy creates a stable, predictable environment. For tech companies, that clarity reduces risk and makes it more attractive to invest in solutions tailored for Canada. For doctors and hospitals, it provides the confidence to adopt new tools, knowing they meet national standards for safety and privacy. At the end of the day, well-designed policy is the engine that will truly power the future of digital health in this country.
A Practical Roadmap for Providers and Innovators
Knowing where Canadian digital health is headed is one thing, but actually getting there is another challenge entirely. For healthcare providers on the front lines and the tech innovators building the tools, the real work begins now. It’s all about turning these big-picture trends into smart, practical strategies.
Success hinges on a two-pronged approach: thoughtful adoption in the clinic and user-focused design from the tech side.
For clinics, hospitals, and other providers, the journey doesn’t start with buying new software. It starts with your people. Bringing new technology into a healthcare setting is, at its core, an exercise in change management. It’s about getting your staff ready for new ways of working, training them properly, and showing them how these tools will make their jobs easier and improve patient care.
A Phased Approach for Healthcare Providers
Jumping into a massive digital overhaul can feel overwhelming. A structured, step-by-step approach makes the whole process much more manageable and far less disruptive.
Assess Clinical Needs: Before you look at any technology, look at your own workflow. What are your biggest headaches right now? Is it chaotic appointment scheduling? Inefficient patient follow-up? The daily struggle of tracking down patient records? Focus on finding a solution that solves a real, pressing problem you face every day.
Pilot Small-Scale Projects: Don't try to change everything at once. Pick a small, motivated team and test a new tool with them first. This creates a safe space to work out the kinks, gather honest feedback, and build a solid case for a wider rollout based on actual results, not just promises.
Invest in Continuous Training: The technology will keep changing, and so should your team’s skills. Think of training not as a one-time event, but as an ongoing process. Consistent education is the only way to get the most out of your digital tools and make sure your staff feels confident using them.
Opportunities for Technology Innovators
For the tech companies and developers out there, the biggest opportunities are in building solutions that are genuinely intuitive, totally secure, and solve a specific clinical problem. The Canadian market doesn't need another flashy app; it needs powerful, reliable tools that can plug directly into the complicated reality of a clinic or hospital.
The digital health tools that truly succeed will be the ones built with a deep understanding of what both patients and providers actually go through every day. Usability isn’t just a nice-to-have feature; it’s the bedrock of safe and effective healthcare technology.
Innovators have to zero in on user-friendly design and prove they get the nuances of Canada's provincial privacy and security rules. Creating a solid product in this space demands serious expertise. Often, the best path forward is to look into options like custom healthcare software in Canada to get the specialised know-how required to navigate this field. By working hand-in-hand with clinicians, tech companies can build the tools that will genuinely define the future of care.
Frequently Asked Questions
As Canada moves toward a more connected healthcare system, a lot of good questions come up. Here, we tackle some of the most common ones to help make sense of where we're headed.
What's the Single Biggest Hurdle for Digital Health in Canada?
If you had to point to one thing, it would be the lack of interoperability. Think of it like this: because each province manages its own healthcare, we've ended up with a patchwork of different Electronic Health Record (EHR) systems from various vendors. The problem is, they don't speak the same language.
This creates "data silos," which is just a technical way of saying a patient's information gets trapped in one hospital's or clinic's system. Sharing that critical data with a specialist across town, let alone in another province, becomes a massive headache. The real solution involves setting national data standards and giving vendors a good reason to build systems that can finally talk to each other – a tough but necessary step.
It’s not a technology problem; it's a connection problem. For digital health to work, patient information needs to flow securely and smoothly between every point of care, no matter the software or the province.
How Will Artificial Intelligence Actually Change My Doctor's Appointment?
AI isn't about replacing your doctor; it's about giving them a major upgrade. In the very near future, AI will work behind the scenes as a highly intelligent assistant, making your care better in a few key ways:
Smarter Triage: Before you even book an appointment, an AI tool could help analyse your symptoms and guide you to the right place; whether that's a virtual consultation, a family doctor, or the emergency room.
A Second Set of Eyes: It can scan medical images like MRIs or X-rays with incredible precision, flagging subtle details for a radiologist to review.
Tailored Treatments: AI can sift through massive amounts of medical research in seconds, helping your doctor find the most effective and personalised treatment plan based on your unique health profile.
The goal here is simple: arm your doctor with better information so they can make faster, more accurate decisions. That means more precise and effective care for you.
Can I Trust Digital Health Services with My Personal Information?
Keeping patient data safe is the bedrock of this entire shift. Canada’s approach to digital health is guided by some of the world's strictest privacy laws. Regulations at both the federal and provincial levels, especially the Personal Information Protection and Electronic Documents Act (PIPEDA), lay down firm rules on how your health information can be handled.
Healthcare organisations aren't just asked to be careful; they're legally required to protect your data with powerful security measures like encryption and controlled access. While no system is ever 100% invulnerable, the legal framework is designed to ensure your sensitive information is treated with the highest standard of care and to hold organisations accountable if they fail.
At Cleffex Digital Ltd, we focus on building secure, compliant software that solves the real-world problems facing Canada's healthcare sector. If you're ready to create the next generation of digital health tools, we have the expertise to navigate the complexities and turn your vision into reality. See how we can help your project at Cleffex.com.







