When we talk about patient care technology, we're referring to the entire suite of digital tools, software, and devices that healthcare professionals rely on to manage patient health and keep their clinics running smoothly. Think of it as the central nervous system for modern medicine: a network that connects everything from a patient's digital chart to sophisticated diagnostic equipment.
This technology is fundamentally changing how medicine is practised. We're moving away from a reactive model, treating sickness as it appears, and toward a proactive one that prioritises prevention and highly personalised care.
Defining the Digital Shift in Healthcare

At its heart, patient care technology includes any digital solution that touches a patient's journey through the healthcare system. This isn't just about massive, complex platforms for big hospitals anymore. These tools are now indispensable for clinics of all sizes, helping them deliver smarter, safer, and more efficient care every single day.
Let's put it this way: a doctor's handwritten note in a manila folder is a static, isolated piece of information. An entry into an Electronic Health Record (EHR), on the other hand, is alive. It can be shared instantly with a specialist across the country, automatically flag a potential drug interaction, or even contribute to a massive dataset that helps researchers predict public health trends. That’s the real power of this digital shift.
From Administration to Active Care
Initially, the first wave of healthcare tech was all about improving back-office efficiency. The goal was to digitise records, automate billing, and streamline appointment scheduling. While those functions are still absolutely critical, the scope has widened considerably.
Today’s tools play a much more active role in clinical decision-making and even direct patient interaction. This evolution is happening for a few key reasons:
Better Connectivity: The rise of high-speed internet and cloud computing means we can now securely send and receive huge amounts of health data in an instant.
Accessible Hardware: Everyone has a smartphone, and many people use tablets and wearable sensors. This makes it far easier to collect and monitor health information from literally anywhere.
Smarter Software: Sophisticated algorithms and artificial intelligence can now sift through complex data to find patterns and insights that a human could never spot alone.
The backbone for many of these modern systems is a secure, flexible cloud infrastructure. To get a better sense of how it all connects, our guide to cloud-based medical systems dives deep into the technology that makes it possible.
By bringing these digital tools together, healthcare providers create a continuous loop of care. Information flows from the patient to the clinician and back again. This allows for real-time adjustments to treatment plans and builds a much more collaborative relationship between patients and their care teams.
Ultimately, the goal of patient care technology is to enhance the incredible skills of healthcare professionals, not to replace them. It handles the repetitive work, provides deeper analytical insights, and extends a clinician's reach far beyond the clinic walls. By freeing them up, it empowers them to focus on what truly matters: delivering high-quality, empathetic care.
Exploring Key Types of Patient Care Technology
The world of patient care technology isn't a single, one-size-fits-all solution. It’s more like a well-stocked workshop where every tool has a specific job, but they all work together to build a better outcome. Getting to know these core categories is the first step in understanding how they can support both clinicians and patients.
At the very foundation, you have Electronic Health Records (EHRs). These are so much more than digital filing cabinets; they're the central nervous system for all patient information. An EHR holds everything from a patient's medical history and lab results to immunisation dates and allergy information, creating one single source of truth for the entire care team.
This accessibility is a game-changer. When a family doctor, a specialist, and an emergency room physician can all see the same up-to-date chart, the risk of errors plummets. It’s the difference between each musician in an orchestra having their own sheet of music versus trying to play a symphony from memory.
Extending Care Beyond the Clinic Walls
While EHRs provide the digital backbone, telehealth platforms are what extend a provider's reach far beyond the clinic's physical walls. Using video conferencing and secure messaging, telehealth connects patients with their clinicians remotely, which has made healthcare dramatically more accessible.
This became especially clear during the COVID-19 pandemic. Before 2020, telehealth was barely on the radar for many. By 2021, however, about half of all adults in California reported using it. The numbers are staggering: for Medi-Cal members, monthly visits shot up nearly 18-fold between 2019 and 2020.
Telehealth is more than a convenience; it's a critical tool for bridging gaps in care. It helps patients in rural areas see specialists, allows people with mobility issues to get consultations from home, and offers a safer option for those who are immunocompromised.
Another powerful tool for care outside the clinic is Remote Patient Monitoring (RPM). RPM relies on connected devices – things like continuous glucose monitors, smart blood pressure cuffs, or wearable heart rate trackers – to collect and send patient health data back to the clinical team in real time.
Think about a patient with diabetes. Instead of relying on manual logs, a device can automatically send glucose readings to the doctor's EHR. If a reading is dangerously high or low, the system can trigger an alert, letting the team step in before it becomes a crisis. This constant stream of data paints a much more accurate picture of a patient's health than a few office visits a year ever could.
Empowering Clinicians with Smarter Tools
Beyond just collecting and sharing data, modern patient care technology is designed to help clinicians make better, more informed decisions right in the moment. Two key areas driving this are AI-assisted medical imaging and clinical decision support systems.
AI-Assisted Medical Imaging: Artificial intelligence algorithms can scan diagnostic images like X-rays, CTs, and MRIs to flag potential abnormalities that might be tough for the human eye to spot. It’s like having a second set of expert eyes on every scan, helping radiologists prioritise urgent cases and boost diagnostic accuracy.
Clinical Decision Support Systems (CDSS): These systems are built right into the EHR, offering evidence-based prompts and alerts during the care process. A CDSS might warn a doctor about a potential drug interaction before they hit 'prescribe' or suggest a treatment protocol based on the very latest clinical guidelines.
Finally, a whole host of technologies are focused on smoothing out the patient journey and administrative workload. Simple but effective tools like automated SMS reminder systems are now widely used to help manage appointments and improve patient follow-through. By cutting down on no-shows and making sure patients remember key instructions, these systems have a surprisingly big impact on both clinic efficiency and health outcomes. Each piece of technology, from complex AI to simple reminders, plays its part in building a more connected and responsive healthcare experience.
The Real-World Gains for Clinics and Hospitals
Let’s move past the theory and talk about what really happens when patient care technology is put to work. For any healthcare organisation, these tools aren't just about looking modern; they're about making tangible improvements to patient health and the financial health of the clinic or hospital. The benefits are felt everywhere, from the front desk staff to the surgical team.
A huge win is the direct impact on patient outcomes. Think of Remote Patient Monitoring (RPM) as a digital safety net. It gives clinical teams the ability to spot a problem long before it turns into an emergency. Imagine someone recovering from heart surgery at home. A simple wearable device tracking their heart rate can flag an irregular rhythm, alerting their doctor to a quick intervention. That single alert could be the difference that prevents a dangerous and expensive trip back to the hospital.
It's a similar story with Clinical Decision Support Systems (CDSS) built right into Electronic Health Records (EHRs). These systems act like a second set of eyes, automatically flagging potential drug interactions or reminding a doctor about a patient's allergy before they hit 'send' on a prescription. This digital co-pilot is brilliant at catching human error, which ultimately leads to safer and more effective care.
The infographic below shows how these core technologies – EHRs, Telehealth, and RPM – don't just exist in silos. They're designed to connect and create a unified system.
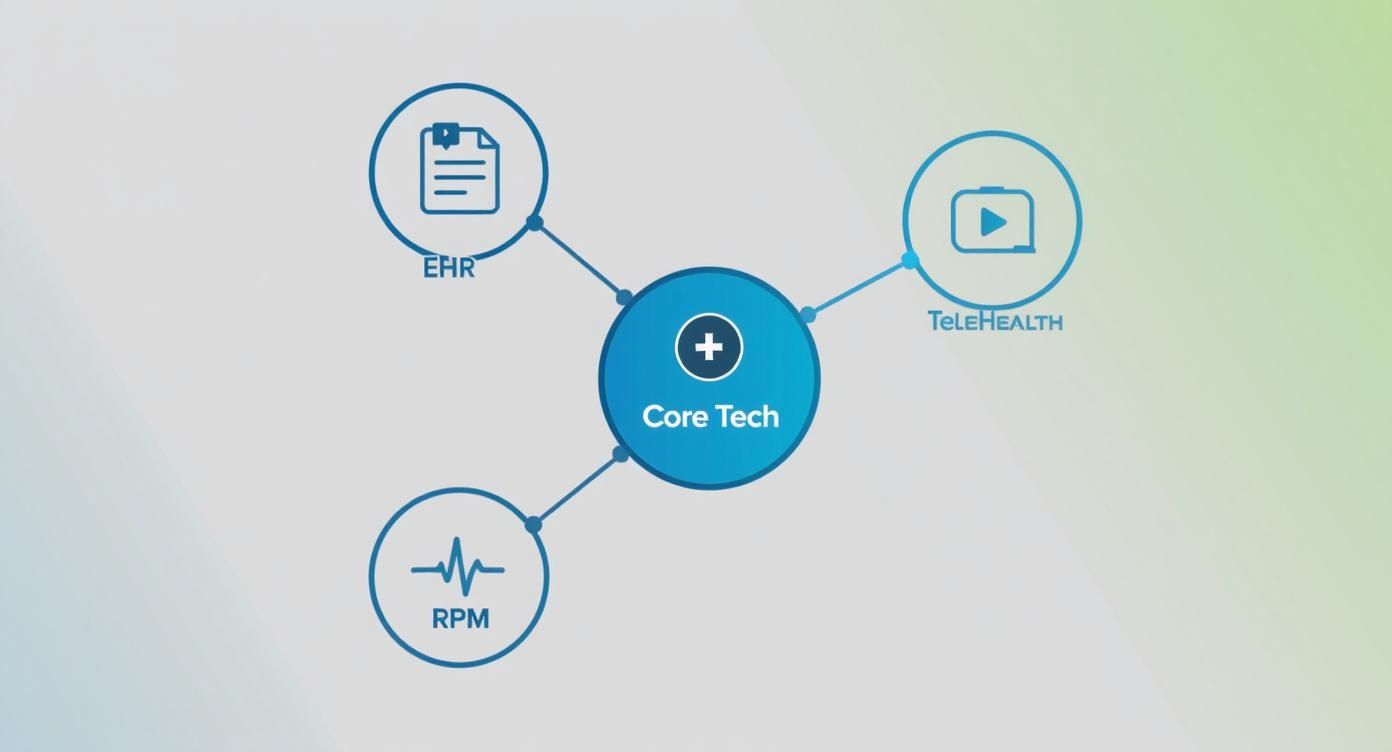
As you can see, while each tool has its own job, their real strength comes from working together. When they're integrated, patient information flows smoothly and securely where it's needed most.
Making Day-to-Day Operations Smoother
Beyond the exam room, patient care technology brings serious efficiency gains to the operational side of things. We all know that administrative work is essential, but it can eat up a massive chunk of a healthcare professional’s day. Automating these repetitive tasks frees up that precious time for what actually matters: caring for patients.
Here’s where you see the biggest boosts in efficiency:
Smarter Scheduling: When patients can book their own appointments online, it drastically reduces phone calls to the front desk and cuts down on simple scheduling mix-ups.
Faster Billing: Automated billing and coding software helps get claims right the first time. This means fewer rejections from insurers and a much faster reimbursement cycle.
Connected Teams: Secure messaging platforms allow doctors, nurses, and specialists to coordinate patient care in real-time without the endless game of phone tag.
These improvements aren't just about saving time; they save money and boost staff morale. When nurses and admin staff aren't bogged down by paperwork, they can focus on the meaningful work that directly helps patients. To see how next-level systems are supercharging operations, you can read more about AI solutions for hospitals in Canada.
Finding Hidden Insights in Your Data
Maybe the most powerful benefit of all is the ability to turn mountains of patient data into truly useful insights. Every appointment, prescription, and lab result logged in an EHR adds to a massive dataset that can be analysed to improve care for everyone.
By using predictive analytics, a hospital can spot trends in patient admissions. This helps them predict staffing needs during flu season or identify which communities are at a higher risk for certain health conditions.
For instance, a local clinic could analyse its data and notice a spike in asthma cases in a particular neighbourhood. This insight could prompt them to launch a targeted air quality awareness campaign. On a much larger scale, researchers can use anonymised data from thousands of patients to figure out which treatment protocols deliver the best results, helping to raise the standard of care across the board.
This data-driven mindset shifts healthcare from being purely reactive to strategically proactive. It allows organisations to get ahead of patient needs, use their resources more wisely, and constantly improve how they do things based on solid evidence. This isn't just about improving one person's health; it's about strengthening the health of entire communities.
Navigating the Common Implementation Hurdles
While the promise of patient care technology is exciting, getting it right is rarely a straight shot. Healthcare organisations often hit some pretty serious speed bumps along the way – hurdles that can stall progress and leave staff feeling frustrated. Knowing what these challenges are from the get-go is the first step toward building a game plan that actually works.
One of the biggest initial hurdles is the price tag. The upfront investment for new software, hardware, and the necessary infrastructure can be substantial. But the costs don’t end after the initial purchase. You also have to account for ongoing maintenance, licensing fees, and the specialised IT support needed to keep everything running smoothly. It all adds up to a complex financial puzzle.
This financial commitment brings up another tough question: what’s the return on investment (ROI)? Unlike a typical business expense, the ROI on this kind of technology isn't just about dollars and cents. How do you put a number on improved patient safety, higher staff morale, or better long-term health outcomes? These gains are incredibly valuable, but they’re notoriously difficult to measure on a balance sheet.
Keeping Patient Data Locked Down
In healthcare, data isn’t just data; it’s deeply personal and legally protected. Securing patient information isn't just a best practice; it's a non-negotiable. A single data breach can have devastating consequences, from massive legal fines and a tarnished reputation to a complete breakdown of patient trust.
This means strictly following regulations like the Personal Information Protection and Electronic Documents Act (PIPEDA) here in Canada, or similar privacy laws globally. But compliance is more than just buying secure software. It demands a true culture of security, which includes:
Rock-Solid Encryption: Data needs to be protected whether it's sitting on a server or moving between systems.
Strict Access Controls: Ensuring only authorised staff can see or change sensitive patient files.
Regular Security Audits: Proactively hunting for weaknesses in your systems and making sure everyone is following security protocols.
If security isn't baked in from day one, a promising tech investment can quickly become a massive liability.
The Fight for System Harmony
Another major technical roadblock is interoperability – a fancy word for getting different systems to talk to each other. Think of it like trying to plug a European appliance into a North American outlet without an adapter. It just doesn't work. It’s the same issue when a hospital’s new electronic health record (EHR) system can't communicate with the local pharmacy's prescription software or a specialist's diagnostic imaging tools.
This disconnect creates "data silos," trapping critical patient information inside one system. When that happens, you lose the complete picture of a patient's health journey. Getting all the pieces to connect seamlessly is the only way to build that comprehensive view.
"True interoperability isn't just a technical goal; it's a clinical necessity. When systems can't communicate, the burden falls on patients and clinicians to manually bridge the gaps, increasing the risk of errors and fragmented care."
The People Problem
Perhaps the most overlooked challenge is the human one. You can have the most brilliant technology in the world, but it’s completely useless if your clinical staff won’t, or can’t, use it effectively. Resistance to change is natural, especially in a high-stakes environment where people have spent years perfecting their workflows.
Staff might worry that new tools will be clunky, slow them down, or even make them feel obsolete. This is exactly why thorough training isn’t a nice-to-have; it's absolutely critical. We see this all the time as healthcare moves toward value-based care. For instance, a recent report on US healthcare found that even when goals are aligned, execution stumbles because of disconnected data strategies and poor staff training. You can read the full report on how tech barriers affect value-based healthcare to see the data.
To make the transition stick, organisations need to do more than just a one-off training workshop. It’s about building confidence, showing how the tech makes a real difference for both staff and patients, and offering continuous support as everyone gets comfortable with a new way of working.
What's Next? Trends Shaping the Future of Healthcare

The world of patient care technology doesn't stand still. New tools and fresh ideas are constantly bubbling up, pushing healthcare to become more predictive, personal, and proactive. These aren't just minor tweaks; we're seeing a real shift in how we think about wellness and disease, bringing care closer to home and making it a whole lot smarter.
Leading the charge is Artificial Intelligence (AI). It's no longer science fiction – AI is here, and it's already making a difference. Think of it as a super-powered analyst, capable of combing through mountains of data to spot patterns a human eye could never catch. This is a game-changer for predictive analytics, where algorithms can flag patients at high risk for issues like sepsis or readmission, giving clinical teams a crucial head start to intervene.
AI isn't just a niche tool anymore; it's going mainstream. In California, for instance, a 2024 report found that 71% of non-federal acute-care hospitals are now using predictive AI built right into their electronic health records. That’s a massive leap in adoption, showing just how deeply these tools are becoming part of the day-to-day work in clinics and hospitals. For more on this, check out these AI adoption statistics in hospitals.
The Rise of Connected Devices
Another huge movement is the growth of the Internet of Medical Things (IoMT). This is all about a web of connected medical devices, sensors, and health monitors that collect and send data in real time. It's like having a digital dashboard of a patient's vital signs that their doctor can check from anywhere.
The IoMT is extending care well beyond the four walls of a clinic. The applications are as practical as they are powerful.
Smart Beds: These aren't just for comfort. They’re packed with sensors that track a patient’s movement, heart rate, and breathing, and can even adjust pressure to prevent bedsores.
Smart Inhalers: For people with asthma or COPD, these devices track when medication is used and can send reminders, which helps with treatment adherence and gives doctors useful data.
Continuous Glucose Monitors: These wearable sensors provide a nonstop stream of blood sugar data for people with diabetes, allowing for better management and fewer complications.
The IoMT turns everyday objects into active partners in a patient's care. This constant flow of data gives clinicians a much clearer, more complete picture of a person's health than a few office visits ever could.
Personalised and Immersive Care
Looking a little further down the road, two other fields are poised to completely change the game: personalised medicine and immersive tech. Personalised medicine, powered by genomics, is all about ditching the one-size-fits-all model. By looking at a patient's unique genetic code, doctors can choose treatments and drugs that are more likely to work well with fewer side effects.
Finally, Virtual and Augmented Reality (VR/AR) are opening up new doors for training and therapy. Surgeons can now rehearse tricky operations in a zero-risk virtual space, while patients can use VR for everything from managing pain to physical rehabilitation. To see just how much is changing, it's worth exploring the future of physical therapy and the role technology is playing. These immersive tools are making healthcare more effective, more engaging, and ultimately, more accessible to everyone.
How to Choose the Right Technology for Your Practice
Picking the right patient care technology isn't about chasing the latest shiny object. It's a strategic move that needs to fit your practice like a glove. The first, most crucial step? A real, honest look at your day-to-day operations.
Walk through your clinic's workflow and find the snags. Are patients getting frustrated with long waits at reception? Is your billing team drowning in paperwork from rejected claims? Pinpointing these specific friction points is everything. It’s how you find a tool that actually solves a problem instead of just adding another layer of complexity to your day.
Once you’ve defined your problems, you can start looking at vendors. But this is so much more than a feature-and-price comparison. You're not just buying software; you're starting a long-term relationship with the company behind it.
Evaluating Potential Technology Partners
A slick sales demo is one thing, but a reliable and secure system is another entirely. Your evaluation needs to go deeper, focusing on factors that ensure the tech can grow with you and keep your patients' data safe.
Here's what should be at the top of your checklist:
Customer Support: When things go wrong, and they sometimes do, how fast and helpful is their team? Look for vendors who provide solid training and are easy to get a hold of.
Security and Compliance: Does the company have a rock-solid security reputation? You have to be absolutely sure they're fully compliant with Canadian privacy laws like PIPEDA.
Scalability: Think about where you want to be in five or ten years. Can this technology keep up, or will you be starting this whole process over again?
A great technology partner should feel like an extension of your team. They should understand the unique challenges of the healthcare environment and be committed to helping you succeed long after the initial sale is complete.
Planning a Smart Implementation
Bringing new technology into your practice requires a careful, phased rollout. If you rush it, you're just asking for frustrated staff and a tool nobody uses. The best way to start is by putting together a team with people from every corner of your practice – clinical, IT, and admin. This makes sure every voice is heard and the solution actually works for the people who will use it every day.
A phased implementation is almost always the smartest route. Introduce the new system one department or one feature at a time. This gives your team a chance to learn and adapt without feeling completely overwhelmed, and it makes it much easier to iron out any kinks along the way. Whether you're building a new system or integrating a ready-made one, a good plan is non-negotiable. If you're considering a bespoke solution, learning about developing custom medical software can offer a clear roadmap for creating a tool that truly fits your unique workflow.
In the end, choosing the right patient care technology is an investment in your practice’s future. By focusing on your real needs, vetting partners thoroughly, and planning a thoughtful rollout, you can find a tool that genuinely empowers your team and helps you deliver better care.
Frequently Asked Questions
It's completely normal to have questions when you're looking into new technology for your clinic or hospital. We get it. Let's walk through some of the most common ones we hear from healthcare professionals just like you.
How Can We Start with a Limited Budget?
Starting small is the key. You don’t need to overhaul your entire system at once. The best first step is to pinpoint your single biggest headache.
Are no-shows costing you a fortune? An affordable, automated SMS reminder service can pay for itself almost immediately. Is billing a chaotic mess? Look for specialised software that can plug into what you’re already using.
Many providers now offer cloud-based tools on a subscription basis. This gets you out of the business of buying and maintaining expensive servers, letting you pay as you go and scale up when the time is right.
What is the Difference Between an EHR and an EMR?
People often use these terms interchangeably, but there's a crucial difference. Think of an Electronic Medical Record (EMR) as a digital version of a patient's old paper chart. It contains their history, diagnoses, and treatments from within one specific clinic.
An Electronic Health Record (EHR) does everything an EMR does, but its real power lies in its ability to be shared securely with other healthcare providers.
An EHR builds a patient's complete health story over their lifetime. It’s a single record that can follow them from their family doctor to a specialist across the country, or even to an emergency room. That ability to connect the dots is what makes care safer and more coordinated.
How Does Technology Improve Patient Safety?
Think of it as a sophisticated safety net. One of its most powerful roles is simply reducing the potential for human error. For instance, automated IV pumps deliver medication at a precise, pre-programmed rate, removing the risk of manual miscalculation. Inside the EHR, Clinical Decision Support Systems (CDSS) act as a second set of eyes, flagging potential drug allergies or harmful interactions before a doctor even finishes writing the prescription.
It also extends your reach beyond the clinic walls. Remote patient monitoring tools can alert your team to subtle changes in a patient's condition at home, letting you step in long before a small problem becomes a full-blown emergency.
What Is the Most Critical Factor for Successful Implementation?
The technology itself is only half the equation. The single most important factor, hands down, is staff buy-in and proper training. If your nurses, doctors, and admin staff don't see how a new system makes their work better and helps patients, they simply won't use it to its full potential. It’ll just become another frustrating task.
A successful rollout means bringing your team into the conversation from the very beginning. It means providing great training, offering ongoing support, and being crystal clear about the "why" behind the change. Ultimately, putting your people first is the only way to make the technology truly work.
At Cleffex Digital Ltd, we build secure, compliant, and intelligent software solutions that empower healthcare providers. Discover how our custom development services can help you solve your biggest challenges by visiting us at https://www.cleffex.com.







