Imagine your clinical staff finally being free from mountains of paperwork. Picture your administrative team running like a well-oiled machine. This isn’t a distant dream; it's what AI automation for healthcare makes possible today. It works like a dedicated digital partner, handling the repetitive tasks and sifting through data so your team can focus on what truly matters: patient care.
Putting AI to Work in Your Clinic or Hospital
AI is no longer a sci-fi concept. It’s a practical, down-to-earth tool that helps medical practices deliver better care and stay ahead of the curve. It cuts through the hype to offer real answers to some of healthcare’s biggest headaches, from staff burnout to frustrating operational delays.
Think of it less as a replacement for human skill and more as a way to amplify it.

By taking over routine processes, AI gives your team back its most precious asset: time. That means more time for meaningful patient conversations, deeper diagnostic thinking, and a healthier, more sustainable work environment for everyone.
The Growing Momentum Behind Healthcare AI
The adoption of AI in medicine is picking up speed, and for good reason. In Canada alone, the market for artificial intelligence in healthcare hit a value of USD 163.8 million, a clear sign of serious growth fuelled by automation.
This number shows that Canada is becoming a real centre for healthcare AI innovation, attracting clinics and startups looking for reliable, secure solutions. What’s more, the sector is forecast to grow at a strong 8.8% compound annual growth rate from 2025 to 2035. You can dig deeper into these market trends to see the full picture.
This momentum is all built on AI's power to deliver results you can actually measure. It’s not just about being faster; it’s about fundamentally improving the way we deliver care.
For clinics and hospitals, AI automation is the key to shifting from constantly putting out fires to proactively managing care. It gives your teams the data-backed insights they need to see patient needs coming and allocate resources smartly – before problems even start.
A Practical Roadmap for Your Organisation
This guide will walk you through how to understand and bring AI automation for healthcare into your own practice. We’ll break down the big ideas into simple, clear steps and show you exactly how these systems can fit into your day-to-day operations.
We’ll cover:
Optimising Clinical Workflows: Learn how to lift the administrative weight off your medical staff’s shoulders.
Streamlining Administrative Tasks: Discover better ways to handle billing, scheduling, and communicating with patients.
Enhancing Diagnostic Accuracy: See how AI can act as a valuable partner in clinical decision-making.
By the end, you'll have a clear understanding of how different AI-powered healthcare solutions can directly help your patients, your staff, and your practice’s financial health.
How AI Is Modernising Daily Healthcare Operations
Let's move past the theory and look at what AI automation for healthcare is actually doing on the ground, right now. These aren't far-off concepts; they are practical tools already changing the day-to-day reality in clinics and hospitals. Instead of replacing human expertise, AI is acting as a powerful assistant, handling the repetitive or data-heavy lifting so professionals can dedicate their time to what truly matters: patient care.

This shift is happening fast. Here in Canada, the interest from healthcare businesses in AI automation is booming. The number of organisations planning to adopt it has more than doubled, jumping from 11.4% to an expected 23.2% by Q2 2025. According to Statistics Canada, that’s the steepest climb of any industry, showing a clear move toward automating everything from patient scheduling to remote monitoring.
To get a clearer picture of where AI is making the biggest waves, here’s a quick summary of its key applications.
Key AI Automation Applications in Healthcare
| Application Area | Example Use Case | Primary Benefit |
|---|---|---|
| Clinical Workflows | AI-driven scheduling that predicts no-shows; automated clinical note generation from conversations. | Reduced patient wait times, less physician burnout, and more time for patient-facing activities. |
| Administrative Tasks | Automated insurance claim processing and eligibility verification; intelligent billing and coding. | Faster revenue cycles, fewer claim denials, and reduced administrative overhead. |
| Diagnostics & Treatment | AI analysis of medical images (X-rays, MRIs) to flag anomalies; personalised treatment plan suggestions. | Improved diagnostic accuracy, earlier disease detection, and a move toward precision medicine. |
| Remote Monitoring | Continuous analysis of data from wearable devices to detect health changes and alert care teams. | Proactive management of chronic conditions, prevention of emergencies, and reduced hospital admissions. |
These examples show how AI isn't just one thing; it's a collection of specialised tools designed to solve specific problems across the entire healthcare spectrum. Now, let's explore each of these areas in more detail.
Optimising Clinical Workflows
One of the most immediate impacts of AI is felt right in the clinic, where it helps manage the flow of patients and information much more smoothly. It’s all about cutting out the wasted time and bottlenecks that frustrate everyone.
Imagine a scheduling tool that does more than just fill empty slots. It could analyse a doctor’s availability, a patient’s medical history, and even local traffic patterns to find the best appointment time. The result? Fewer no-shows and shorter waits.
Then there’s the mountain of paperwork. Doctors spend hours every day on documentation, a huge source of burnout. Tools like AI-powered documentation solutions can listen to a patient visit and automatically generate a perfect, structured summary for the electronic health record (EHR). That one change can give a physician back hours every week.
Streamlining Administrative Task Automation
The administrative side of healthcare is full of repetitive, rules-based work – a perfect fit for automation. AI is a game-changer here, handling huge volumes of tasks with incredible speed and accuracy. This frees up staff to focus on more complex patient needs and financial discussions.
Take insurance claims, for instance. AI algorithms can:
Instantly check a patient's eligibility and coverage details.
Scan claims for common mistakes or missing information before they're submitted.
Automate the submission and follow-up process, slashing denial rates.
This not only improves the organisation’s financial health but also lets the administrative team provide better, more personal support to patients instead of chasing down paperwork.
By automating the back-office, healthcare organisations not only cut operational costs but also reduce the friction that often frustrates both patients and staff. The result is a smoother, more transparent experience for everyone involved.
Advancing Diagnostics and Treatment Pathways
In a clinical setting, AI acts like a second set of expert eyes. It helps clinicians spot subtle patterns in complex data, like medical images or genetic information, at a speed no human could match.
For example, an AI algorithm trained on thousands of X-rays can highlight a tiny area of concern that might be overlooked, flagging it for a radiologist's review. The AI doesn’t replace the radiologist; it makes their expertise even more effective and accurate.
AI models can also analyse a patient's unique genetic profile, lifestyle, and medical history to suggest personalised treatment options. This is a huge step away from the old one-size-fits-all model and toward precision medicine built for the individual.
Enabling Proactive Remote Patient Monitoring
With the rise of smartwatches and other wearable devices, we have a constant stream of health data. But who has time to monitor it all? This is where AI automation for healthcare is incredibly powerful.
AI systems can analyse data from these devices 24/7, tracking things like heart rate, blood glucose, or sleep patterns. If the AI spots a reading that strays from a patient's normal baseline, it can automatically alert the care team.
This allows for intervention before a small issue becomes a big one – often before the patient even feels symptoms. It’s a fundamental change from reactive to proactive care, helping people manage chronic conditions better and avoid costly trips to the emergency room.
Calculating the Real Value of Healthcare AI
When you're looking at any major investment, the first thing you ask is, "What's the return?" For AI automation in healthcare, the answer goes way beyond just saving a few dollars. The true value comes from a blend of three key areas: a healthier bottom line, better patient care, and a more sustainable workplace.
To really see the return on investment (ROI), you have to look past the initial price tag. It's about measuring the real-world benefits that spread throughout your entire organisation – the gains in efficiency, clinical results, and the satisfaction of both your patients and your staff.
Boosting Operational Efficiency
The most straightforward financial win from AI is making your day-to-day operations much sharper and more accurate. Think about all those repetitive administrative tasks. They are perfect for automation, which immediately frees up your team's time and slashes the risk of expensive human errors.
Take the revenue cycle, for instance. AI systems can process insurance claims, check patient eligibility, and manage billing at a speed that's simply not humanly possible. This kind of automation drastically cuts down on claim denials, which can cost a typical practice thousands of dollars every single month. The result? A more predictable and faster flow of revenue, with a lot less time wasted on paperwork.
This newfound efficiency directly impacts labour costs. Staff who were once bogged down with administrative work can now shift their focus to more meaningful activities, like handling complex patient questions or coordinating care.
Driving Better Clinical Outcomes
Operational savings are great, but the clinical value of AI is where you'll see the most meaningful impact. When AI tools help with diagnostics and treatment planning, they directly contribute to better patient health, which carries its own significant financial benefits.
For example, AI algorithms that scan medical images can spot diseases like cancer earlier and with greater accuracy. Catching these conditions early often means less invasive, less costly treatments and a huge improvement in patient survival rates. This doesn't just save lives; it also cuts the long-term cost of care that comes with treating advanced illnesses.
AI is a game-changer for identifying patients at high risk of being readmitted. By flagging these individuals for proactive follow-up, hospitals can bring down their readmission rates – a critical metric for both quality of care and avoiding financial penalties.
Getting the most out of this requires turning patient data into real-world insights. You can dig deeper into this by exploring comprehensive healthcare data analytics solutions designed to support these clinical goals.
Improving Patient and Staff Experience
A great experience for patients and staff isn't just a "nice-to-have"; it's the bedrock of a successful, growing practice. AI automation helps create a better environment for everyone by smoothing out the bumps and reducing daily frustrations.
For patients, this translates into real improvements they can feel:
Shorter Wait Times: Smart scheduling systems organise appointment flows, meaning less time spent flipping through old magazines in the waiting room.
Personalised Communication: Automated, tailored reminders and follow-ups help patients stay engaged and on top of their care plans.
Quicker Answers: AI-powered chatbots can handle common questions instantly, letting staff focus on more pressing needs.
For your team, the biggest win is a massive reduction in burnout. Automating the monotonous stuff lets clinicians and administrators focus on the rewarding, human side of their jobs. A happier, more engaged team means lower staff turnover and higher productivity – both of which directly support your organisation's financial stability. When you put a smart AI strategy in place, higher patient retention and a motivated team are the clear results.
Navigating Healthcare Data Privacy and Compliance
Bringing new technology into a healthcare setting always sparks a crucial conversation about security. And when you're dealing with something as deeply personal as patient health information, trust isn't just important; it's everything. This is why getting a firm grasp on the regulatory landscape is step one for any practice thinking about AI automation for healthcare.
Thankfully, we aren't starting from scratch. Robust data privacy frameworks are already in place to protect patient information. These regulations aren't roadblocks to progress; think of them as the guardrails that ensure technology serves patients safely and ethically. Understanding these rules is the foundation for building patient confidence.
Understanding the Core Privacy Frameworks
For any healthcare provider, particularly here in Canada, a few key regulations really set the standard for data protection. While they might have different origins, they all share a common mission: to keep patients in control of their own health information.
You can think of these frameworks as a digital version of the "do no harm" oath, making sure that every piece of patient data is handled with the highest degree of care.
PIPEDA (Personal Information Protection and Electronic Documents Act): This is the cornerstone of federal privacy law in Canada. It dictates how private-sector organisations, including clinics, can collect, use, and share personal information. In simple terms, it means you need clear consent from patients before you gather their data, and you can only use it for the reason you stated.
HIPAA (Health Insurance Portability and Accountability Act): While HIPAA is an American law, its influence is felt globally. It has become the gold standard for protecting sensitive patient health information. Many Canadian practices that work with U.S.-based patients or partners will follow its strict guidelines for things like data encryption and access controls.
GDPR (General Data Protection Regulation): This regulation from the European Union has a long reach. If your practice offers services to anyone who is an EU citizen, even through a telehealth appointment, you need to comply with its demanding rules on data consent, transparency, and the "right to be forgotten."
At the heart of all these laws is a simple truth: patient data belongs to the patient. Your organisation is simply a custodian, and you've been entrusted with protecting it. Getting this wrong can lead to heavy financial penalties, but even worse, it can permanently break the trust you've built with your patients.
How Reputable AI Partners Build in Compliance
A responsible AI partner doesn't just bolt on compliance features at the end. Instead, they weave security and privacy into the very fabric of their technology right from the start. They get that for AI automation for healthcare to truly work, it must be secure by design.
This commitment to security is a non-negotiable, and it involves several key practices. For a deeper dive into how these principles are applied, check out our guide on AI in healthcare data privacy in Canada.
Top-tier AI vendors use a multi-layered security strategy, with technical safeguards working quietly in the background to keep every byte of data safe.
Key Security Measures in Compliant AI
End-to-End Encryption: This is a fundamental security measure. It essentially scrambles patient data the moment it’s entered, making it completely unreadable to anyone without the right key. It's like sending a message in a locked box that only the intended recipient can open.
Data Anonymisation: Whenever possible, AI models are trained on data that has been de-identified. This process strips out personal details like names, addresses, and health card numbers, so the algorithm can learn from the medical information without ever linking it back to a specific person.
Strict Access Controls: Not everyone in your clinic needs to see every piece of patient information. A well-designed AI system uses role-based access, meaning staff can only see the specific data they need to perform their duties – nothing more.
Secure Cloud Infrastructure: Leading AI providers rely on certified, healthcare-compliant cloud platforms. These data centres are protected by world-class physical and digital security, and they undergo regular, independent audits to prove they are up to the task.
If you want to see what this looks like in practice, you can review Recepta.ai's Privacy Policy for a real-world example of how a company communicates its commitment to data protection. With the right technology partner and the right safeguards in place, you can bring AI into your practice with confidence, knowing that innovation and patient privacy can and absolutely must go hand in hand.
Your Step-by-Step AI Implementation Plan
Bringing AI into your healthcare organisation feels like a huge undertaking, but it doesn't have to be. The secret is to treat it less like a massive tech overhaul and more like a clinical trial for your own operations. You start with a focused goal, measure the results carefully, and then scale what works.
This roadmap breaks the journey down into four manageable phases. It’s designed to guide you from initial curiosity to full-scale implementation, making sure each step builds logically on the last. The goal is a smooth transition that delivers real value without ever disrupting patient care.
Before we dive in, let's establish the bedrock of any AI initiative in healthcare: data privacy. The principles shown below: encryption, consent, and access control, must be built into every stage of your plan.
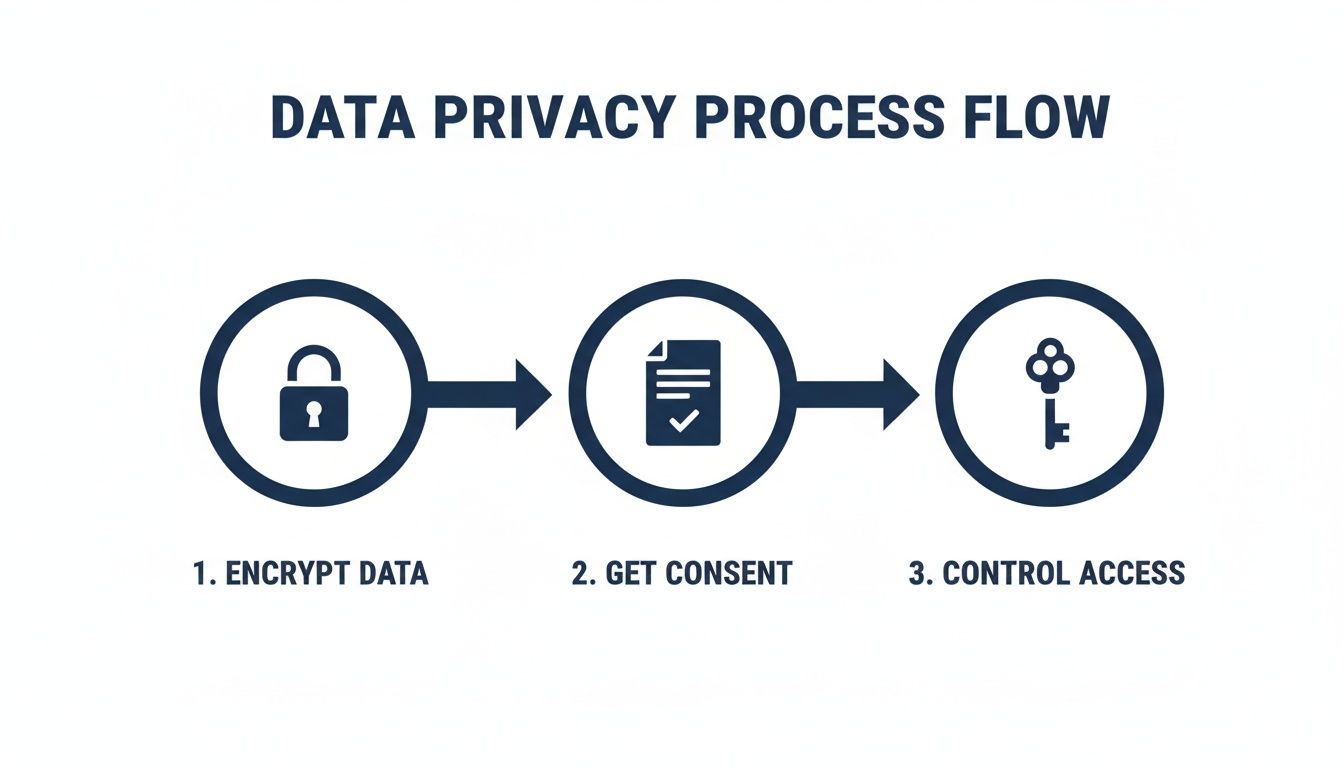
Think of this as your non-negotiable foundation. Without an unwavering commitment to privacy, even the most promising AI strategy is destined to fail.
Phase 1: Assessment and Strategy
Before you look at a single piece of software, you need to look inward. This first phase is all about discovery – finding the best opportunities for AI within your existing workflows. You’re hunting for the "low-hanging fruit," those repetitive, time-sucking tasks that are ripe for improvement.
Start by mapping out your daily operations. Where are the bottlenecks? What jobs consistently lead to staff burnout or human error?
A few common starting points include:
Administrative Overload: Are your front-desk staff buried in appointment reminders and insurance eligibility checks?
Documentation Burden: How many hours do your clinicians lose to writing and finalising notes after each patient visit?
Revenue Cycle Delays: Are simple billing errors and claim denials choking your cash flow?
By zeroing in on these high-impact areas, you can build a focused strategy. The aim isn't to automate everything at once. It’s to pick one, well-defined problem that AI can solve decisively, delivering a quick and visible win that gets your whole team on board.
Phase 2: The Pilot Program
Once you have a clear target, it’s time to launch a pilot program. This is your chance to test an AI solution on a small, controlled scale. You get to prove its value and gather essential feedback before committing to a full rollout. A successful pilot builds internal support and gives you the hard data needed to make a confident, organisation-wide decision.
For example, if documentation is your biggest headache, you could trial an AI-powered note-generation tool with a small group of clinicians for 90 days. During that time, you'll need to track specific, measurable outcomes.
The entire purpose of a pilot is to answer one question with data: Does this technology actually make a meaningful difference to how we work? It shifts the conversation from "what if" to "here's how."
This controlled test keeps risks low and gives your team a chance to get comfortable with the new technology in a low-pressure setting. It’s also the perfect time to spot any integration challenges or training gaps early on.
Phase 3: Integration and Training
With a successful pilot in the bag, the next step is integration. This is where the technical details come into play. Your new AI tool needs to connect seamlessly with your existing systems, especially your Electronic Health Record (EHR). The connection has to be flawless; the AI should feel like a natural extension of your workflow, not another clunky program to manage.
This is where your choice of implementation partner becomes absolutely critical. Whether you build a solution in-house or work with a specialist, you need a team that can navigate the technical complexities and ensure your AI tool talks perfectly to your EHR and other software.
Just as important is staff training. A tool is only as good as the people using it. Great training should be focused on:
Practical Skills: Showing teams how to use the tool in real, day-to-day scenarios.
Highlighting Benefits: Clearly explaining how the AI will reduce their workload and free them up to focus on patients.
Building Confidence: Offering ongoing support and creating a space where questions are encouraged.
When your staff feels empowered to use the new tools effectively, you unlock the true potential of your investment in AI automation for healthcare.
Phase 4: Validation and Monitoring
Here’s a crucial point: implementation is not the finish line. The final phase is a continuous loop of validation and monitoring. You need to make sure the AI solution is delivering on its promise and look for ways to make it even better. This means consistently tracking the key performance indicators (KPIs) you set back in the pilot phase.
Are you seeing that reduction in documentation time you were hoping for? Have your claim denial rates dropped? Are fewer patients missing their appointments?
Regularly reviewing these metrics allows you to quantify your return on investment (ROI) and build a powerful business case for expanding AI into other areas of your practice. This data-driven approach keeps your AI strategy locked on your core goals, turning your initial project into a long-term strategic advantage.
Choosing Your AI Implementation Partner
Deciding whether to build your AI solution from scratch or partner with an outside expert is a major decision. An in-house team offers deep institutional knowledge, but an external specialist brings focused expertise and experience from multiple implementations.
The table below compares these two paths to help you weigh the pros and cons for your organisation.
| Consideration | In-House Development | Outsourcing to a Specialist (e.g., Cleffex) |
|---|---|---|
| Expertise & Resources | Relies on existing team's skillset; may require new hires or extensive training. | Access to a dedicated team of AI and healthcare integration experts. |
| Speed to Implementation | Often slower due to learning curves, resource allocation, and competing priorities. | Faster deployment, leveraging pre-built components and proven methodologies. |
| Cost | High upfront investment in salaries and infrastructure; ongoing maintenance costs. | Typically a project-based or subscription fee; more predictable costs. |
| Focus | Internal team may be pulled into other IT projects, diluting focus. | The partner's sole focus is on delivering and supporting your AI solution. |
| Risk | Higher risk if the project fails to deliver; all development costs are sunk. | Lower risk; partners often have performance guarantees and established track records. |
Ultimately, the right choice depends on your organisation's resources, timeline, and risk tolerance. For many clinics and hospitals, partnering with a specialist like Cleffex provides the fastest, most reliable path to achieving a strong ROI from their AI initiatives.
Real-World Examples of AI in Action
It's one thing to talk about AI in theory, but it’s another to see it working in the real world. The best way to grasp the power of AI automation in healthcare is to look at how it's solving everyday problems for organisations big and small. These aren't just hypotheticals; they're stories of clinics, hospitals, and startups finding smarter ways to work.
Let’s walk through a few examples, looking at the challenge they faced, the AI tool they brought in, and the results they saw.
A Small Clinic Tackles Patient No-Shows
The Problem: A busy family practice was dealing with a frustratingly high number of no-shows. These empty appointment slots didn't just mess with the daily schedule; they also hit the clinic's bottom line. Their front-desk staff were spending a huge chunk of their day making manual reminder calls, which pulled them away from helping patients who were actually in the clinic.
The Solution: They brought in an AI-powered scheduling and reminder tool. Instead of just blasting out generic messages, this system looked at each patient's history to figure out the best way to remind them, whether by text or email. It even got smart enough to predict which patients were most likely to cancel, giving staff a heads-up to reach out personally.
The Outcome: The results were impressive. In just six months, the clinic cut its no-show rate by 30%. This simple application of AI automation for healthcare gave the front-desk team their time back, letting them focus on what matters most: the patient experience.
A Regional Hospital Gets Diagnostic Results Faster
The Problem: The radiology department at a mid-sized regional hospital was drowning in diagnostic images. The sheer volume meant it was taking longer and longer to get reports back to doctors, which in turn delayed treatment plans and left patients anxiously waiting.
The Solution: The hospital decided to bring in an AI platform that could assist with analysing medical images. This AI worked side-by-side with the radiologists, scanning X-rays and CTs to quickly flag areas that needed a closer look. Think of it as a highly trained assistant that never gets tired, helping to prioritise the most urgent cases and pointing out subtle details that the human eye might miss on a busy day.
This isn't about replacing the expert radiologist. It's about augmenting their abilities, allowing them to interpret images faster and with greater confidence, directly accelerating the path to patient care.
The Outcome: With the AI's help, the department sliced its report turnaround time in half. Even better, follow-up audits revealed a noticeable improvement in diagnostic accuracy. It was a clear win, proving that AI can boost both the speed and the quality of care.
A Startup Uses AI to Predict Health Events
The Problem: A health-tech startup had a great idea: a remote monitoring service for patients with chronic conditions. The challenge was figuring out how to make sense of the constant flood of data coming from wearable devices. They needed a way to spot the early warning signs of a health problem before it became an emergency.
The Solution: They built their platform around an AI engine designed to learn each patient's individual health patterns. The system continuously tracked data points like heart rate variability, sleep patterns, and activity levels. Its job was to look for tiny deviations from a person's baseline that could signal trouble ahead.
The Outcome: The AI model worked. It successfully identified patients at risk of a health crisis, giving their care teams a chance to step in before things got serious. This breakthrough helped the startup secure its next round of funding and forge partnerships with major healthcare providers, demonstrating that AI is key to moving from reactive to genuinely proactive care.
Your Questions About AI in Healthcare, Answered
When new technology comes on the scene, it's natural to have questions. Getting straight answers about how AI automation really works in a healthcare setting is the first step toward making a smart decision for your practice. Here are a few of the most common questions we get from clinics, hospitals, and health-tech startups.
We've kept the answers direct and practical to give you the clarity you need to move forward.
Is AI Automation Affordable for Smaller Practices?
Yes, absolutely. It's a common myth that AI is a tool reserved for massive hospital networks with deep pockets. The reality is that many of the best AI solutions today are built on scalable, subscription-based models. This means you avoid a huge upfront investment and only pay for what you actually use.
The key to seeing a return on your investment (ROI) is to start small and specific. Pinpoint a single, costly problem. For instance, figure out exactly how much staff time is spent each year on manual appointment reminders, or calculate the revenue you're losing from denied insurance claims. An AI tool focused on solving just one of those problems can often pay for itself in a matter of months.
Will AI Replace Doctors and Nurses?
In a word, no. The goal of AI in a clinical environment isn't to replace your team's expertise; it's to support it. It's best to think of AI as an incredibly efficient assistant. It takes on the repetitive, data-heavy tasks that contribute to burnout, which frees up your clinical staff to focus on what humans do best: complex problem-solving, showing empathy, and delivering hands-on care.
AI is brilliant at spotting patterns in massive amounts of data and automating tedious administrative tasks. It's like a tireless partner, making sure clinicians have the best information and more time to actually care for their patients.
At the end of the day, AI actually enhances the human side of medicine by getting rid of the administrative headaches that stand in the way of meaningful patient conversations.
How Do We Ensure AI Is Ethical and Unbiased?
This is one of the most important conversations to have when it comes to AI in healthcare. Building fair and ethical AI begins with the data used to train it. A responsible technology partner will make it a priority to use diverse and representative datasets that mirror your actual patient population. This is the single most effective way to minimise bias from the start.
Beyond the data, transparency is non-negotiable. An ethical AI system shouldn't be a "black box." It should be auditable and, wherever possible, provide clear reasons for its recommendations. It's crucial to partner with vendors who are committed to constantly monitoring their algorithms to find and fix biases as they emerge.
What Is the Single Best First Step to Get Started?
The best place to begin is with a simple workflow audit. Don't try to solve every problem at once. Instead, identify the single biggest bottleneck or source of frustration in your day-to-day operations. Is it patient scheduling? Clinical documentation? The billing cycle?
Once you’ve pinpointed that one specific pain point, you have a perfect target for your first AI project. This focused approach makes it much easier to choose the right tool, run a successful pilot program, and show your team a clear, measurable win right out of the gate.
Ready to find the perfect starting point for AI automation in your practice? Cleffex Digital Ltd specialises in developing secure, compliant, and scalable AI solutions designed for the unique challenges of the Canadian healthcare sector. We can help you conduct a workflow audit and build a clear roadmap for success. Learn more about our custom healthcare software solutions.







