Think of AI-assisted clinical decision support (CDSS) as an intelligent co-pilot for healthcare professionals. It doesn't fly the plane, but it provides the critical data and alerts needed to navigate complex situations, augmenting a clinician's own expertise with powerful insights right at the point of care.
Unlocking Smarter Healthcare Decisions with AI
At its heart, an AI-assisted CDSS sifts through mountains of patient data, everything from electronic health records and lab results to medical imaging. It's designed to spot the subtle patterns and predict potential risks that the human eye might miss, especially during a hectic shift.
This technology acts as a vigilant partner, helping doctors and nurses make faster, more informed, and more accurate decisions that ultimately lead to better patient outcomes. The whole point is to move clinical workflows from being reactive to proactive. Instead of just responding after a patient's condition worsens, these systems can forecast the risk of an event like sepsis or acute kidney injury, giving care teams a crucial window to intervene.
The Role of an Intelligent Co-Pilot
Imagine a system that can instantly cross-reference a patient's unique symptoms and genetic markers with a secure database of thousands of similar cases. That’s the real power of an AI-assisted CDSS. It offers an analytical depth that’s simply beyond human capacity, especially under the intense time pressures of a clinic or hospital. We explore the nuts and bolts of building these systems in our guide to AI-powered healthcare solutions.
This capability is fundamental to delivering truly personalised treatment plans. The system can help clinicians find answers to critical questions on the fly:
Which medication is most likely to be effective for this patient's specific profile?
Is this individual at a high risk for a post-operative complication?
Are there any subtle anomalies in this CT scan that warrant a closer look?
When these insights are embedded smoothly into existing clinical workflows, a well-designed CDSS becomes an indispensable part of modern medicine. It empowers healthcare providers by turning a flood of raw data into clear, actionable intelligence.
How an AI-Powered CDSS Actually Works
So, how does an AI-assisted clinical decision support system really operate? To get a clear picture, we need to look under the hood. At its heart, the system runs on three core components working together: high-quality data, sophisticated analytical models, and deep integration into the clinical workflow. Each piece is vital for turning a flood of information into sharp, usable clinical intelligence.
It all starts with data. This is the fuel for the entire system, but it’s not just one type of information. We're talking about a rich mix of patient inputs, from structured data like lab results and electronic health record (EHR) entries to unstructured sources like doctors' notes, pathology reports, and even diagnostic images like X-rays. The quality and diversity of this data are everything – the better the input, the more reliable the output.
The Brains of the Operation: The AI Models
Once the data is collected, the real magic happens. This is where advanced machine learning and deep learning models take over. Imagine these models as expert digital researchers, tirelessly combing through massive datasets to spot hidden connections and predict outcomes. An algorithm might, for instance, learn to recognise the earliest, faintest signs of sepsis by analysing vital signs from thousands of patients, picking up on patterns a human simply couldn't see in real-time.
This analytical engine is what puts the "intelligence" in AI-CDSS. These aren't just rigid, rule-based systems; they actually learn and adapt as they encounter more data. This dynamic ability allows them to offer tailored recommendations based on a specific patient's situation, going far beyond the generic alerts of the past. The technical architecture behind these systems is a complex subject, something we explore further when discussing AI in medical software development.
From Insight to Action: Seamless Integration
All that brilliant analysis is worthless if it doesn't get to the right person at the right time. The true value of an AI-assisted clinical decision support system comes from its seamless integration into a clinician's day-to-day work, usually right inside the EHR.
The goal is to make the technology feel like a natural extension of the clinician's own expertise, not another screen to check or system to log into. A well-integrated AI-CDSS provides alerts, risk scores, and recommendations as a seamless part of the patient care process.
For example, a warning about a patient's high risk for acute kidney injury might appear directly on their chart just as the physician is reviewing their latest lab results. This kind of immediate, context-aware guidance is what elevates an analytical tool into a genuine co-pilot for clinical practice.
This concept map shows the entire process, from gathering patient data to generating actionable clinical insights.
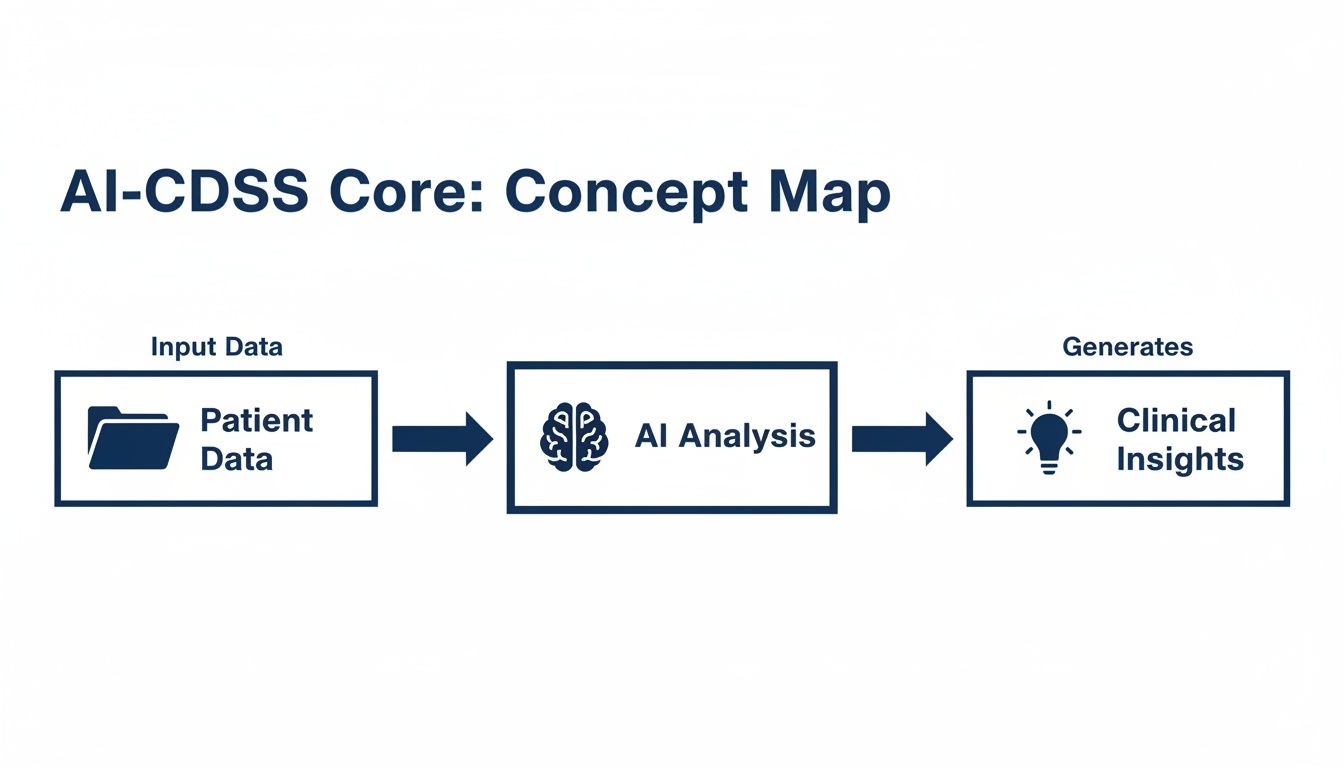
As you can see, each step builds on the one before it. Without a solid foundation of comprehensive data and intelligent models, the insights delivered to clinicians would be incomplete. This tight coupling of data, analysis, and workflow is what creates a powerful tool that truly supports clinicians and improves patient care.
Putting AI-CDSS Into Practice in Healthcare
It's one thing to talk about AI-assisted clinical decision support in theory, but where is it actually showing up on the clinic floor? This isn't science fiction anymore. These tools are already making a real difference in how care is delivered across dozens of medical specialities.

The core idea is simple: give clinicians sharper insights from the data they’re already collecting. This is happening right now to improve how we diagnose diseases, create personalised treatment plans, and even get ahead of problems before they start. The end goals are always better patient outcomes and smarter, more efficient workflows.
Enhancing Diagnostic Accuracy
Think of AI algorithms as a powerful partner for specialists, especially in diagnostics. These systems are brilliant at sifting through complex medical images, like MRIs and CT scans, to flag subtle patterns that might signal an early-stage malignancy.
This doesn’t mean the AI replaces the radiologist. Far from it. It acts as a second set of highly trained eyes, highlighting areas of concern that warrant a closer look. This kind of backup helps catch cancers earlier and more precisely, which can be the deciding factor in a successful treatment.
Creating Personalised Treatment Plans
One of the most exciting applications for AI-assisted clinical decision support is in crafting treatment plans that are unique to each patient. These systems can look at a person’s genetic markers, clinical history, lab results, and even lifestyle data to suggest the most effective course of action.
We’re finally moving past the one-size-fits-all model of medicine. For instance, an oncologist could use an AI tool to see which chemotherapy regimen is most likely to work for a patient with a specific tumour profile, basing that recommendation on the outcomes of thousands of similar cases. For a closer look at how AI support tools are being used on the ground, platforms like the SupportGPT platform offer some great examples.
By making sense of incredibly complex datasets, AI-CDSS gives clinicians the ability to tailor treatments directly to the individual. This not only improves how well a therapy works but can also reduce nasty side effects. It’s a huge step toward truly patient-centred care.
This is especially valuable for managing chronic conditions, where care plans need to be adjusted over the long haul. Having the right support tools can make all the difference.
Enabling Proactive and Preventive Care
Perhaps the biggest shift AI-CDSS brings to the table is the move from reactive to proactive care. Instead of waiting for a health crisis to happen, these systems can monitor patient data in real time to spot individuals at high risk for a serious event.
This is a massive deal here in Canada, where managing long-term health is a major priority. Consider this: recent data from Statistics Canada showed that in 2021, over 45 per cent of Canadians were living with at least one major chronic disease. That sheer volume of conditions like chronic kidney disease and hypertension means we urgently need systems that can flag high-risk individuals in large populations.
AI models can now predict the likelihood of sepsis or acute kidney injury hours or even days before obvious symptoms appear. That gives clinicians a critical window to step in and prevent a crisis, which is better for the patient and helps lower the cost of care. We dive much deeper into this in our guide to AI-driven EHR solutions for modern healthcare.
These real-world examples show that AI-CDSS isn't just an abstract idea. It's a practical toolkit that is already making healthcare better and more efficient.
Balancing the Promise and Pitfalls of AI in the Clinic
Bringing AI-assisted clinical decision support into the clinic holds incredible promise, but it’s not a magic wand. Think of it like any other advanced instrument in a hospital; it's a powerful tool that requires a clear-eyed view of both the rewards and the responsibilities. The benefits are genuinely compelling, but they have to be carefully weighed against the inherent risks.
The upside is massive. These systems can sharpen diagnostic accuracy, cut down on medical errors, and make clinical workflows much smoother. By taking over routine data analysis, AI-CDSS frees up clinicians to focus on what truly matters: direct patient care, complex problem-solving, and the human side of medicine.
But getting there means navigating the potential downsides. Rolling out this technology successfully demands a solid governance framework and a firm grasp of regulatory compliance to keep both patients and the organisation safe.
The Major Benefits of AI-CDSS
One of the first things you’ll notice is a real boost in clinical efficiency and accuracy. By flagging potential issues early and serving up the right data at the right time, these systems help ease the cognitive load on physicians and nurses.
Beyond the day-to-day, the economic impact could be huge for Canada's healthcare system. A McKinsey analysis suggests that a full-scale deployment could lower net healthcare spending by 4.5% to 8.0% each year. That translates to a potential net savings of CA $14 billion to CA $26 billion annually. You can dig deeper into the potential benefits of AI for healthcare in Canada to see the full picture.
Understanding and Mitigating the Risks
Of course, introducing powerful AI into healthcare settings comes with serious considerations that need to be tackled head-on. Patient data privacy is non-negotiable, and any system must comply with strict regulations like PHIPA. Then there’s the very real risk of algorithmic bias, where a model trained on unrepresentative data ends up reinforcing or even worsening existing health disparities.
The goal is always to enhance clinical judgment, never to replace it. The clinician must remain in control, using the AI's output as just one piece of the puzzle in their expert decision-making. This "human-in-the-loop" approach is the bedrock of safe and ethical AI in medicine.
The following table breaks down how to think about these trade-offs, pairing the major benefits with the associated risks and outlining practical ways to manage them.
Benefits of AI-CDSS and Strategies for Risk Mitigation
| Key Benefit | Potential Risk | Mitigation Strategy |
|---|---|---|
| Enhanced Diagnostic Accuracy | Misdiagnosis from flawed AI models or over-reliance on technology. | Implement a "human-in-the-loop" model, requiring clinician validation. Perform continuous model monitoring and regular performance audits. |
| Improved Clinical Efficiency | Workflow disruptions and alert fatigue if the system is poorly integrated. | Design user-centred interfaces with input from clinicians. Use intelligent alert filtering and ensure seamless EMR integration. |
| Reduced Healthcare Costs | High initial investment and ongoing maintenance costs with uncertain ROI. | Start with pilot projects focused on high-impact use cases. Conduct a thorough cost-benefit analysis before full-scale deployment. |
| Personalised Treatment Plans | Algorithmic bias leading to inequitable care for underrepresented patient groups. | Train and validate models on diverse, representative datasets. Implement fairness metrics and conduct regular bias audits. |
| Proactive Risk Identification | Patient data privacy breaches and non-compliance with regulations like PHIPA. | Employ robust data encryption, access controls, and anonymisation techniques. Ensure full compliance with all healthcare data protection laws. |
Managing these challenges effectively is all about having a clear strategy. This means rigorous model validation, ongoing performance monitoring, and being transparent with both staff and patients about how the technology works.
Partnering with an experienced software development company that truly understands these nuances is crucial. A team with a proven track record in custom healthcare software development can architect systems that maximise the upsides while building in the necessary safeguards. By taking a proactive approach, healthcare providers can ensure their healthcare software solutions are safe, effective, and ready to pave the way for a more data-informed future in patient care.
A Practical Roadmap for Implementing AI-CDSS
Bringing AI-assisted clinical decision support into a hospital or clinic isn't just about plugging in a new piece of software. It’s a carefully managed journey that blends change management, deep technical work, and a commitment to getting it right for the people on the front lines. The real goal is to build a tool that clinicians actually trust and that shows its value from the moment it goes live.
This journey doesn't start with code; it starts with a conversation about a real clinical need. You have to pinpoint a specific, high-impact area where AI can make a genuine difference; maybe it’s cutting down diagnostic wait times for time-sensitive conditions or lowering the readmission rates for patients with chronic diseases.
Starting small and focused is the key. It helps you get that crucial initial buy-in from staff and demonstrates a tangible return on investment much faster, which builds the momentum you need for wider adoption down the road.
Defining the Scope and Securing Buy-In
Once you’ve zeroed in on a use case, getting clinicians on board is your single most important task. Your medical staff need to be part of the conversation from the very beginning, helping to shape the design and test the system. Their real-world insights are what will make the tool a helpful co-pilot instead of another frustrating hurdle in their day.
When you bring stakeholders in early, you're not just asking for their opinion; you're building a sense of shared ownership. This collaborative spirit is what ensures the final product fits naturally into existing clinical workflows and solves the problems that practitioners actually face.
And the demand for these tools is only growing. In Canada alone, the clinical decision support systems market was worth USD 311.1 million in 2023 and is expected to climb to USD 793.9 million by 2030. That’s a powerful signal of where the industry is heading. You can discover more insights about the Canadian CDSS market on grandviewresearch.com.
Integration and Phased Rollout
Let's be clear: seamless integration with your existing IT systems, especially the Electronic Health Record (EHR), is non-negotiable. An AI-CDSS that lives in its own little world, forcing doctors and nurses to juggle multiple screens, is doomed to fail. The insights it provides have to appear right where clinicians are already working, without breaking their concentration.
The smartest way forward is a phased rollout, starting with a controlled pilot project. This approach lets your implementation team gather honest, real-world feedback, spot challenges you couldn't have predicted, and fine-tune everything before you attempt a full-scale deployment.
A pilot program is your crucial testing ground. It’s your chance to refine the AI models, tweak the user interface based on what clinicians tell you, and measure the system's impact on a small scale. This minimises risk and builds confidence for the big launch.
This kind of methodical planning is absolutely essential for navigating the complex world of healthcare technology projects.
Key Implementation Steps
A successful implementation doesn't happen by accident; it follows a clear, structured path. Here are the core stages that should guide your project from concept to reality:
Identify a High-Value Problem: Start by finding a specific clinical challenge where AI can deliver obvious and measurable benefits.
Assemble a Cross-Functional Team: Bring everyone to the table: clinicians, IT specialists, data scientists, and administrators, to make sure all perspectives are heard.
Ensure Data Readiness: Take a hard look at the quality, accessibility, and security of the data you'll need to train and run the AI models, ensuring full compliance with standards like PHIPA.
Develop and Validate the AI Model: Whether you build or buy, the AI model must be rigorously validated against trusted clinical benchmarks before it ever touches a real patient workflow.
Pilot and Iterate: Launch a limited pilot to test the system in the wild. Collect user feedback and be ready to make adjustments.
Train and Support Users: Provide thorough training for all clinical staff and have ongoing support in place to help them become proficient and confident users.
Monitor and Evaluate: Once live, continuously monitor the system's performance. Keep a close eye on your key metrics and evaluate their long-term impact on patient outcomes and clinic efficiency.
Following these steps turns a daunting project into a manageable process. As we explored in our end-to-end software development guide, this kind of strategic planning is the bedrock for delivering technology that truly solves problems and gets used for years to come.
Looking Ahead: Building Data-Driven Healthcare
AI-assisted clinical decision support isn't some far-off idea from a sci-fi movie; it's here now, actively helping clinicians improve patient care. Think of it as an intelligent partner, one that helps deliver more personalised, efficient, and safer medicine. It provides deeper insights, automates the tedious parts of analysis, and ultimately helps doctors get ahead of problems before they become critical.
Moving forward, the real progress will come from strong collaborations between healthcare leaders and technology experts. This partnership is what will truly build the next generation of healthcare, turning mountains of data into clear, actionable intelligence that saves lives.
The Foundation of Any Smart System
To build this future, you need a rock-solid foundation. That starts with specialised healthcare data engineering. This discipline is all about making sure the data that feeds the AI is clean, secure, and properly structured. Without this crucial first step, even the most sophisticated algorithm is useless – garbage in, garbage out.
This means building resilient data pipelines, getting different systems to talk to each other, and staying on the right side of privacy laws like PHIPA. A well-designed data infrastructure is the bedrock for any successful AI-assisted clinical decision support tool. It's not the glamorous part, but it's absolutely essential.
Finding the Right Partner for a Complex Field
Getting this right takes more than just good technology; it demands a real understanding of how hospitals actually work and the principles of solid software engineering. This is why choosing the right partner is so important. A skilled software development company that lives and breathes healthcare can guide you through the entire process, from hashing out the initial idea to implementation and support.
Success comes from a true collaboration that marries clinical expertise with technical skill. The aim is to create tools that aren't just powerful, but are also practical and intuitive for the clinicians who will use them every single day.
A strong partnership ensures the final product solves a genuine clinical problem and fits neatly into existing workflows. It’s all about building tools that doctors and nurses can trust. Firms that focus on custom healthcare software development are prepared for the unique challenges of the sector and can deliver secure, effective healthcare software solutions. The path to a data-driven future is a team effort, and we invite you to learn more about our mission.
Questions We Often Hear About AI-CDSS
As AI-assisted clinical decision support finds its way into more hospitals and clinics, a lot of good questions come up. We've gathered some of the most common ones here to give you straightforward answers about what this technology is, what it does, and how to get started.
How Is AI-CDSS Different from the Clinical Alerts We Already Have?
Think of traditional clinical decision support as a simple checklist. It's great at following fixed rules, like an "if-this-then-that" command. For example, it will flag a drug allergy if it's already documented in a patient's chart. It’s a necessary safety net, but it only knows what you’ve explicitly told it to look for.
AI-assisted clinical decision support, on the other hand, is more like an experienced consultant. It learns from massive amounts of data, spotting subtle patterns that a human or a simple rule would miss. Instead of just flagging a known allergy, an AI model could predict a patient's likely response to a specific chemotherapy drug by analysing the outcomes of thousands of similar patients. It’s predictive, not just reactive.
Can This Actually Work with Our Existing EHR System?
Yes, and frankly, it has to. The whole point of an effective AI-CDSS is to slide intelligent insights directly into a clinician's existing workflow. It can't be another clunky, standalone application that doctors have to switch to.
A successful implementation means the recommendations and alerts appear right inside your Electronic Health Record (EHR) interface, exactly when and where they're needed most. Making this integration seamless is a non-negotiable part of any project, ensuring the tool helps rather than hinders. It's a key principle behind our custom healthcare software development.
What's the First Step for a Hospital Wanting to Get Started?
Start small, but aim for high impact. Don't try to boil the ocean by "implementing AI." Instead, pick one specific, pressing clinical problem you want to address. Maybe it's reducing sepsis mortality rates in the ICU or improving the accuracy of radiological reads for certain types of scans.
Once you have that clear goal, you need to look at your data. Do you have the clean, reliable data needed to train a smart model? If you do, the best way forward is to launch a focused pilot project. This approach, as we explored in our end-to-end software development guide, lets you prove the tool's value quickly and get crucial feedback from the clinicians who will actually be using it.
Cleffex is a software development company that builds powerful healthcare software solutions that drive modern medicine forward. Learn more about our mission and expertise on our about us page.







