When you hear "AI in hospital management," don't picture robots replacing doctors and nurses. The reality is far more practical and powerful. It’s about providing your healthcare teams with intelligent tools that can anticipate needs, streamline complex operations, and ultimately enhance patient care. Think of it as a strategic partner that helps untangle the immense complexity of modern healthcare delivery.
What Is AI in Hospital Management

Picture an air traffic control system, but for a hospital. It doesn't just track patient movements; it anticipates bottlenecks in the ER, reroutes staff to where they’re needed most, and helps ensure every patient journey is as seamless as possible. That’s the essence of artificial intelligence in hospital management. It pushes past simple automation into a proactive, data-fueled environment where every decision is smarter and more efficient.
Instead of constantly reacting to problems like bed shortages or long wait times, AI systems help administrators get ahead of them. By digging into historical data and processing real-time information, these platforms can forecast patient admission rates, predict which medical supplies will run low, and build optimal staff schedules weeks in advance. This kind of foresight is a game-changer for operational stability.
A Strategic Partner for Better Outcomes
AI’s true value is in augmenting human expertise, not trying to replace it. It does the heavy lifting, sifting through mountains of data, which frees up clinicians and administrators to focus on what they do best: applying critical judgment and providing empathetic patient care.
This partnership makes the entire healthcare system more responsive and resilient. For a deeper look at its impact across the industry, you can explore the wider applications of artificial intelligence in healthcare.
AI becomes not just an enabler, but I believe it is going to accelerate our ability… to advance our safety model using these high-impact, cross-industry, safety practices.
This kind of strategic collaboration fundamentally changes the day-to-day reality of running a hospital. The benefits ripple out across the entire organisation, empowering every team to deliver exceptional care more consistently.
Core Functions of AI in Hospital Management
The applications are incredibly diverse, but most of them fall into a few key areas that tackle the most common operational headaches. These intelligent systems are built to:
-
Predict and Plan: By analysing past trends, AI can forecast everything from patient flow and resource demand to potential disease outbreaks in the community.
-
Optimise and Allocate: Whether it's operating theatre schedules or nurse staffing levels, algorithms can pinpoint the most efficient way to use limited resources.
-
Support Clinical Decisions: AI tools can analyse patient data to flag potential risks or suggest diagnostic pathways, giving clinicians an extra layer of support right at the point of care.
-
Automate Administrative Tasks: Routine work like medical billing, coding, and inventory tracking can be automated, which cuts down on errors and frees up countless hours.
How AI Transforms Hospital Operations

So, how does AI in hospital management actually work on the ground, beyond the theoretical concepts? It’s about giving practical solutions to the persistent, day-to-day headaches that administrators and clinicians know all too well. These tools aren’t meant to be disruptive overhauls; they're designed to slot into existing workflows, sharpening efficiency, easing staff burnout, and putting a real dent in operational challenges.
The fundamental idea is simple: automate what's predictable and analyse what's complex. This frees up your highly skilled people to focus on the human side of care: the parts of the job that require judgment, empathy, and quick thinking. It’s about making your data work for you, not the other way around.
Let's look at the real-world applications making this happen.
Streamlining The Patient Journey
Right from the moment a patient walks through the door, AI can start smoothing out their experience. The emergency department (ED) is a perfect example, often the most chaotic centre of a hospital, where these tools can deliver an immediate, noticeable impact.
AI-powered triage systems are a game-changer here. By analysing a patient’s symptoms, vitals, and medical history in seconds, these algorithms can flag high-risk individuals much faster and more consistently than manual checks. This means the people who need critical care get it sooner, reducing the risk of them deteriorating in the waiting room. Pilot programs have shown this can cut wait times by up to 30%.
But the improvements don't stop at the ED. Intelligent scheduling tools use predictive analytics to manage everything from appointments and surgical theatre bookings to outpatient clinics. By forecasting demand and juggling variables like procedure duration and surgeon availability, these systems create dynamic schedules that minimise downtime for expensive equipment and slash wait times for patients.
Optimising Resource and Supply Chain Management
A hospital runs on logistics. Having the right people, equipment, and supplies in the right place at the right time is everything. AI is incredibly good at solving this complex puzzle.
-
Intelligent Staffing: Instead of just reacting to a busy ward, AI models can look at patient census data, acuity levels, and historical trends to predict staffing needs ahead of time. This helps create balanced schedules that avoid both understaffing (which burns out nurses) and overstaffing (which drains the budget).
-
Automated Inventory Control: Forget manual stocktakes. AI-driven systems monitor supply usage in real time, predicting when you’ll run low on critical items like medications or PPE and automatically placing orders. This prevents the kind of stockouts that can delay patient care.
-
Operating Theatre Efficiency: Sophisticated algorithms can optimise surgical schedules by analysing case complexity, equipment requirements, and surgeon availability. This ensures that every valuable minute of operating theatre time is used effectively, allowing more procedures to be completed safely.
By constantly analysing operational data streams, AI delivers a level of foresight that’s simply impossible with traditional methods. It shifts the entire management approach from reactive problem-solving to proactive, intelligent planning.
Enhancing Clinical and Administrative Support
Beyond the logistical side, AI also acts as a powerful assistant for both clinical and administrative staff, freeing them up to focus on what matters most.
Here is a quick look at some of the most impactful applications making a difference in hospitals today.
Key AI Applications in Hospital Operations
| AI Application | Problem Addressed | Primary Benefit |
|---|---|---|
| Predictive Triage | Inconsistent, slow patient assessment in emergency departments. | Faster identification of high-risk patients, reduced wait times. |
| Intelligent Scheduling | Inefficient use of operating theatres and clinical resources. | Maximised resource utilisation, fewer scheduling conflicts. |
| Supply Chain Automation | Manual inventory tracking leading to stockouts or over-ordering. | Prevention of critical shortages, reduced waste, lower costs. |
| Clinical Decision Support | Clinician overload, risk of missed diagnoses or drug interactions. | Data-backed clinical insights, improved patient safety. |
| Automated Billing & Coding | Time-consuming, error-prone manual medical coding. | Faster reimbursement cycles, increased billing accuracy. |
| AI Voice Scribes | Extensive administrative burden from clinical documentation. | Reduced clinician burnout, more time for direct patient care. |
These tools aren't just about efficiency; they directly support better clinical outcomes and a healthier work environment for staff.
Clinical Decision Support (CDS) systems are a prime example. Think of them as a data-savvy second set of eyes. These tools scan a patient's electronic health record (EHR) to flag potential drug interactions, suggest possible diagnoses based on symptoms and lab work, or identify patients at high risk for conditions like sepsis. It doesn’t replace a doctor’s expertise; it strengthens it.
On the admin front, AI is tackling some of the most tedious tasks. Natural Language Processing (NLP) tools can read a clinician's notes and automatically generate the correct medical codes for billing, a process that is notoriously slow and prone to error. This not only speeds up the reimbursement cycle but also frees up staff to handle more complex claims. You can see a great example of this in how an AI voice assistant revolutionising healthcare operations can drastically cut down on documentation time.
Taken together, these applications chip away at the administrative burden that contributes so heavily to burnout across the healthcare sector.
The Financial Case for AI in Canadian Healthcare
When we talk about bringing AI into hospital management, it's easy to focus on the operational side of things. But for hospital executives and financial officers in Canada, the conversation quickly turns to the bottom line. Investing in AI isn't just a tech upgrade; it’s a strategic financial decision with a clear and measurable return on investment (ROI). It's about shifting from simply improving how things are done to driving real cost reductions and ensuring long-term financial health.
By having AI take over routine tasks and untangle complex workflows, hospitals can directly address some of their biggest expenses. These aren't just small adjustments, either. They open up major opportunities for savings that can be funnelled right back into patient care, vital research, and staff development.
Driving Major Cost Reductions
One of the first places you see a financial impact is in how resources are managed. Think about operating theatres – incredibly expensive assets that need to be used effectively. AI-powered scheduling systems can boost their utilisation by 15-20%, making sure every minute counts. The same logic applies to inventory; predictive AI can stop you from either tying up capital in overstocked supplies or paying a premium for emergency orders when you run short.
Then there's the mountain of administrative work. Automated medical coding and billing systems are a game-changer. They cut down on human error, which means fewer rejected claims and much faster reimbursement cycles. An application like this can easily recover thousands of dollars each month that would otherwise disappear due to simple clerical mistakes.
In the Canadian healthcare landscape, AI is unlocking massive cost-saving potential, particularly in hospital management, where efficiency is paramount. A detailed McKinsey analysis found that deploying AI at scale across public health and care delivery could generate net annual savings of CA $14 billion to CA $26 billion for the system.
Reducing The High Cost of Patient Readmissions
Patient readmissions are a massive financial headache for any hospital. They’re often preventable and lead to high, unbudgeted costs. This is where predictive analytics really shines.
AI models can sift through a patient's electronic health record, demographic information, and even social determinants of health to pinpoint who is at high risk of coming back soon after discharge. By flagging these individuals, care teams can step in before a problem arises.
This could mean:
-
Creating personalised discharge plans with tailored follow-up care.
-
Arranging targeted post-discharge support, like home care visits or telehealth check-ins.
-
Using AI-powered tools to help with medication adherence monitoring.
Every single readmission that's prevented saves the system thousands of dollars. This makes predictive analytics one of the strongest arguments for AI investment. To dig deeper into the direct economic benefits, it’s worth reviewing specific AI use cases in Health Economics and Outcomes Research.
Gaining a Strategic Competitive Edge
The financial case for AI isn't just about cutting costs today; it’s about securing a stronger position for tomorrow. In a competitive environment, especially when it comes to attracting top medical talent, being an early adopter of advanced technology makes a huge difference.
Clinicians want to work in places that give them tools to be more effective and reduce their administrative burden. A hospital that invests in AI is sending a clear signal that it’s committed to innovation and supporting its people. That makes it a far more attractive workplace for sought-after specialists, nurses, and researchers.
Beyond staffing, a reputation for efficiency and excellent patient outcomes is invaluable. When wait times are shorter and care is better coordinated, patient satisfaction scores go up. That strengthens the hospital’s standing in the community and among referring physicians, building a foundation for sustained growth. For a broader look, check out our guide on the benefits of AI in Canadian healthcare.
Ultimately, the financial argument is a powerful one. It covers everything from immediate operational savings and reduced readmission costs to the long-term strategic advantage of becoming a leader in the field.
Untangling the Technical and Regulatory Knots
Bringing AI into your hospital's operations isn't just about picking the right software. It's a careful walk through a maze of technical hookups and strict rules. To get it right, you need to handle data with care, make sure new systems can talk to your old ones, and follow Canada's tough laws on patient privacy.
Think of these challenges less as roadblocks and more as essential checkpoints. Tackling them head-on from the start ensures your AI tools are not only smart but also secure, compliant, and trustworthy.
Laying a Foundation with Strong Data Governance
Data is the fuel for any AI system, and in health care, that data is incredibly personal. Before you can even think about launching an algorithm, your hospital needs a bulletproof data governance framework. This isn't just a job for the IT department; it’s the bedrock of patient trust and ethical AI.
Think of data governance as the constitution for your hospital's data. It creates clear rules for:
-
Data Quality: Making sure the information going into the AI is accurate and complete. Bad data in means bad or even dangerous results out.
-
Access Control: Locking down who can see or use sensitive patient data, and for what specific reasons.
-
Data Lineage: Keeping a clear record of where data came from, how it was changed, and where it went. This creates an audit trail you can always rely on.
Without these ground rules, even the most sophisticated AI can churn out results you can't trust.
Protecting Patient Privacy and Staying Compliant with PIPEDA
In Canada, protecting patient information isn’t just good practice; it's the law. The Personal Information Protection and Electronic Documents Act (PIPEDA) sets the rules for how organisations handle personal data. For any hospital using AI, following these rules is non-negotiable.
This means every AI solution has to be built with privacy baked in from the start. Patient data should be anonymised or de-identified whenever possible, and strong encryption must shield it, whether it's sitting on a server or moving across the network.
A single data breach can shatter a hospital's reputation and bring on massive fines. Every AI project has to be viewed through a privacy lens to ensure it meets or, better yet, exceeds what the law requires.
Getting a handle on these legal duties is a must. To dig deeper, you can learn more about the specifics of AI in healthcare and data privacy in Canada in our detailed guide.
Solving the Interoperability Puzzle
One of the biggest headaches you'll face is interoperability. In simple terms, this is about getting your new AI system to talk seamlessly with your hospital's existing tech, especially your Electronic Health Record (EHR). The EHR is your hospital's central hub, holding nearly all critical patient information.
An AI tool that can't communicate with your EHR is basically a fancy, expensive paperweight. It leads to isolated pockets of data, forces your staff into clunky manual workarounds, and completely misses the mark on making things more efficient. It’s like buying a high-tech appliance only to get it home and find out it has a plug that doesn't fit any of your outlets.
The key is to partner with vendors who know their way around major EHR systems. They should be fluent in standard data formats like HL7 or FHIR, which act as universal languages to ensure information flows smoothly and securely.
Making Sense of the Regulatory Approval Process
Finally, many AI tools, especially those that help with clinical decisions or diagnostics, are considered medical devices. That means they need a green light from regulatory bodies before they can be used.
In Canada, Health Canada is the gatekeeper. The approval process is all about proving the AI model is both safe and effective for what it's designed to do. This involves intense validation, crystal-clear documentation of how the algorithm performs, and a solid plan for keeping an eye on it after it's launched. Getting through this process takes real expertise, so it's a critical factor to consider when you're choosing a partner.
Your AI Implementation Roadmap
Bringing AI into your hospital operations can feel like a huge undertaking. The key is to break it down. Think of it less as a single, massive tech project and more as a series of deliberate, strategic steps. For hospital leaders, this isn't just about buying new software; it's about guiding a fundamental shift in how your facility operates.
A well-structured plan is what separates a successful initiative from a stalled one. It helps you move from theory to real-world results, one phase at a time, minimising risks and building momentum along the way. The objective is to implement solutions that genuinely solve the everyday problems your staff face.
Phase 1: Assess Your Data and Infrastructure
Before you can even think about AI models, you have to look at the fuel they run on: your data. This first phase is all about a frank assessment of your hospital’s data ecosystem. Are your electronic health records (EHRs) clean and well-organised? Is the patient data you hold accurate, complete, and most importantly, accessible?
Think of it like laying the foundation for a new building. If that foundation is weak or cracked, anything you build on top of it will be unstable. This audit needs to identify any gaps in data quality and flag technical roadblocks, like legacy systems that will make integration a nightmare.
Phase 2: Start Small with a Pilot Program
Don’t try to boil the ocean. Instead of a massive, hospital-wide overhaul, the smartest approach is to begin with a focused pilot project. Pinpoint a single, high-impact problem where AI can deliver a clear, measurable win.
Good candidates for a pilot often include:
-
Optimising operating theatre scheduling to cut down on expensive idle time.
-
Automating inventory management for a specific category of high-use supplies.
-
Rolling out an AI-powered triage tool in one department, like the emergency room.
A successful pilot does more than just prove the technology works; it creates internal champions. When your staff see a tool directly improving their day-to-day workflow, they become the best possible advocates for wider adoption.
This method lets you test, learn, and adjust your strategy on a manageable scale. It gives you invaluable insight into what actually works within your hospital’s unique culture, setting you up for success when it’s time to scale up.
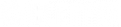
The infographic below shows the common hurdles you'll need to clear, from wrangling data to navigating regulatory approval.
As you can see, the technical work is just one piece of a much larger puzzle that has data security and compliance embedded from start to finish.
Phase 3: Master Change Management and Staff Adoption
Technology doesn't create change – people do. The most critical part of any AI in hospital management roadmap, and the one that’s easiest to get wrong, is change management. Your clinicians, nurses, and admin staff are the ones who will use these tools every day. If they aren't on board, the project is doomed.
Get them involved from the very beginning. Ask them about their biggest operational headaches. Include them when you're selecting and designing the pilot programs. It's absolutely crucial that your team sees AI as a helpful tool, not as a threat or another frustrating system they're being forced to learn.
Effective change management really comes down to three things:
-
Clear Communication: Constantly explain the "why" behind the new technology. Focus on the benefits that matter to them, like less paperwork and more time to focus on patient care.
-
Comprehensive Training: Provide hands-on, role-specific training that actually builds confidence. Make sure everyone knows exactly how to use the new tools in the context of their job.
-
Feedback Loops: Create simple ways for staff to give feedback, report issues, and suggest improvements. When you act on that feedback, it proves you're listening.
By making your staff active partners in this journey, you can turn natural resistance into genuine enthusiasm. It stops feeling like a top-down mandate and becomes a collaborative effort to build a better, more efficient hospital for everyone.
Choosing the Right AI Technology Partner
Picking the right technology vendor is probably the single most important decision you'll make on your entire AI in hospital management journey. The success of your project hangs on more than just a clever algorithm; it depends entirely on the expertise, reliability, and strength of the partner you bring on board. This isn't just about buying software; it's about building a strategic, long-term relationship.
A vendor might show up with flashy tech, but if they don’t have a deep understanding of the healthcare world, their solutions will almost certainly fall flat. You need a partner who speaks the same language as your clinicians and administrators, who gets the tangled workflows of a hospital, and who truly respects the massive responsibility that comes with handling patient data.
Look Beyond the Technology
When you're vetting potential partners, their technical skills are just the price of entry. What really sets the great ones apart is their specific experience within the Canadian healthcare system. A vendor with a proven history of building secure, compliant solutions is non-negotiable for navigating our country’s tight regulatory environment.
You should be looking for partners who can show you:
-
Deep Healthcare Domain Expertise: They need to understand the real-world operational headaches, from patient flow in the emergency department to the nuances of clinical documentation.
-
A Proven Track Record in Compliance: Ask them for concrete examples of how their solutions meet Canadian privacy laws like PIPEDA. They should be able to walk you through their security protocols with total confidence.
-
A Collaborative Development Approach: The best partners work with you, not just for you. They should be eager to get your clinical and admin staff in the room from day one, making sure the final product actually solves the problems your team is facing.
A true technology partner doesn't just sell you a product; they invest in your outcomes. They understand that their success is directly tied to the measurable improvements their AI brings to your hospital's efficiency and patient care.
This kind of collaborative spirit is what ensures the solution is practical and, more importantly, actually gets used by the frontline staff who need it most.
Critical Questions to Ask Potential Vendors
To cut through the marketing fluff and find a genuine partner, you need to ask sharp, specific questions. Your mission is to get a crystal-clear picture of their technical chops, their security posture, and their commitment to you for the long haul.
Walk into every meeting with a checklist of must-ask questions. This simple framework will help you compare your options apples-to-apples and make a decision based on what really matters in a healthcare setting.
Here are a few non-negotiable questions to get you started:
-
Data Security and Privacy: How exactly do you ensure all patient data is encrypted, both when it's stored and when it's moving? Can you walk me through your specific protocols for PIPEDA compliance and data anonymisation?
-
Model Validation and Performance: What methods do you use to prove your AI models are accurate and fair? How do you keep an eye out for algorithmic bias or performance degradation after the system goes live?
-
Integration Capabilities: What’s your track record integrating with major EHR systems like Cerner or Epic? Can you share case studies of successful integrations with hospital systems similar to ours?
-
Post-Launch Support and Training: What does your support model look like? If we have a technical problem, who does my team call? What kind of training do you offer to make sure our staff can actually use these new tools effectively?
Finding a partner who can answer these questions with confidence and transparency is everything. They aren't just a supplier; they’re a co-author of your hospital's future success.
Common Questions About AI in Hospitals
Even with the clearest plan, it’s natural for hospital leaders to have some tough questions before diving into an AI strategy. Getting these concerns out in the open is the best way to build the confidence your team needs to move forward successfully. Let's tackle some of the most common things that come up when discussing AI in hospital management.
Our goal here is to pull back the curtain on the technology. We want to provide clear, straightforward answers that help your team see AI not as another complex hurdle, but as a practical tool for making daily operations and patient care better.
Will AI Replace Doctors and Nurses in Our Hospital?
This is easily the most frequent question, and the answer is a firm no. The role of AI in any clinical setting is augmentation, not replacement. These tools are built to take on the repetitive, data-intensive tasks that bog down staff and contribute to burnout.
It’s best to think of AI as a highly capable assistant. It can sift through mountains of data to help inform a clinical decision or automate routine paperwork, freeing up your talented medical professionals. This gives them more time to focus on what they do best: providing hands-on patient care and making the complex, human judgments that technology can't.
Is AI Implementation Affordable for Our Budget?
The notion that AI is reserved for huge, deep-pocketed institutions just isn't true anymore. Today, many leading AI solutions are offered through a Software as a Service (SaaS) model, which dramatically lowers the cost of entry. Instead of a massive upfront investment, you're looking at a more predictable, subscription-style cost.
The smartest way to begin is to start small. Pinpoint a single, high-impact problem, maybe it's optimising your surgical scheduling or tackling patient readmission rates, where you can see a clear and quick return on investment (ROI). A successful pilot project gives you solid proof of value, making it far easier to get the green light from leadership for a broader, phased implementation.
How Do We Ensure Patient Data Remains Secure and Private?
Protecting patient data isn't just a priority; it's non-negotiable. It’s the very foundation of patient trust and a strict legal obligation under Canadian regulations like PIPEDA.
Any AI partner you consider must have proven, deep expertise in healthcare compliance and data security. There are a few essential safeguards you should expect as standard:
-
Robust Data Encryption: Patient data must be encrypted at all times, whether it's sitting on a server or being transmitted.
-
Strict Access Controls: Access to sensitive information should be granted on a need-to-know basis, tied directly to a person's role.
-
Data Anonymisation: Where feasible, data should be de-identified to strip out personal details and protect patient privacy.
-
Regular Security Audits: The system's defences need to be constantly monitored and audited to stay ahead of new threats.
Ultimately, your AI platform needs to be built with a "privacy by design" mindset, ensuring every component meets and preferably exceeds all regulatory standards from day one.
Ready to build a smarter, more efficient hospital? Cleffex Digital Ltd develops secure, compliant, AI-driven solutions tailored to the unique challenges of the Canadian healthcare sector. Find out how we can be your technology partner at Cleffex.com.