AI-driven healthcare solutions aren't just about futuristic algorithms; they're about using machine learning to make sense of incredibly complex medical data. Think of it as giving clinicians a powerful collaborator that helps them make faster, more accurate decisions, ultimately leading to real improvements in patient care and hospital operations.
The New Era of Healthcare AI

Imagine a highly skilled assistant working alongside every healthcare professional – one that can sift through immense datasets in seconds to flag potential issues or suggest better treatment paths. That's the reality of today's AI-driven healthcare tools. For years, artificial intelligence was more of an experimental concept in medicine, but it has finally matured into practical applications that are being embedded directly into clinical and administrative workflows.
This guide isn't about abstract ideas. We're going to dig into how AI is becoming an indispensable partner in modern medicine. You'll see exactly how these technologies deliver tangible value, whether it's by boosting diagnostic accuracy, personalising patient treatments, or simply making hospital operations run more smoothly. The focus here is on practical application, not just theory.
What You Will Learn in This Guide
This is more than just a surface-level overview. We've put together a clear and comprehensive roadmap for healthcare leaders, clinicians, and IT professionals who are ready to move from discussion to action. Our goal is to give you a deep understanding of what it really takes to implement these advanced systems successfully.
Our journey will cover:
Practical Applications: We’ll explore real-world examples of how AI is being used in diagnostics, treatment planning, and hospital management right now.
Technical Foundations: We'll demystify the core components, breaking down machine learning models, data architecture, and the necessary tech stack into plain English.
Regulatory and Privacy Challenges: You'll learn how to navigate the critical landscape of data privacy, security, and compliance with Canadian standards like PIPEDA.
Implementation and ROI: We provide a step-by-step guide to deploying AI, from small pilot projects to measuring the true impact on patient outcomes and operational costs.
The core promise of AI in this field isn’t to replace human experts, but to augment their abilities. It processes information at a scale and speed that humans simply can’t, uncovering insights that lead to proactive, rather than reactive, patient care.
Our goal is to give you the knowledge needed to make informed decisions. We'll look at both the incredible potential and the very real hurdles of integrating AI into a healthcare setting. For a closer look at the specific advantages, you can learn more about the benefits of AI in the healthcare industry in our detailed article.
By the time you finish this guide, you’ll have a clear framework for evaluating, planning, and executing an AI strategy that delivers meaningful results for your organisation and, most importantly, for the patients you serve.
Where AI is Making a Real Difference: Clinical Care vs. Hospital Operations
Artificial intelligence is no longer just a buzzword in healthcare; it's actively changing how things get done, from the operating room to the back office. Its influence really branches into two main areas: the clinical side, which is all about patient diagnosis and treatment, and the operational side, which focuses on making the entire healthcare system run smoothly. Looking at both gives you the full picture of how AI-driven healthcare solutions are creating real value.
On the clinical front, think of AI as a super-powered assistant for doctors. It can sift through incredibly complex medical data, like MRIs, CT scans, and genetic information, to spot subtle patterns a person might miss. This isn't about replacing radiologists or oncologists. It’s about giving them better tools to make earlier, more accurate diagnoses.
For example, AI algorithms trained on thousands of mammograms can flag suspicious areas with incredible precision, guiding a radiologist’s attention to potential cancers much sooner. In a similar way, predictive models can analyse a patient's electronic health record (EHR) to flag their risk of developing a critical condition like sepsis, allowing doctors to step in before it becomes a crisis.
Elevating Patient Care with AI
Personalised medicine is where AI is truly starting to shine. Instead of a one-size-fits-all approach, AI helps build care plans specifically for an individual’s unique biology and lifestyle.
Customised Treatment Plans: An AI system can analyse a patient's genomic data and cross-reference it with clinical trial results to suggest cancer therapies most likely to work on their specific tumour type.
Predictive Health Monitoring: Wearable devices are constantly collecting data. AI platforms can analyse this stream to predict health events, like a hypoglycemic episode in a diabetic patient or an irregular heartbeat, alerting both the person and their care team.
Disease Outbreak Forecasting: On a much larger scale, AI can analyse population health data to forecast the spread of infectious diseases, which helps public health officials get resources where they’re needed most.
This move toward data-driven, personalised care is a huge leap forward in improving patient outcomes. It shifts the focus from just treating sickness to proactively managing health.
Streamlining Healthcare Operations
While the clinical applications grab the headlines, the operational impact of AI is just as important. Hospitals and clinics are complex beasts, often bogged down by a mountain of administrative work. AI solutions are built to automate tedious tasks, manage resources better, and cut down on waste.
Just think about the paperwork involved in patient admissions, billing, and insurance claims. AI-powered tools are taking on a lot of that load. Natural Language Processing (NLP) can pull key information from a doctor's notes to pre-fill claim forms. Meanwhile, machine learning models can audit those claims for errors before they're submitted, which dramatically reduces denial rates.
By taking over routine administrative tasks, AI gives clinicians and staff back their most valuable resource: time. They can spend less of it on clerical work and more on what actually matters – caring for patients. This not only boosts efficiency but also helps tackle the problem of professional burnout.
The adoption of these technologies is picking up speed, although many are still in their early days. For instance, an inventory of AI solutions in California’s health plans showed that while deployment is growing, only about one-third of the identified tools are fully up and running. These applications cover a huge range of functions, from clinical support to administrative automation. You can dig into the specifics in the 2025 CalPERS Health Plan AI Inventory.
As AI smooths out these various processes, it opens up new avenues for improving productivity through optimised operational workflows.
To make the distinction clearer, let's break down how AI is used in both clinical and operational settings.
Clinical vs Operational AI Healthcare Applications
The table below highlights the different goals, examples, and benefits of AI in these two core areas of healthcare.
| Application Area | Primary Goal | Example Use Case | Key Benefit |
|---|---|---|---|
| Clinical | Improve Patient Outcomes & Diagnostic Accuracy | AI-powered analysis of medical images (X-rays, MRIs) to detect anomalies. | Earlier disease detection and more accurate diagnoses. |
| Operational | Enhance Efficiency & Reduce Costs | Automated patient scheduling and hospital bed management systems. | Reduced patient wait times and optimised resource utilisation. |
| Clinical | Personalise Treatment | Using genomic data to recommend targeted therapies for cancer patients. | Higher treatment efficacy and fewer adverse effects. |
| Operational | Simplify Administrative Tasks | Automating the medical coding and insurance claims submission process. | Faster reimbursement cycles and lower administrative overhead. |
Ultimately, the real magic of AI-driven healthcare solutions happens when these two streams – clinical and operational – work together. A well-run hospital gives clinicians more time to use advanced diagnostic tools, which leads directly to better, more personalised care for every patient who walks through the door.
Understanding the Technology Behind Healthcare AI
To really get a handle on how AI-driven healthcare solutions work, it’s helpful to picture them as a sophisticated, multi-layered system. Each layer has a specific job, from gathering raw data all the way to delivering insights a clinician can actually use. Let's peel back the curtain on this technical stack to see not just what each part is, but why it's so crucial for building a solid and secure AI tool.
Everything starts with the data foundation. This is the bedrock. We're talking about a massive collection of information from all corners of the healthcare ecosystem: electronic health records (EHRs), detailed medical images like MRIs and CT scans, genomic sequences, and even live data streams from patient monitors and wearables.
To wrangle this sheer volume and variety, organisations often rely on a data lake. Think of it as a vast, digital reservoir that can hold both structured and unstructured data at any scale. It’s where every bit of health information, no matter the format, is stored and prepped for analysis.
The Engine Room: Machine Learning Models
One layer up, we find the processing engine – the heart of the whole operation. This is where the real "intelligence" gets built. Here, machine learning (ML) and deep learning algorithms are trained on the data to spot complex patterns that would be nearly impossible for a human to see. Different jobs call for different kinds of models, each one a specialist.
Convolutional Neural Networks (CNNs): These are the visual experts, tailor-made for medical imaging. A CNN can learn to identify the faintest anomalies in an X-ray or flag potential tumours on a mammogram with impressive accuracy. We explore this in more detail in our guide on AI for medical imaging and diagnostics.
Natural Language Processing (NLP): This technology is all about understanding human language. In a hospital setting, NLP models can read a doctor's unstructured clinical notes or patient feedback, pulling out key information to update records or gauge patient sentiment.
Time-Series Models: These algorithms excel at analysing data collected over time, like an ECG trace or blood sugar readings from a continuous glucose monitor. By spotting trends, they can predict future events, like flagging a potential cardiac event based on subtle changes in a patient's heart rhythm.
This infographic gives a great visual breakdown of the two main areas where these technologies make an impact.
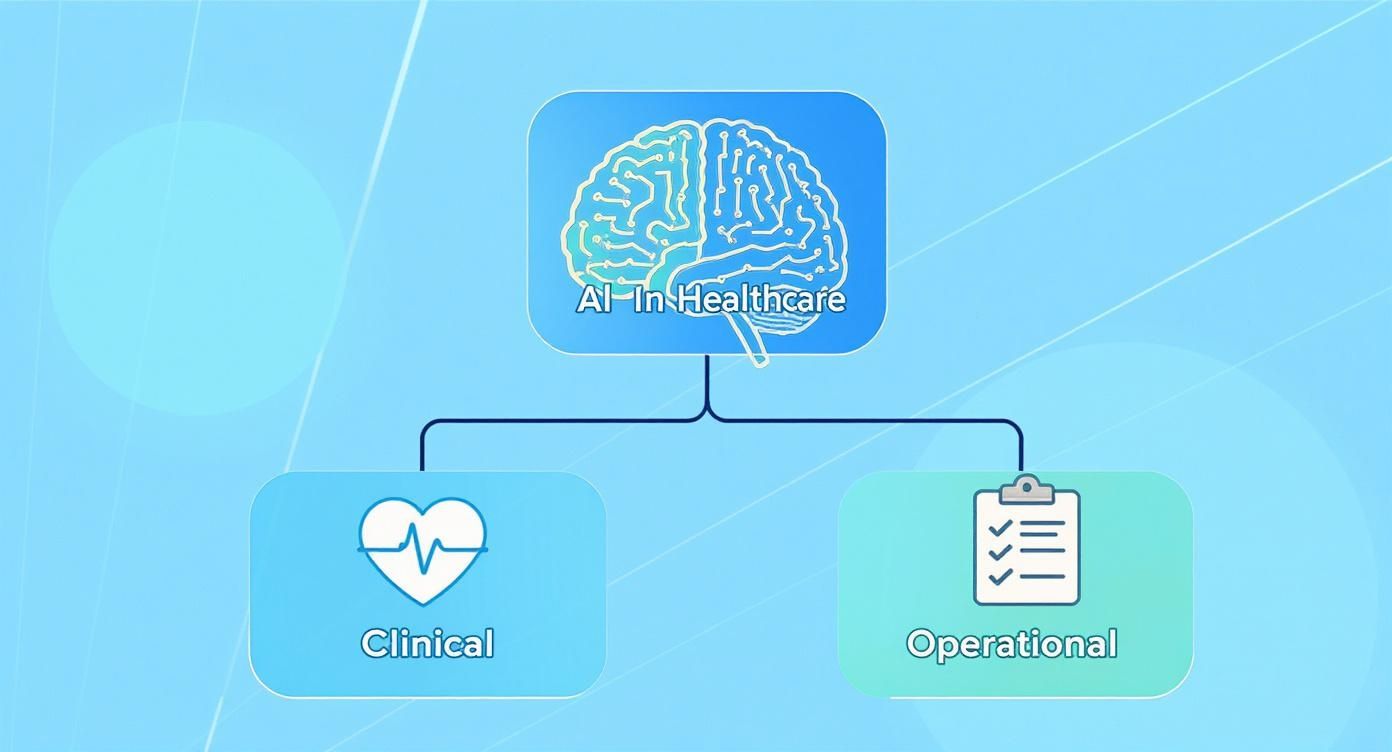
As you can see, the core AI engine serves both patient-facing clinical functions and the operational needs behind the scenes, showing just how versatile it is.
Bringing Insights to the User
The final piece of the puzzle is the application and integration layer. This is the part of the system that people – clinicians, administrators, and sometimes patients – actually interact with. It takes the complex findings from the machine learning models and serves them up in a clear, useful way, often right inside the software they already use every day.
The most powerful AI model is useless if its insights can't be seamlessly delivered to the right person at the right time. This final layer is all about bridging the gap between algorithmic prediction and real-world clinical action.
This is where Application Programming Interfaces (APIs) come in. APIs are like digital messengers that let different software systems talk to each other. For instance, an API can connect an AI imaging tool directly into a hospital’s Picture Archiving and Communication System (PACS), automatically highlighting urgent cases within the radiologist’s standard workflow. In the same way, an API can push an alert from a predictive model into the EHR, notifying a nurse that a specific patient is at high risk for a fall.
Together, these layers – data, processing, and application – form the complete architecture of modern AI-driven healthcare solutions. Building a truly effective system means getting every level right, ensuring the data is clean, the models are accurate, and the insights are delivered in a way that genuinely enhances patient care.
Navigating Data Privacy and Regulatory Hurdles

In healthcare, trust is everything. As we weave AI-driven healthcare solutions deeper into our clinics and hospitals, we unlock incredible potential. But we also face a new, more complex set of challenges around patient privacy, data security, and the ever-present web of regulations.
Protecting sensitive health information isn’t just a box to tick on a compliance form; it's the ethical bedrock of the patient-provider relationship. Getting this right means building safeguards into the very fabric of an AI system from day one. It demands a solid understanding of Canada's legal landscape, especially the Personal Information Protection and Electronic Documents Act (PIPEDA), which lays down strict rules for handling patient data.
Building Trust Through Privacy by Design
The smartest way to tackle this is with a Privacy by Design philosophy. This isn't about adding security features at the end of a project. It’s about making privacy a core, non-negotiable part of the system's architecture from the very beginning. The idea is to make robust data protection the default setting, so patient information is kept safe automatically.
Let's be clear: people are rightfully concerned about their data. A recent survey from the Carnegie Endowment for International Peace found that a staggering 81% of respondents were not comfortable with AI systems sharing their personal information. While this was a general survey, it sends a powerful message about the high bar for privacy in a field as sensitive as healthcare.
To move forward, we need practical strategies that drive innovation without ever compromising patient confidentiality.
The question isn't whether to innovate or protect privacy; it's how to innovate by protecting privacy. The strongest AI solutions are those that earn trust by demonstrating a clear and unwavering commitment to securing patient data at every turn.
This involves some clever techniques for managing data responsibly. For a deeper dive, check out our guide on https://www.cleffex.com/blog/ai-in-healthcare-data-privacy-canada/.
Key Strategies for Securing Patient Data
Protecting data for AI models goes beyond standard encryption. It calls for specialised methods that limit data exposure while still letting the algorithms learn effectively.
Here are three essential strategies every healthcare organisation should consider:
Data Anonymisation and Pseudonymisation: Before any data gets near an AI model for training, all personally identifiable information (PII) must be stripped out. This means names, addresses, and health card numbers are removed or swapped with a random token, effectively severing the link between the data and the individual.
Federated Learning: This is a truly clever approach. Instead of moving massive amounts of sensitive data to a central server, the AI model travels to the data. The model trains locally on a hospital's or clinic's own servers, and only the anonymous insights – not the raw data – are sent back to refine the central algorithm. This dramatically shrinks the risk of a large-scale data breach.
Privacy Impact Assessments (PIAs): Think of a PIA as a risk-assessment blueprint for privacy. It’s a formal process to identify and address potential privacy pitfalls before an AI solution goes live. Conducting a thorough PIA is a critical step to prove due diligence and ensure you're building a system that’s compliant right from the start.
Ensuring Transparency with Explainable AI
One of the biggest trust barriers with AI is the "black box" problem. An AI might make a brilliant recommendation, but if no one can understand why, it's useless in a clinical setting where every decision can have life-or-death implications.
This is where Explainable AI (XAI) comes in. XAI is a collection of tools and methods designed to make AI decision-making transparent and understandable to people. For instance, if an AI model flags a mammogram as potentially cancerous, an XAI system would highlight the exact pixels or patterns that led to its conclusion.
This level of transparency is non-negotiable for gaining the trust of clinicians and satisfying regulators. It allows doctors to validate the AI’s logic, establishes clear accountability, and simplifies compliance with complex rules. Navigating these regulations is crucial, and you can find more guidance on frameworks like essential GDPR compliance. By building AI that is transparent, secure, and compliant, we can truly enhance patient care without chipping away at the trust that holds it all together.
Your Roadmap for Implementing AI Solutions
Bringing AI into your healthcare organisation isn't a one-and-done tech install; it’s a journey. A successful rollout hangs on a clear, phased plan that turns technological promise into real-world clinical value. Think of this roadmap as a practical framework built for healthcare settings, ensuring your AI initiative is strategically sound, sustainable, and actually solves a problem.
It all starts by zeroing in on a specific, high-impact issue. Resist the allure of "AI for AI's sake." Instead, ask the tough questions. Where are our biggest operational drags? Which diagnostic pathways are most prone to error? What administrative black hole is eating up our team's time? By anchoring your project to a well-defined problem, you set a clear finish line from day one.
For instance, maybe your hospital is wrestling with long emergency department wait times. An AI tool could be brought in to predict patient admission volumes from live data, helping you align staffing and resources more effectively. This focused approach gives the project an immediate, undeniable purpose.
Phase 1: Laying the Foundation
Before you even think about algorithms, you need to take a hard look at your organisation's readiness. This foundational phase is all about getting your house in order across three key areas: data, people, and processes. If you skip this, even the most brilliant AI tool will fall flat.
Assess Your Data Readiness: AI models are hungry for data, and they’re picky eaters. They’re only as good as the information they’re fed. You need to honestly evaluate the quality, volume, and accessibility of your data. Are your Electronic Health Records (EHRs) a mess of inconsistent entries? Is your imaging data locked away in a siloed archive? Finding these data gaps early lets you build a plan to clean, standardise, and harmonise everything before you get started.
Assemble a Cross-Functional Team: Getting AI right is a team sport. It demands a mix of perspectives: clinicians who live and breathe the daily workflow, IT experts who know the infrastructure inside and out, data scientists who can build the models, and leadership who can provide the vision and resources. This mix ensures the final solution is clinically relevant, technically possible, and tied directly to your organisation's goals.
Define What Success Looks Like: How will you know if this actually worked? You need to set your key performance indicators (KPIs) before you write a single line of code. For that emergency department example, success might look like a 15% reduction in average wait time or a 10% improvement in patient satisfaction scores.
Phase 2: Pilot and Validation
With the groundwork laid, it’s time to launch a controlled pilot program. A pilot is your small-scale test flight, a chance to evaluate feasibility, costs, and any unexpected bumps in the road. It’s all about minimising risk and allowing for tweaks before you go all-in.
A pilot program acts as a real-world laboratory. It’s where you validate your assumptions, uncover unforeseen challenges in a low-stakes environment, and gather the hard data needed to build a compelling business case for wider adoption.
This is also when you'll pick your technology partner or vendor. Look for a team with a proven track record in healthcare, a deep understanding of regulatory hurdles, and a solution that plays nicely with your existing systems, like your EHR. How the pilot performs against your KPIs will tell you whether to move forward, adjust your strategy, or go back to the drawing board.
Phase 3: Scaling and Integration
Once your pilot proves its worth, the final phase is about scaling the solution and weaving it into your daily clinical fabric. This is about much more than just a technical hookup; it requires smart change management to win the trust and adoption of your clinicians. Think clear communication, hands-on training, and demonstrating exactly how the tool makes their lives easier.
As you scale, the regulatory environment becomes even more critical. Staying on top of evolving legislation is non-negotiable. In California, for example, new rules are already taking shape. Assembly Bill 3030, which kicks in on January 1, 2025, will require healthcare facilities using generative AI to clearly disclose its use to patients. Transparency is becoming law. You can read more about how California is regulating AI in healthcare and what that means for the future on chambers.com.
By following a structured roadmap, your organisation can systematically de-risk its AI initiatives and build tools that deliver real, lasting value.
Measuring the True Impact of Healthcare AI
So, you've invested in a new AI solution. How do you actually know it's working? The answer isn't just about the money you're saving. To really understand the value of AI-driven healthcare solutions, you need to look at the whole picture – how it's affecting clinical care, daily operations, and the patient experience.
Think of it as a balanced scorecard. This approach helps you show the full value to everyone involved. The executive board wants to see the numbers, but the doctors and nurses on the floor need to see how it makes their jobs and their patients' lives better. It's this comprehensive view that builds momentum and secures ongoing support for innovation.
Beyond the Bottom Line: Clinical Metrics
Ultimately, the real test of any healthcare technology is its impact on patient outcomes. These are the metrics that show you're improving the quality of care, and they provide the strongest evidence that your AI tool is worth the investment.
Here are a few key things to track:
Reduced Patient Readmission Rates: If your AI can flag patients at high risk of returning to the hospital, you can step in sooner. A noticeable drop in your 30-day readmission rate is a huge win.
Improved Diagnostic Accuracy: Are your radiologists and pathologists catching more with AI's help? Look for a percentage increase in correct diagnoses or a reduction in false negatives.
Faster Time-to-Treatment: In critical situations like a stroke, every second counts. AI can slash the time it takes from scan to treatment, and tracking this improvement in minutes can literally show how lives are being saved.
Gauging Operational and Experiential Gains
While better patient health is the primary goal, the operational wins are what often keep the lights on for these projects. Creating smoother workflows and a less stressful journey for patients are essential pieces of the puzzle.
The true impact of AI is realised when operational improvements create more time and resources for clinical excellence. By reducing administrative friction, you empower clinicians to focus entirely on patient care.
Keep an eye on improvements in these areas:
Lower Administrative Costs: When you automate things like medical coding, billing, or scheduling, you're not just cutting costs; you're also cutting down on human error.
Shorter Patient Wait Times: AI-powered systems for managing patient flow and bed availability can make a world of difference in a busy emergency department, leading to a much better experience for everyone.
Improved Clinician Satisfaction: This is a big one that often gets missed. By taking tedious paperwork off their plates, AI can be a powerful tool against burnout, helping you retain your best people.
To help you get started, here's a breakdown of some key performance indicators (KPIs) you can use to measure the success of your AI initiatives across these different domains.
Table: Key Performance Indicators for Healthcare AI
| Metric Category | Example KPI | What It Measures |
|---|---|---|
| Clinical Outcomes | 30-Day Readmission Rate | The effectiveness of predictive models and proactive patient care interventions. |
| Diagnostic Error Rate | The AI's contribution to improving the accuracy of diagnoses in fields like radiology or pathology. | |
| Time-to-Diagnosis/Treatment | The efficiency gain in critical care pathways, such as identifying sepsis or stroke faster. | |
| Operational Efficiency | Administrative Task Automation Rate | The percentage of repetitive tasks (e.g., coding, scheduling) handled by AI, freeing up staff time. |
| Average Patient Wait Time | The impact of AI-driven optimisation on patient flow and resource allocation in clinics or emergency departments. | |
| Bed Occupancy Rate Optimisation | The ability of AI to improve hospital capacity management and reduce patient transfer delays. | |
| Patient Experience | Patient Satisfaction Scores (e.g., HCAHPS) | Correlation between AI implementation (e.g., faster service, better communication) and patient sentiment. |
| No-Show Rate Reduction | The success of AI-powered predictive appointment reminders and smart scheduling. | |
| Clinician Experience | Clinician Burnout/Satisfaction Surveys | The perceived impact of AI on reducing administrative burden and improving work-life balance for medical staff. |
| Time Spent on EHR Data Entry | The reduction in manual documentation time, allows for more focus on direct patient interaction. |
Tracking these kinds of metrics paints a complete and compelling story. It proves that your AI projects aren't just another expense, but a fundamental driver of better, more efficient healthcare for everyone.
Ready to build secure, compliant, and impactful AI-driven solutions for your healthcare organisation? Cleffex Digital Ltd has the expertise to guide you from initial concept to successful implementation. Discover our custom software development services today.







