AI-driven EHR solutions are more than just digital record systems; they are intelligent platforms that actively analyze patient data, automate tedious administrative work, and offer predictive insights to clinicians. Think of them less as a storage system and more as a proactive partner in patient care, designed to lighten the load on healthcare professionals and improve outcomes.
From Digital Filing Cabinets to Intelligent Healthcare Partners
For a long time, Electronic Health Records (EHRs) have been little more than digital filing cabinets. They're great for storing a patient's history, but they can be a real headache to sort through. Clinicians often find themselves spending hours digging through records, a manual process that pulls them away from their patients and contributes heavily to burnout.
The shift to AI-driven EHR solutions is changing this entire dynamic. Imagine an EHR that doesn't just hold a lab result but actually understands what it means for that specific patient, flagging a potential drug interaction or identifying someone at high risk for a chronic condition. It can even listen to a doctor-patient conversation and draft the clinical notes automatically. This is the real evolution—from a passive database to an active, intelligent assistant.
The Driving Force Behind AI Adoption
The demand for smarter healthcare tools has reached a critical point. Clinician burnout and staff shortages are serious problems, especially in large, complex health systems. Healthcare professionals are crying out for technology that can slash their administrative burden so they can focus on what they were trained to do: care for patients.
This isn't just wishful thinking; the enthusiasm for AI is real. A recent survey showed that 81.63% of physicians and 78.79% of administrators are eager to bring AI tools into their practices. Their top reasons are incredibly practical:
Reducing the crushing administrative workload (52.38%)
Making EHR management less of a chore (47.61%)
Improving the accuracy of diagnoses (41.90%)
This tells us something important: AI in healthcare has moved beyond a futuristic buzzword. It's now seen as a real-world solution to today's most urgent problems. You can dig deeper into these trends by reading the full AI trends in healthcare report.
The chart below breaks down exactly where healthcare leaders see AI making the biggest difference.

It’s clear the focus is on practical applications that make daily workflows more efficient and accurate. The goal is to finally transform the EHR from a simple record-keeper into a proactive partner that helps deliver better care.
Decoding the Technology Behind AI-Powered EHRs

To really get why AI-driven EHR solutions are such a big deal, we need to pop the hood and look at the engines making them run. It helps to think of these systems less as a single program and more like a well-oiled team of digital experts, each bringing a special skill to the table.
This team works in concert, transforming what used to be a static, digital filing cabinet into an active partner in patient care. Each piece of the puzzle is vital for understanding data, anticipating clinician needs, and taking over tedious tasks. The end goal? Giving healthcare professionals back their most precious commodity: time.
Machine Learning: The Digital Diagnostician
The brain of any smart EHR is Machine Learning (ML). Picture a veteran doctor who’s seen it all over a decades-long career. They’ve developed an almost sixth sense for spotting subtle patterns that hint at a bigger problem, often long before it becomes an emergency.
That's essentially what Machine Learning does, but on a superhuman scale. It sifts through immense, anonymised patient datasets—everything from lab work and imaging reports to doctors' notes—to find hidden connections a person could never spot.
Here’s what that looks like in practice:
Predicting Patient Risk: By learning from past cases, an ML model can flag a patient who is at high risk for developing sepsis or being readmitted, allowing the clinical team to step in early.
Personalising Treatment Plans: It can suggest which treatments worked best for other patients with a nearly identical genetic makeup and lifestyle.
Optimising Hospital Operations: ML can even predict patient admission waves, helping hospitals schedule staff and allocate resources more effectively.
This predictive power is what fundamentally changes the EHR's role. It moves from being a reactive record of what happened to a proactive tool that helps maintain health and prevent illness.
Natural Language Processing: The Expert Transcriber
So much of a patient's real story is buried in unstructured text, the detailed notes a doctor dictates after a visit, a specialist’s consultation report, or the discharge summary. A standard EHR can hold this text, but it can’t make sense of it. That’s where Natural Language Processing (NLP) comes in.
NLP is the technology that lets a computer read and understand human language. In an AI-powered EHR, NLP is like having an expert transcriber who doesn't just type but also understands the context, pulling structured, useful data out of messy, free-form notes.
This technology is a game-changer for cutting down the documentation grind. Instead of clunky drop-down menus and endless typing, NLP can instantly pull key information like symptoms, medications, and diagnoses directly from a doctor’s spoken or written words.
This means a physician can just have a normal conversation with their patient, and the EHR drafts a structured clinical note in the background, ready for a quick review. It's a massive time-saver, but it also captures a much richer and more accurate patient story.
Generative AI: The Efficient Assistant
The newest player on the team is Generative AI. If Machine Learning is the diagnostician and NLP is the transcriber, think of Generative AI as the super-efficient assistant who handles all the paperwork and follow-up.
Working with the clean, structured data provided by ML and NLP, Generative AI can create entirely new content. This is incredibly useful for automating both clinical and administrative tasks. For example, it can automatically:
Draft a referral letter to a specialist.
Write a patient-friendly summary of a complex treatment plan.
Generate the first draft of an insurance pre-authorisation request.
When these technologies work together, they create a powerful engine for the modern EHR. And as we consider the technical side, it's impossible to ignore the need for specialized cloud hosting for healthcare. These systems require immense data storage and processing power, and a secure, compliant hosting environment is the foundation they're built on. This combination is what makes an AI-driven EHR more than just a piece of software—it’s an intelligent partner in delivering better care.
How AI Features Actually Change Clinical Workflows
It’s one thing to talk about the tech behind AI-driven EHR solutions, but the real magic happens when you see how these features play out in a busy clinic or hospital. We're not talking about futuristic concepts; these are practical tools that are already tackling some of the biggest headaches in healthcare.
The core idea is to flip the script. For years, clinicians have had to bend their workflows to fit the rigid structure of their EHR software. AI-powered features do the opposite—they adapt to the clinician. This is where the real change begins, turning the EHR from a data-entry burden into a genuinely helpful assistant. The goal is simple: let the machines handle the repetitive stuff so the experts can focus on what they do best: caring for patients.
Intelligent Clinical Documentation
Ask any physician about their biggest frustration, and clinical documentation will likely top the list. It's a huge source of burnout. The endless typing, clicking, and checking boxes after every single patient visit eats up a staggering amount of time.
This is where intelligent documentation comes in, and one of the most powerful examples is ambient listening technology. Picture this: a doctor is having a normal, face-to-face conversation with a patient. In the background, an AI system is quietly listening, transcribing their chat, and then automatically populating a structured clinical note. No more turning your back to the patient to type.
The benefits here are immediate and obvious:
Massive Time Savings: That 20 or 30 minutes of after-hours "pajama time" spent catching up on notes? It shrinks to a quick review and a single click to sign off.
Better, More Accurate Notes: The AI captures the full conversation, often leading to richer, more detailed notes than what a clinician might recall and type up later.
A Return to Real Doctor-Patient Connection: Doctors can finally maintain eye contact and truly engage with their patients, not their keyboards.
This image shows just how stark the difference is between the old way of doing things and a workflow supported by AI.
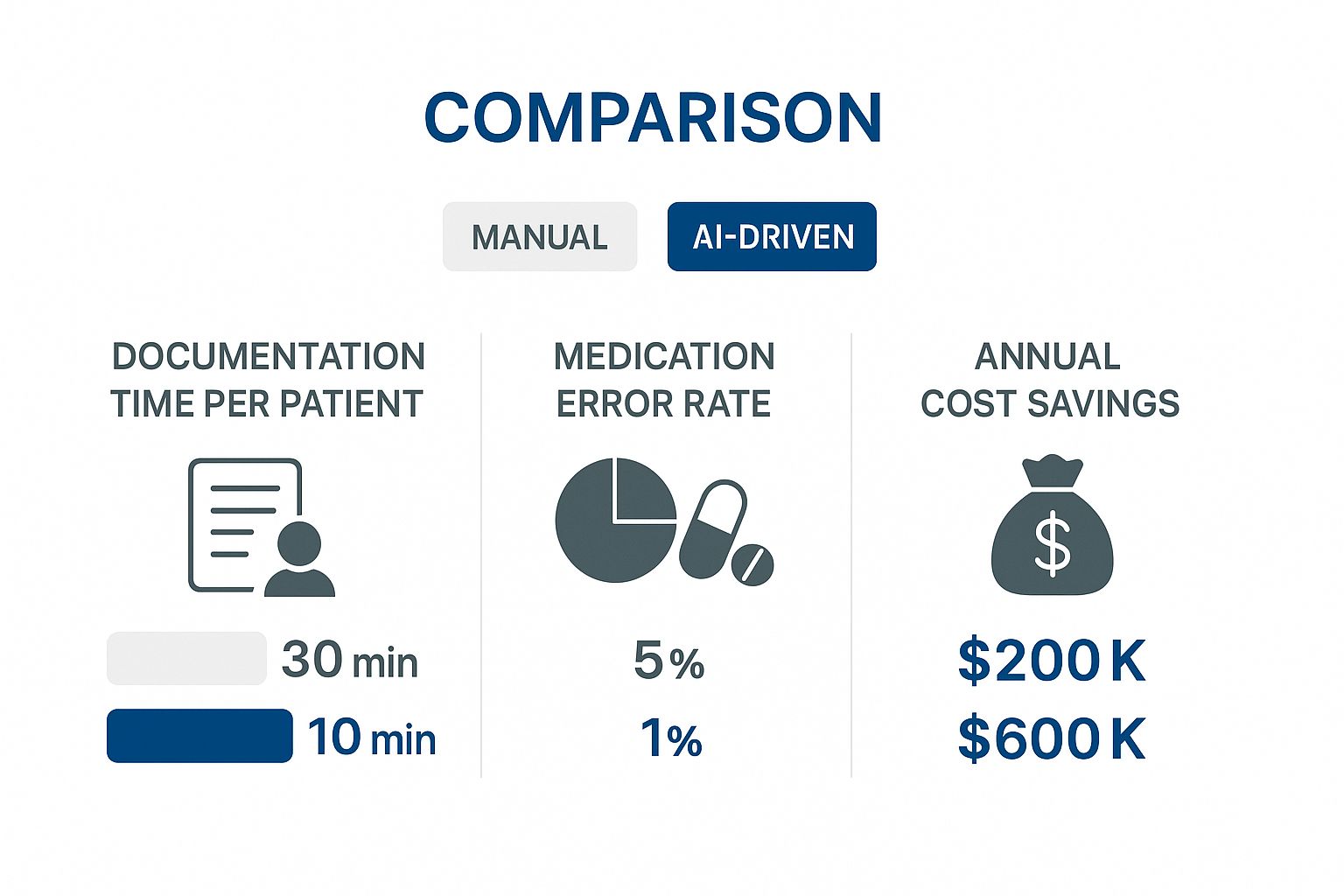
As you can see, the improvements in speed, safety, and even the bottom line are pretty dramatic.
To truly appreciate the leap forward, it helps to see a direct comparison. Here’s a look at how standard EHR features stack up against their AI-enhanced counterparts.
Comparing Traditional EHR vs AI-Driven EHR Features
Feature Area | Traditional EHR Capability | AI-Driven EHR Capability |
|---|---|---|
Clinical Documentation | Manual data entry, template-based notes | Ambient listening, automated note generation, voice-to-text |
Decision Support | Basic alerts based on simple rules (e.g., drug allergies) | Predictive risk scoring, personalised treatment suggestions |
Data Analysis | Manual queries, basic reporting dashboards | Proactive identification of at-risk patient cohorts, trend analysis |
Administrative Tasks | Manual medical coding, template-based billing | Automated coding suggestions from clinical notes, revenue cycle optimisation |
Patient Scheduling | Manual booking, simple calendar views | Predictive scheduling to minimise no-shows, optimised resource allocation |
This table makes it clear that AI doesn't just add a few new bells and whistles. It fundamentally upgrades the core purpose of the EHR, moving it from a passive record-keeper to an active, intelligent partner in care delivery.
Predictive Analytics for Proactive Care
For the most part, healthcare has always been reactive. We wait for a problem to show up, and then we treat it. AI-driven EHRs are helping to change that by using predictive analytics to spot trouble long before it becomes a full-blown crisis. Think of it as a sophisticated early warning system for your entire patient population.
The system crunches thousands of data points, like lab results, vital signs, medication history, and even social determinants of health, and its machine learning models find subtle patterns that a human could easily miss. This allows care teams to step in early and prevent a costly hospital stay or a serious health decline. If you want to dive deeper into the mechanics, you can learn more by reading our guide on predictive healthcare with AI.
It's about seeing the bigger picture. An AI might connect a slight dip in a patient's kidney function with a new prescription and their recent missed appointments to predict a high risk of readmission—a connection that's tough to make in the moment.
This shift to proactive care isn't just better for patients; it's also a much smarter way to use healthcare resources. You can focus your efforts on the people who need it most, right when that intervention will have the greatest impact.
Automated Administrative Tasking
Beyond direct patient care, there's a mountain of administrative work that keeps a healthcare organisation running: scheduling, medical coding, billing, and more. While essential, these tasks are repetitive and a breeding ground for human error, which can lead to denied claims and compliance headaches.
AI-driven EHR solutions are exceptional at automating these workflows. For example, once a clinical note is signed, an AI tool can scan the text, instantly identify the procedures and diagnoses, and suggest the correct billing codes. This doesn't just get claims out the door faster; it dramatically improves coding accuracy and reduces denials.
It's the same story with scheduling. AI can analyse historical data to predict no-shows and automatically optimise the appointment calendar to keep the clinic running smoothly. By lifting these administrative burdens, the entire team, from clinicians to front-desk staff, is freed up to focus on more meaningful, patient-centred work. That’s a win for efficiency and a huge boost for morale.
Navigating the Realities of Implementation

Bringing an AI-driven EHR solution into your healthcare practice is a major move. While the payoff can be huge, the path to get there is lined with some very real-world challenges. This isn't just a simple software update; it's a fundamental shift in your team's day-to-day workflow.
To pull this off successfully, you need a clear-eyed plan. Think of it like mapping out a major expedition. You wouldn't just start walking into the wilderness. You'd chart your course, get your team on board, and make sure you have the right gear. The same level of foresight and planning is absolutely essential here.
Overcoming Data Interoperability Hurdles
Let’s be honest: one of the first and biggest headaches you'll face is data interoperability. Your patient information is likely scattered everywhere, such as in lab systems, billing platforms, and old EHRs. Each system speaks its own digital language, and an AI can't generate meaningful insights from data it can't understand.
This is where data standards like Fast Healthcare Interoperability Resources (FHIR) become your best friend. FHIR essentially acts as a universal translator, enabling all your different systems to finally talk to each other.
Adopting FHIR isn't just about ticking a technical box. It’s the foundational move that creates a single, unified view of a patient’s journey, which is what allows the AI to do its best work.
Without that cohesive data stream, your shiny new AI-EHR is effectively working with one hand tied behind its back. Making interoperability a day-one priority is non-negotiable.
Mastering Change Management and Staff Training
You can have the most brilliant technology in the world, but it’s useless if your staff won’t use it. If your clinical team sees the new system as a burden or, worse, a threat to their autonomy, you're headed for failure. This makes change management just as crucial as the technology itself.
Getting buy-in from your team starts with clear, honest communication. They need to understand the why behind the change, not just the what. Frame the conversation around the benefits that will actually make their lives easier, such as:
Spending less time on paperwork and more time with patients.
Getting smarter clinical decision support that works like a helpful co-pilot.
Cutting down the administrative grind, which means less after-hours charting and burnout.
Effective training is also key. Forget the one-off, overwhelming session. Plan for phased training that lets people build skills and confidence over time. A great strategy is to identify and train a few "super-users" in each department who can then provide on-the-ground, peer-to-peer support. For more on this, our guide on developing custom medical software digs into the importance of user-focused design.
Addressing the Digital Divide
While many hospitals and clinics have gone digital, a significant gap still exists, especially in more specialised care sectors. This "digital divide" can stop an AI-driven EHR from reaching its full potential. You have to have a solid IT foundation in place before layering on advanced AI.
A recent assessment of California's health IT landscape really brings this issue to light, particularly in behavioral health and social services. Even though the HITECH Act pushed EHR adoption forward, many providers in these critical areas still don't have the basic digital tools needed to exchange data. This creates a huge barrier to providing holistic care and getting the most out of AI.
The data clearly show that while hospital adoption rates are high, other crucial facilities, like mental health and substance use treatment centres, are lagging far behind. It’s a stark reminder that to truly unlock the power of AI in healthcare, we first need to ensure the entire care continuum is on a solid digital footing.
Upholding Trust with Ethical and Compliant AI
In healthcare, technology is only as good as the trust it inspires. This is especially true for AI-driven EHR solutions. We're not just talking about managing data here; these systems touch sensitive patient lives. That makes governance, ethics, and compliance the absolute bedrock of their design.
For these intelligent tools to become true partners in patient care, they have to operate within a strict ethical framework. It’s about actively embedding the core principles of responsible AI. Without that commitment, even the most powerful technology can undermine the very patient-provider relationship it’s supposed to strengthen.
The Pillars of Responsible AI in Healthcare
Building an AI-powered EHR you can trust means focusing deliberately on three critical areas. These aren't just buzzwords; they are the principles that ensure technology serves clinical needs without ever compromising patient safety or a clinician's judgment.
Fairness and Equity: An AI model is a reflection of the data it learns from. A responsible system is constantly checked to find and fix biases that might lead to unfair care recommendations for certain groups of people.
Transparency and Explainability: Clinicians need to understand why an AI suggests a particular diagnosis or treatment. "Black box" algorithms simply don't belong in healthcare. The system has to offer clear, logical reasons to support human decision-making.
Accountability and Oversight: The AI is there to assist, not replace, the clinician. The final call must always belong to a licensed professional. This keeps technology in its proper place as a tool and maintains clear lines of accountability for patient outcomes.
The goal is to preserve clinical autonomy. An AI-driven EHR should feel like a trusted advisor offering data-backed insights, not an unchallengeable authority dictating care. Striking that balance is crucial for both provider adoption and patient safety.
Navigating the Regulatory Landscape
Beyond ethical design, following privacy laws is non-negotiable. Regulations are changing fast to keep up with technology, placing strict compliance demands on both healthcare organisations and their tech vendors. A big part of maintaining trust and compliance is having solid security, which is why understanding the role of Artificial Intelligence in enhancing cybersecurity for businesses is so important.
California, for example, is getting ahead of the curve on AI governance in health. The state's Assembly Bill 3030, which takes effect in 2025, requires that any generative AI used for patient communication must be reviewed and documented by a licensed provider. This really cements the principle of clinical accountability and shows the growing focus on making sure AI is a safe, reliable tool in the healthcare world.
A Framework for Evaluating Vendors
When you're looking for an AI-driven EHR partner, you have to ask the right questions to see how serious they are about ethical and compliant AI. Don't get distracted by flashy features; dig into their governance practices. For a broader look at this topic, you might want to read our deep dive into ethics and AI in healthcare.
Here are a few key questions to put to any potential vendor:
How do you source your training data, and what's your process for auditing it for potential biases?
What do you have in place to make sure your AI's recommendations are explainable to clinicians?
How does your system's design guarantee that human oversight remains central to every clinical workflow?
Can you show us your documentation proving compliance with all relevant privacy and security regulations?
Choosing a vendor who puts these principles first means you’re not just buying software. You’re investing in a technology partner who is as dedicated as you are to protecting the trust that is so fundamental to patient care.
Calculating the Real Return on Your AI Investment
When you’re thinking about investing in an AI-driven EHR solution, the initial price tag is only one small part of the story. The real value isn't just about getting new software; it’s about seeing tangible improvements ripple across your entire organisation. To build a solid business case, you need to measure the return on investment (ROI) across three critical areas: financial, clinical, and operational.
This mindset shifts the whole conversation. Instead of asking, "How much does it cost?", we start asking, "How much value will it create?" By breaking down the benefits this way, you can build a compelling case that ties the technology directly to your core mission: delivering excellent patient care as efficiently as possible.
Measuring the Financial Gains
The most straightforward place to start is with the financials. AI is incredibly good at finding and fixing the administrative waste and inefficiencies that quietly drain resources. These systems can take over manual tasks, leading to immediate cost savings and more accurate revenue capture.
To get a clear picture, start by tracking these key performance indicators:
Reduced Administrative Costs: Think about all the time your staff spends on medical coding, billing, and processing claims. AI automation can slash that time, meaning fewer person-hours are needed for back-office work. That’s a direct saving.
Improved Billing Accuracy: When AI suggests medical codes based on clinical notes, you cut down on human error and, consequently, claim denials. Even a 5-10% reduction in denial rates can have a massive impact on your revenue cycle.
Faster Reimbursement Cycles: Cleaner claims get submitted faster, which means you get paid by insurers sooner. This directly improves your organisation's cash flow.
Think of it this way: the AI system isn't just another cost centre. It’s an engine for revenue cycle optimisation. It actively works to plug financial leaks that many have just accepted as a standard cost of doing business in healthcare.
Quantifying Clinical and Operational Improvements
While the financial gains are a huge selling point, the real power of an AI-driven EHR is how it improves patient outcomes and makes daily operations smoother. These benefits can sometimes be harder to stick a dollar value on, but they're absolutely fundamental to the long-term success of your practice.
Focus on tracking how things improve in these areas:
Better Patient Outcomes: Start watching metrics like lower hospital readmission rates or better management of chronic conditions for specific patient groups. These are direct signs that proactive, AI-guided care is making a real difference.
Increased Clinician Capacity: When AI handles the grunt work of documentation and administrative tasks, clinicians get valuable time back. That reclaimed time means they can see more patients or spend more meaningful time with each one, which is a win for both productivity and quality of care.
Higher Staff Retention: Clinician burnout is a massive, expensive problem. A primary driver of that burnout is the crushing administrative burden. By easing that load, an AI-powered system can genuinely improve job satisfaction and lower staff turnover, saving a fortune in recruitment and training costs down the line.
Common Questions We Hear About AI in EHRs
As healthcare leaders start looking into AI-powered EHRs, some very practical questions and real concerns always come up. This is a big shift, after all, and you need straight answers. Let's walk through some of the most common questions we get asked to help clear things up as you weigh your options.
Getting a handle on these points is key for anyone trying to steer their organisation through this transition. We'll get into the reality of what it takes to implement these systems, how patient data is kept safe, and what this all means for your most important asset: your people.
Will AI Replace Our Clinicians or Medical Staff?
This is probably the number one question on everyone's mind, and the answer is a firm no. The whole point of AI in a clinical setting is to augment, not replace. Think of it as the most capable assistant you've ever had; the one that’s built to take on the tedious, data-intensive tasks that bog down your team and lead to burnout.
AI is fantastic at automating routine work, like drafting initial clinical notes or sifting through mountains of data to flag potential patient risks. This frees up your clinicians to focus on what they were trained to do: handle complex patient cases, apply their critical thinking skills, and build the human connection that is, and always will be, at the heart of medicine.
The real goal of AI in an EHR is to empower your human experts, not make them redundant. By shouldering the administrative load, AI lets your clinical team work at the very top of their licence.
How Secure is Patient Data in an AI System?
Protecting patient data is non-negotiable. Reputable AI-EHR solutions are built on a bedrock of security, using things like end-to-end encryption and strict access controls to lock down sensitive information. These systems are designed from day one to meet and exceed demanding privacy laws.
On top of that, the best platforms take a "privacy-first" approach when training their AI models. This means your specific protected health information (PHI) is never used to teach the core AI, keeping that data completely separate and ensuring you stay compliant. When you’re vetting vendors, make sure they can show you a clear, unwavering commitment to data protection.
What Does the Implementation Process Actually Look Like?
Bringing an AI-powered EHR into your practice is a journey, not a flip of a switch. A smart implementation is almost always done in phases to make the transition as smooth as possible and get everyone on board. You're not looking at a sudden, all-at-once changeover.
Typically, the process kicks off with a smaller pilot program in one department or clinic. This controlled start lets your organisation:
Demonstrate Value: You can show real, tangible benefits early on, which helps build momentum and excitement.
Refine Workflows: It’s the perfect time to find and fix any hitches in your processes on a smaller scale.
Gather Feedback: You can get direct input from users to help shape the training and support for the full rollout.
This deliberate approach, often spanning several months, is the best way to manage change and lay the groundwork for a successful, organisation-wide adoption down the road.
At Cleffex Digital Ltd, we specialise in developing secure, compliant, and user-friendly AI-driven solutions that empower healthcare providers. Discover how our custom software can transform your clinical workflows.